Volume 10, Issue 3 (2022)
Health Educ Health Promot 2022, 10(3): 525-530 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghodrati Torbati A, Eshaghzadeh M, Imeni M, Abbaspour S. The Effects of Educational Intervention based on Dialectical Behavior Therapy on Emotional Regulation and Self-control after Discharge in Patients with COVID-19. Health Educ Health Promot 2022; 10 (3) :525-530
URL: http://hehp.modares.ac.ir/article-5-58062-en.html
URL: http://hehp.modares.ac.ir/article-5-58062-en.html
1- Department of Nursing, School of Nursing and Midwifery, Torbat Heydariyeh University of Medical Sciences, Torbat Heydariyeh, Iran
2- Faculty of Educational Sciences and Psychology, Islamshahr Branch, Islamic Azad University, Islamshahr, Iran
2- Faculty of Educational Sciences and Psychology, Islamshahr Branch, Islamic Azad University, Islamshahr, Iran
Keywords: Dialectical Behavior Therapy [MeSH], Emotional Regulation [MeSH], Self-Control [MeSH], COVID-19 [MeSH]
Full-Text [PDF 481 kb]
(3859 Downloads)
| Abstract (HTML) (2291 Views)
Full-Text: (469 Views)
Introduction
COVID-19 is caused by a new type of coronavirus that was first reported on December 31, 2019, under the original name of the new coronavirus (CoV-2019) in Wuhan, China, and has since become a pandemic with far-reaching economic, social, and health consequences [1]. This pandemic can have far-reaching consequences for individuals [2].
One of the most important causes of anxiety in COVID-19 is the inability to regulate emotion during threatening and anxious situations. Psychologists define emotion regulation as the process of initiating and maintaining a person's emotions [3]. Emotion regulation, especially in cognitive reassessment, plays an important role in anxiety disorders [4]. Research evidence shows that emotion regulation is not only associated with increased health and psychological and social benefits but can also help people manage many work-related challenges [5]. Recognizing and understanding the power of emotion regulation is very important in the face of coronavirus disease [6]. Emotion regulation can provide better emotional control in difficult situations [7].
Another factor related to mental health and symptoms of people with respiratory disease is self-control [8]. The ability to manage and have self-control plays an important role in maintaining sustainable social relationships and well-being. One of the factors that are effective in controlling the disease and its symptoms is self-control or a source of health control [9] which indicates that people can consider external control as a source for behaviors and events and give responsibility for behaviors to the chance and environment or they can consider the behavior factor as an internal source and take responsibility for the behavior and consider themselves as an important factor in behaviors and behavioral consequences, each of which has negative and positive consequences [10]. Belief in self-control is associated with psychological well-being; people who have a source of internal control try to control events and behaviors and create a sense of self-control and positive effectiveness [11]. Therefore, it is clear that the simultaneous emergence of psychological disorders in patients with respiratory diseases is important from both diagnostic and quality of life perspectives. Generally, treatment of psychological disorders in these patients reduces the number of attacks and improves respiratory performance [12]. Several studies showed that psychotherapy techniques are successful in improving respiratory symptoms as well as depression, anxiety, and stress [13-15]. Dialectical behavioral therapy is one of these techniques.
Dialectical behavioral therapy was developed by Linhan in the 1970s to treat women with borderline personality disorder with suicidal ideation, suicidal act, and chronic self-harming behaviors. It was then revised in 1993, and this new method was successfully used to regulate the emotions of people with borderline personality disorder [16]. This approach is based on the four components of mindfulness and distress tolerance as components of acceptance and regulation of emotion and interpersonal efficiency as components of change [17]. The goal of dialectical behavior therapy is to reduce the suffering of people involved in emotional regulation problems such as lack of self-control and anxiety [18].
One of the skills of dialectical behavior therapy is emotion regulation skills. Emotional regulation means the ability of individuals to influence the type, time, and manner of self-control and emotional regulation as well as changing the duration or intensity of behavioral processes and are done consciously or unconsciously through the use of emotion regulation strategies [19]. Emotional dysregulation can be a prelude to the onset of mental disorders such as depression and lack of self-control over a person's thoughts and behavior, which has been confirmed in previous studies [20].
The spread of coronary heart disease has confused and, by altering people's living conditions, has had devastating psychological effects, including a lack of self-control and a lack of emotion regulation. In addition, the epidemic crisis can cause negative psychological and social effects that in some way affect the mental health of people in society. Therefore, this study aimed to evaluate the effectiveness of dialectical therapy on emotional regulation and self-control in COVID-19 patients after hospital discharge.
Material & Methods
It was a quasi-experimental pre-test post-test study with a control group conducted in Torbat Heydariyeh, Iran. The study included all men who had passed the hospital quarantine period for COVID-19 which was 14 days after their discharge from the hospital. Before starting the intervention, the necessary explanations were given to the individuals about the objectives of the research, and after obtaining their informed consent, the individuals entered the project. The statistical sample consisted of 30 people (15 people in each group) and was determined based on similar studies [21, 22]. The available sampling method was used and inclusion and exclusion criteria were used for the random assignment of individuals in the experimental and control groups. Inclusion criteria were: male, minimum age 20, maximum 40 years, no history of chronic mental illness, no use of sedatives, and patients with COVID-19 who have been discharged for 14 days. Exclusion criteria also included absence from more than two sessions in training sessions, dissatisfaction, and cooperation of individuals and failure to perform the tasks specified in the training process, and recurrence of the disease.
At the beginning of the study, both groups were pre-tested by the Tanji self-control questionnaire [23] and the Garnofsky emotional regulation questionnaire [24].
Tanji self-control questionnaire: It has 36 items and its purpose is to measure the extent of people's control over themselves. It is a 5-point Likert scale (1=never and 5=very high) questionnaire. To get the total score of the questionnaire, the total scores of all questions are added together. The maximum score for the Tanji self-control questionnaire is 180 and the minimum is 36. A high score indicates more self-control and a low score indicates less self-control. The validity of this scale has been confirmed by assessing its correlation with the scales of academic achievement, adjustment, positive relationships, and interpersonal skills. Also, its reliability was obtained on two statistical samples using Cronbach's alpha test of 0.83 and 0.85 [23]. The validity and reliability of the Persian version of the Tanji self-control questionnaire have been calculated and confirmed by Mousavi Moghadam et al. [25].
Emotion Regulation Questionnaire: Compiled by Granefski, it is a self-report tool that has 36 items. The range of scores on the scale is from 1 (almost never) to 5 (almost always). Each subscale consists of 4 items and the total score is obtained from the sum of the subscales. The 5-Likert point is used in the form of 1 (never), 2 (rarely), 3 (sometimes), 4 (often), and 5 (always). The interpretation of the questionnaire is that a score between 36 to 72 indicates poor emotional cognitive regulation, a score between 72 to 108 indicates moderate emotional cognitive regulation and a score above 108 indicates strong emotional cognitive regulation in individuals. The alpha coefficient for the subscales of this questionnaire has been reported by Garanfsky et al. in the range of 0.71 to 0.81 [25]. Hasani et al. obtained the reliability of the Persian version of the questionnaire by Cronbach's alpha method of 92% [26].
It was approved by the ethics committee of Torbat Heydariyeh University of Medical Sciences and was set according to the STROBE guidelines. The dialectical behavior therapy intervention was performed on the experimental group in 10 sessions of 90 minutes (two sessions per week) in the form of face-to-face sessions concerning social distance and the use of personal protective equipment. The control group was on the waiting list during the treatment intervention. The post-test was taken from both groups after the last treatment session. After the end of the study, dialectical behavior therapy training was held in the form of face-to-face sessions for the control group, observing social distance and using personal protective equipment. The content of treatment sessions is reported in Table 1.
The collected data were analyzed using SPSS software version 21 and multivariate analysis of covariance.
Table 1) Content of dialectical behavior therapy sessions

Findings
The demographic variables of the experimental and control groups are presented in Table 2. The results of the Chi-square test showed that there was no significant difference between the two groups in terms of age, marital status, occupation, and level of education and the groups were homogeneous (p>0.05).
The mean and standard deviation of emotional regulation and self-control scores by pre-test and post-test in both experimental and control groups are shown in Table 3.
Multivariate analysis of covariance to compare experimental and control groups in dependent variables is also presented in Tables 4 and 5. In this study, multivariate analysis of covariance was used for the inferential analysis of the results. First, the required assumptions were examined.
In this study, the assumptions of normality of distribution, homogeneity of variances, and equality of covariances were investigated. The results of the Kolmogorov-Smirnov test showed that the distribution was normal (p>0.05). Levene test results in the emotional regulation variable (p=0.145, F=2.243) and self-control (p=0.324, F=1.007) showed that the presumption of equality of variance was confirmed in all research variables. Based on the box test results (p=0.467, F=0.970, Mbox=11.498), the assumption of the equality of covariance was accepted.
Table 2) Descriptive statistics of demographic variables
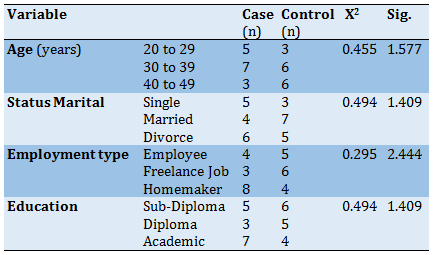
Table 3) Mean±SD results of dependent variables in the two groups

There was a significant difference between the experimental and control groups in post-test scores in the variables of emotional regulation and self-control and the amount of this difference was 0.78 (p<0.05), i.e. 78% of individual differences in variables are related to differences between groups.
By eliminating the effect of pre-test scores, the difference between the mean of post-test scores in the variables of emotional regulation and self-control in the experimental and control groups was significant (p<0.05). The effect of this treatment on increasing the emotional regulation score was 27% and on increasing the self-control score was 15%.
Discussion
This study aimed at evaluating the effectiveness of dialectical therapy on emotional regulation and self-control in COVID-19 patients after hospital discharge. The results showed that dialectical therapy increased the score of emotional regulation. This finding was consistent with the findings of China's research on the effect of teaching dialectical behavior therapy skills to solve adolescents' emotional problems [1]. Rady et al. also showed the effect of dialectical behavior therapy on emotion regulation disorder in couples and both sexes made significant improvements in emotion regulation and marital adjustment scores [27]. Pasieczny & Connor showed that dialectical behavior therapy significantly improves mental health and its components and improves emotions [28]. The results of a study also showed the effectiveness of dialectical behavior therapy on executive performance, emotional control, and symptom severity in patients with bipolar disorder in the intervention group [29].
Dialectical behavior therapy is based on the premise of improving skills and applying them through positive emotional regulation. Emotional regulation is the process by which individuals regulate their emotions in response to conscious environmental changes and changes that are subconscious, and improve emotional disorder and functional impairment of emotions [30].
Dialectical behavior therapy skills target the difficulty of regulating emotions, which is one of the early signs of mood instability. At the core of dialectical behavior therapy are mindfulness and emotional regulation skills that teach people to accept things without judgment, deal with emotions, and act against strong emotional desires. Emotional instability damages communication, and in this context, training effective interpersonal skills help individuals to rebuild past damaged relationships and learn negotiation techniques for resolving conflict [31]. Interpersonal skills training identifies communication styles and the fit between one's desires and those of others and identifies problems in interpersonal relationships. The principle of acceptance helps to accept emotions and the principle of change helps to change emotions. As a result, dialectical behavior therapy, through its therapeutic mechanisms, reduces irrational beliefs and improves emotional regulation in individuals [32].
The other findings of the study showed the effect of this treatment on increasing self-control scores. This finding was consistent with the findings of Robison & Luczakowsky. They found that dialectical behavior therapy reduced self-destructive behaviors, improved self-control, impaired identity and low self-esteem problems, and improved problems with social skills in individuals [33]. Ghodrati et al. also showed that dialectical behavior therapy and compassion therapy can increase self-control and decrease blood cortisol levels [22]. Tavakoli et al. also showed that adherence to dialectical behavior therapy and self-care behavior increased significantly in the experimental group compared to the control group and dialectical behavior therapy affected self-care and adherence to treatment in patients [34]. Dialectical behavior therapy is used in people who have negative emotions and lack self-control, and clinicians are asked to help the client understand disturbing behaviors to solve the problem, and this is one of the reasons that dialectical behavior therapy has been effective in strengthening self-control behaviors [35]. People with physical illnesses are known, above all, for not regulating negative emotions and lacking self-control, and for being cognitively disturbed. In addition, they show a lack of positive self-control, which causes irrational and superficial arousal and they cannot have pre-planned behaviors. Therefore, it can be concluded that one of the reasons for the success of dialectical behavior therapy in the mentioned studies is the reduction of suffering of people involved in problems of lack of self-control that dialectical behavior therapy skills have improved self-control in individuals [36].
One of the limitations of the present study was that the statistical population was limited to the population studied in this study and patients are not isolated in terms of disease severity. The next limitation was holding face-to-face training sessions for the experimental group despite the social distance and the use of personal protective equipment, there was still the possibility of contact with the COVID-19 virus, which is suggested to be considered in future research.
Conclusion
The results of this study showed that dialectical behavior therapy can increase cognitive regulation and improve self-control in patients with the COVID-19 virus. Therefore, to prevent further psychological consequences caused by this virus, it is recommended to use this intervention in designing treatment programs for psychological centers, comprehensive health service centers, counselors, clinical psychologists, and therapists.
Acknowledgments: The authors thank all relevant officials and all participants for participating in the research project.
Ethical Permissions: The study was approved by the Vice Chancellor for Research and Technology of Torbat Heydariyeh University of Medical Sciences with the code of ethics committee IR.THUMS.REC.1400.001.
Conflicts of Interests: This article is the result of a research project.
Authors’ Contributions: Ghodrati Torbati A (First Author), Methodologist/Main Researcher (25%); Eshaghzadeh M (Second Author), Introduction Writer/Assistant Researcher (25%); Imeni M (Third Author), Statistical Analyst (25%); Abbaspour S (Forth author), Discussion writer (25%)
Funding/Support: None declared.
COVID-19 is caused by a new type of coronavirus that was first reported on December 31, 2019, under the original name of the new coronavirus (CoV-2019) in Wuhan, China, and has since become a pandemic with far-reaching economic, social, and health consequences [1]. This pandemic can have far-reaching consequences for individuals [2].
One of the most important causes of anxiety in COVID-19 is the inability to regulate emotion during threatening and anxious situations. Psychologists define emotion regulation as the process of initiating and maintaining a person's emotions [3]. Emotion regulation, especially in cognitive reassessment, plays an important role in anxiety disorders [4]. Research evidence shows that emotion regulation is not only associated with increased health and psychological and social benefits but can also help people manage many work-related challenges [5]. Recognizing and understanding the power of emotion regulation is very important in the face of coronavirus disease [6]. Emotion regulation can provide better emotional control in difficult situations [7].
Another factor related to mental health and symptoms of people with respiratory disease is self-control [8]. The ability to manage and have self-control plays an important role in maintaining sustainable social relationships and well-being. One of the factors that are effective in controlling the disease and its symptoms is self-control or a source of health control [9] which indicates that people can consider external control as a source for behaviors and events and give responsibility for behaviors to the chance and environment or they can consider the behavior factor as an internal source and take responsibility for the behavior and consider themselves as an important factor in behaviors and behavioral consequences, each of which has negative and positive consequences [10]. Belief in self-control is associated with psychological well-being; people who have a source of internal control try to control events and behaviors and create a sense of self-control and positive effectiveness [11]. Therefore, it is clear that the simultaneous emergence of psychological disorders in patients with respiratory diseases is important from both diagnostic and quality of life perspectives. Generally, treatment of psychological disorders in these patients reduces the number of attacks and improves respiratory performance [12]. Several studies showed that psychotherapy techniques are successful in improving respiratory symptoms as well as depression, anxiety, and stress [13-15]. Dialectical behavioral therapy is one of these techniques.
Dialectical behavioral therapy was developed by Linhan in the 1970s to treat women with borderline personality disorder with suicidal ideation, suicidal act, and chronic self-harming behaviors. It was then revised in 1993, and this new method was successfully used to regulate the emotions of people with borderline personality disorder [16]. This approach is based on the four components of mindfulness and distress tolerance as components of acceptance and regulation of emotion and interpersonal efficiency as components of change [17]. The goal of dialectical behavior therapy is to reduce the suffering of people involved in emotional regulation problems such as lack of self-control and anxiety [18].
One of the skills of dialectical behavior therapy is emotion regulation skills. Emotional regulation means the ability of individuals to influence the type, time, and manner of self-control and emotional regulation as well as changing the duration or intensity of behavioral processes and are done consciously or unconsciously through the use of emotion regulation strategies [19]. Emotional dysregulation can be a prelude to the onset of mental disorders such as depression and lack of self-control over a person's thoughts and behavior, which has been confirmed in previous studies [20].
The spread of coronary heart disease has confused and, by altering people's living conditions, has had devastating psychological effects, including a lack of self-control and a lack of emotion regulation. In addition, the epidemic crisis can cause negative psychological and social effects that in some way affect the mental health of people in society. Therefore, this study aimed to evaluate the effectiveness of dialectical therapy on emotional regulation and self-control in COVID-19 patients after hospital discharge.
Material & Methods
It was a quasi-experimental pre-test post-test study with a control group conducted in Torbat Heydariyeh, Iran. The study included all men who had passed the hospital quarantine period for COVID-19 which was 14 days after their discharge from the hospital. Before starting the intervention, the necessary explanations were given to the individuals about the objectives of the research, and after obtaining their informed consent, the individuals entered the project. The statistical sample consisted of 30 people (15 people in each group) and was determined based on similar studies [21, 22]. The available sampling method was used and inclusion and exclusion criteria were used for the random assignment of individuals in the experimental and control groups. Inclusion criteria were: male, minimum age 20, maximum 40 years, no history of chronic mental illness, no use of sedatives, and patients with COVID-19 who have been discharged for 14 days. Exclusion criteria also included absence from more than two sessions in training sessions, dissatisfaction, and cooperation of individuals and failure to perform the tasks specified in the training process, and recurrence of the disease.
At the beginning of the study, both groups were pre-tested by the Tanji self-control questionnaire [23] and the Garnofsky emotional regulation questionnaire [24].
Tanji self-control questionnaire: It has 36 items and its purpose is to measure the extent of people's control over themselves. It is a 5-point Likert scale (1=never and 5=very high) questionnaire. To get the total score of the questionnaire, the total scores of all questions are added together. The maximum score for the Tanji self-control questionnaire is 180 and the minimum is 36. A high score indicates more self-control and a low score indicates less self-control. The validity of this scale has been confirmed by assessing its correlation with the scales of academic achievement, adjustment, positive relationships, and interpersonal skills. Also, its reliability was obtained on two statistical samples using Cronbach's alpha test of 0.83 and 0.85 [23]. The validity and reliability of the Persian version of the Tanji self-control questionnaire have been calculated and confirmed by Mousavi Moghadam et al. [25].
Emotion Regulation Questionnaire: Compiled by Granefski, it is a self-report tool that has 36 items. The range of scores on the scale is from 1 (almost never) to 5 (almost always). Each subscale consists of 4 items and the total score is obtained from the sum of the subscales. The 5-Likert point is used in the form of 1 (never), 2 (rarely), 3 (sometimes), 4 (often), and 5 (always). The interpretation of the questionnaire is that a score between 36 to 72 indicates poor emotional cognitive regulation, a score between 72 to 108 indicates moderate emotional cognitive regulation and a score above 108 indicates strong emotional cognitive regulation in individuals. The alpha coefficient for the subscales of this questionnaire has been reported by Garanfsky et al. in the range of 0.71 to 0.81 [25]. Hasani et al. obtained the reliability of the Persian version of the questionnaire by Cronbach's alpha method of 92% [26].
It was approved by the ethics committee of Torbat Heydariyeh University of Medical Sciences and was set according to the STROBE guidelines. The dialectical behavior therapy intervention was performed on the experimental group in 10 sessions of 90 minutes (two sessions per week) in the form of face-to-face sessions concerning social distance and the use of personal protective equipment. The control group was on the waiting list during the treatment intervention. The post-test was taken from both groups after the last treatment session. After the end of the study, dialectical behavior therapy training was held in the form of face-to-face sessions for the control group, observing social distance and using personal protective equipment. The content of treatment sessions is reported in Table 1.
The collected data were analyzed using SPSS software version 21 and multivariate analysis of covariance.
Table 1) Content of dialectical behavior therapy sessions

Findings
The demographic variables of the experimental and control groups are presented in Table 2. The results of the Chi-square test showed that there was no significant difference between the two groups in terms of age, marital status, occupation, and level of education and the groups were homogeneous (p>0.05).
The mean and standard deviation of emotional regulation and self-control scores by pre-test and post-test in both experimental and control groups are shown in Table 3.
Multivariate analysis of covariance to compare experimental and control groups in dependent variables is also presented in Tables 4 and 5. In this study, multivariate analysis of covariance was used for the inferential analysis of the results. First, the required assumptions were examined.
In this study, the assumptions of normality of distribution, homogeneity of variances, and equality of covariances were investigated. The results of the Kolmogorov-Smirnov test showed that the distribution was normal (p>0.05). Levene test results in the emotional regulation variable (p=0.145, F=2.243) and self-control (p=0.324, F=1.007) showed that the presumption of equality of variance was confirmed in all research variables. Based on the box test results (p=0.467, F=0.970, Mbox=11.498), the assumption of the equality of covariance was accepted.
Table 2) Descriptive statistics of demographic variables
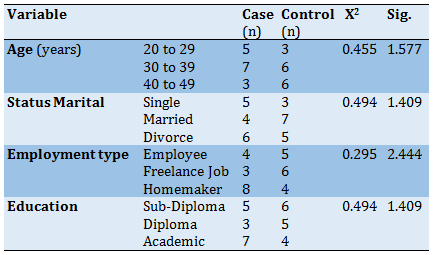
Table 3) Mean±SD results of dependent variables in the two groups

There was a significant difference between the experimental and control groups in post-test scores in the variables of emotional regulation and self-control and the amount of this difference was 0.78 (p<0.05), i.e. 78% of individual differences in variables are related to differences between groups.
By eliminating the effect of pre-test scores, the difference between the mean of post-test scores in the variables of emotional regulation and self-control in the experimental and control groups was significant (p<0.05). The effect of this treatment on increasing the emotional regulation score was 27% and on increasing the self-control score was 15%.
Discussion
This study aimed at evaluating the effectiveness of dialectical therapy on emotional regulation and self-control in COVID-19 patients after hospital discharge. The results showed that dialectical therapy increased the score of emotional regulation. This finding was consistent with the findings of China's research on the effect of teaching dialectical behavior therapy skills to solve adolescents' emotional problems [1]. Rady et al. also showed the effect of dialectical behavior therapy on emotion regulation disorder in couples and both sexes made significant improvements in emotion regulation and marital adjustment scores [27]. Pasieczny & Connor showed that dialectical behavior therapy significantly improves mental health and its components and improves emotions [28]. The results of a study also showed the effectiveness of dialectical behavior therapy on executive performance, emotional control, and symptom severity in patients with bipolar disorder in the intervention group [29].
Dialectical behavior therapy is based on the premise of improving skills and applying them through positive emotional regulation. Emotional regulation is the process by which individuals regulate their emotions in response to conscious environmental changes and changes that are subconscious, and improve emotional disorder and functional impairment of emotions [30].
Dialectical behavior therapy skills target the difficulty of regulating emotions, which is one of the early signs of mood instability. At the core of dialectical behavior therapy are mindfulness and emotional regulation skills that teach people to accept things without judgment, deal with emotions, and act against strong emotional desires. Emotional instability damages communication, and in this context, training effective interpersonal skills help individuals to rebuild past damaged relationships and learn negotiation techniques for resolving conflict [31]. Interpersonal skills training identifies communication styles and the fit between one's desires and those of others and identifies problems in interpersonal relationships. The principle of acceptance helps to accept emotions and the principle of change helps to change emotions. As a result, dialectical behavior therapy, through its therapeutic mechanisms, reduces irrational beliefs and improves emotional regulation in individuals [32].
The other findings of the study showed the effect of this treatment on increasing self-control scores. This finding was consistent with the findings of Robison & Luczakowsky. They found that dialectical behavior therapy reduced self-destructive behaviors, improved self-control, impaired identity and low self-esteem problems, and improved problems with social skills in individuals [33]. Ghodrati et al. also showed that dialectical behavior therapy and compassion therapy can increase self-control and decrease blood cortisol levels [22]. Tavakoli et al. also showed that adherence to dialectical behavior therapy and self-care behavior increased significantly in the experimental group compared to the control group and dialectical behavior therapy affected self-care and adherence to treatment in patients [34]. Dialectical behavior therapy is used in people who have negative emotions and lack self-control, and clinicians are asked to help the client understand disturbing behaviors to solve the problem, and this is one of the reasons that dialectical behavior therapy has been effective in strengthening self-control behaviors [35]. People with physical illnesses are known, above all, for not regulating negative emotions and lacking self-control, and for being cognitively disturbed. In addition, they show a lack of positive self-control, which causes irrational and superficial arousal and they cannot have pre-planned behaviors. Therefore, it can be concluded that one of the reasons for the success of dialectical behavior therapy in the mentioned studies is the reduction of suffering of people involved in problems of lack of self-control that dialectical behavior therapy skills have improved self-control in individuals [36].
One of the limitations of the present study was that the statistical population was limited to the population studied in this study and patients are not isolated in terms of disease severity. The next limitation was holding face-to-face training sessions for the experimental group despite the social distance and the use of personal protective equipment, there was still the possibility of contact with the COVID-19 virus, which is suggested to be considered in future research.
Conclusion
The results of this study showed that dialectical behavior therapy can increase cognitive regulation and improve self-control in patients with the COVID-19 virus. Therefore, to prevent further psychological consequences caused by this virus, it is recommended to use this intervention in designing treatment programs for psychological centers, comprehensive health service centers, counselors, clinical psychologists, and therapists.
Acknowledgments: The authors thank all relevant officials and all participants for participating in the research project.
Ethical Permissions: The study was approved by the Vice Chancellor for Research and Technology of Torbat Heydariyeh University of Medical Sciences with the code of ethics committee IR.THUMS.REC.1400.001.
Conflicts of Interests: This article is the result of a research project.
Authors’ Contributions: Ghodrati Torbati A (First Author), Methodologist/Main Researcher (25%); Eshaghzadeh M (Second Author), Introduction Writer/Assistant Researcher (25%); Imeni M (Third Author), Statistical Analyst (25%); Abbaspour S (Forth author), Discussion writer (25%)
Funding/Support: None declared.
Article Type: Original Research |
Subject:
Health Education and Health Behavior
Received: 2021/12/22 | Accepted: 2022/04/9 | Published: 2022/07/13
Received: 2021/12/22 | Accepted: 2022/04/9 | Published: 2022/07/13
References
1. Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. [Link] [DOI:10.1136/bmj.m408]
2. Sarmadi M, Ghodrati-Torbati A, Gazerani A, Yaghoobi H, Bakhtiari-Dovvombaygi H. Association of HIV/AIDS and COVID-19 variables: an ecological study. HIV AIDS Rev. 2021;20(2):71-7. [Link] [DOI:10.5114/hivar.2021.107233]
3. Hyland P, Shevlin M, McBride O, Murphy J, Karatzias T, Bentall RP, et al. Anxiety and depression in the Republic of Ireland during the COVID‐19 pandemic. Acta Psychiatr Scand. 2020;142(3):249-56. [Link] [DOI:10.1111/acps.13219]
4. Abbaspour S, Tajik R, Atif K, Eshghi H, Teimori G, Ghodrati-Torbati A, et al. Prevalence and correlates of mental health status among pre-hospital healthcare staff. Clin Pract Epidemiol Ment Health. 2020;16:17-23. [Link] [DOI:10.2174/1745017902016010017]
5. Iman S, Khaula A, Maryam T, Sedigheh A, Anahita Z, Gholamheidar TB, Abbas GT. Accomplices of job burnout among employees of a medical university. Rus Open Med J. 2019;8(1):105. [Link] [DOI:10.15275/rusomj.2019.0105]
6. Restubog SLD, Ocampo ACG, Wang L. Taking control amidst the chaos: emotion regulation during the COVID-19 pandemic. J Vocat Behav. 2020;119:103440. [Link] [DOI:10.1016/j.jvb.2020.103440]
7. Wills TA, Ainette MG, Stoolmiller M, Gibbons FX, Shinar O. Good self-control as a buffering agent for adolescent substance use: an investigation in early adolescence with time-varying covariates. Psychol Addict Behav. 2008;22(4):459-71. [Link] [DOI:10.1037/a0012965]
8. von Leupoldt A, Chan PYS, Esser RW, Davenport PW. Emotions and neural processing of respiratory sensations investigated with respiratory-related evoked potentials. Psychosom Med. 2013;75(3):244-52. [Link] [DOI:10.1097/PSY.0b013e31828251cf]
9. Ahmedani BK, Peterson EL, Wells KE, Rand CS, Williams LK. Asthma medication adherence: the role of God and other health locus of control factors. Ann Allergy Asthma Immunol. 2013;110(2):75-9.e2. [Link] [DOI:10.1016/j.anai.2012.11.006]
10. Culpin I, Stapinski L, Miles ÖB, Araya R, Joinson C. Exposure to socioeconomic adversity in early life and risk of depression at 18 years: the mediating role of locus of control. J Affect Disord. 2015;183:269-78. [Link] [DOI:10.1016/j.jad.2015.05.030]
11. Seyyedmoharrami I, Dehaghi BF, Abbaspour S, Zandi A, Tatari M, Teimori G, et al. The relationship between organizational climate, organizational commitment and job burnout: Case study among employees of the university of medical sciences. Open Public Health J. 2019;12(1). [Persian] [Link] [DOI:10.2174/1874944501912010094]
12. Lehrer PM, Karavidas MK, Lu SE, Feldman J, Kranitz L, Abraham S, et al. Psychological treatment of comorbid asthma and panic disorder: a pilot study. J Anxiety Disord. 2008;22(4):671-83. [Link] [DOI:10.1016/j.janxdis.2007.07.001]
13. Grover N, Kumaraiah V, Prasadrao P, D'souza G. Cognitive behavioural intervention in bronchial asthma. J Assoc Phys Ind. 2002;50:896-900. [Link]
14. Deshmukh VM, Toelle BG, Usherwood T, O'Grady B, Jenkins CR. Anxiety, panic and adult asthma: a cognitive-behavioral perspective. Respir Med. 2007;101(2):194-202. [Link] [DOI:10.1016/j.rmed.2006.05.005]
15. Sánchez-Román S, Velasco-Furlong L, Rodríguez-Carvajal R, Baranda-Sepúlveda J. Effectiveness of a cognitive-behavioural program to reduce anxiety in medically ill patients. Revista de Investigacion Clinica. 2006;58(6):540-46. [Spanish] [Link]
16. Lynch TR, Chapman AL, Rosenthal MZ, Kuo JR, Linehan MM. Mechanisms of change in dialectical behavior therapy: Theoretical and empirical observations. J Clin Psychol. 2006;62(4):459-80. [Link] [DOI:10.1002/jclp.20243]
17. Wagner AW, Rizvi SL, Harned MS. Applications of dialectical behavior therapy to the treatment of complex trauma‐related problems: When one case formulation does not fit all. J Trauma Stress. 2007;20(4):391-400. [Link] [DOI:10.1002/jts.20268]
18. Alizadeh A, Alizadeh E, Mohamadi A. Effectiveness of individual dialectical behavior therapy skills training on major depression. Iranian J Psychiatr Nurs. 2013;1(2):62-9. [Persian] [Link]
19. Chaplin TM, Cole PM, Zahn-Waxler C. Parental socialization of emotion expression: gender differences and relations to child adjustment. Emotion. 2005;5(1):80-8. [Link] [DOI:10.1037/1528-3542.5.1.80]
20. Salehi A, Baghban I, Bahrami F, Ahmadi A. The effect of emotion regulation training based on dialectical behavior therapy and gross process model on symptoms of emotional problems. Zahedan J Res Med Sci. 2012;14(2):e93581. [Link]
21. Taheri Daghiyan A, Qasemi Motlagh M, Mehdian H. The effectiveness of dialectical behavior therapy on anxiety and rumination in depressed patients. Med J Mashhad Univ Med Sci. 2019;62:264-74. [Persian] [Link]
22. Ghodrati TA, Nejat H, Toozandehjani H, Samari AA, Akbari AH. Comparing the effectiveness of dialectical behavior therapy and compassion focused therapy on blood cortisol levels and self-control in drug abusers. J Torbat Heydariyeh Univ MedSci. 2020;7(4):35-48. [Persian] [Link]
23. Tangney JP, Baumeister RF, Boone AL. High self‐control predicts good adjustment, less pathology, better grades, and interpersonal success. J Personal. 2004;72(2):271-324. [Link] [DOI:10.1111/j.0022-3506.2004.00263.x]
24. Garnefski N, Kraaij V. Cognitive emotion regulation questionnaire-development of a short 18-item version (CERQ-short). Personal Individ Differ. 2006;41(6):1045-53. [Link] [DOI:10.1016/j.paid.2006.04.010]
25. Mousavimoghadam SR, Houri S, Omidi A, Zahirikhah N. Evaluation of relationship between intellectual intelligence and self-control, and defense mechanisms in the third year of secondary school girls. Med Sci J Islam Azad Univ. 2015;25(1):59-64. [Persian] [Link]
26. Hasani J, Azad Falah P, Rasoulzade Tabatabaei K, Ashayeri H. The assessment of cognitive emotion regulation strategies according to neuroticism and extraversion personality dimensions. Adv Cogn Sci. 2009;10:1-13. [Persian] [Link]
27. Rady A, Molokhia T, Elkholy N, Abdelkarim A. The effect of dialectical behavioral therapy on emotion dysregulation in couples. Clin Pract Epidemiol Ment Health. 2021;17:121-7. [Link] [DOI:10.2174/1745017902117010121]
28. Pasieczny N, Connor J. The effectiveness of dialectical behaviour therapy in routine public mental health settings: an Australian controlled trial. Behav Res Ther. 2011;49(1):4-10. [Link] [DOI:10.1016/j.brat.2010.09.006]
29. Zargar F, Haghshenas N, Rajabi F, Tarrahi MJ. Effectiveness of dialectical behavioral therapy on executive function, emotional control and severity of symptoms in patients with bipolar I disorder. Adv Biomed Res. 2019;8:59. [Link] [DOI:10.4103/abr.abr_42_19]
30. Dixon-Gordon KL, Chapman AL, Turner BJ. A preliminary pilot study comparing dialectical behavior therapy emotion regulation skills with interpersonal effectiveness skills and a control group treatment. J Exp Psychopathol. 2015;6(4):369-88. [Link] [DOI:10.5127/jep.041714]
31. Zamani N, Ahmadi V, Ataie MV, Mirshekar S. Comparing the effectiveness of two therapeutic methods of dialectical behavior therapy and cognitive behavior therapy on the improvement of impulsive behavior in the patients suffering from major depressive disorder (MDD) showing a tendency to suicide. J Ilam Univ Med Sci. 2014;22(5):45-54. [Persian] [Link]
32. Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archi Gen Psychiatry. 1991;48(12):1060-4. [Link] [DOI:10.1001/archpsyc.1991.01810360024003]
33. Robison S, Luczakowsky N. Dialectical behavior therapy as a tool for reducing addictive behaviors and attitudes: an adolescent group review. MOJ Addict Med Ther. 2015;1(1):00005. [Link] [DOI:10.15406/mojamt.2015.01.00005]
34. Tavakoli F, Kazemi-Zahrani H, Sadeghi M. The effectiveness of dialectical behavior therapy on adherence to treatment and self-caring behavior in patients with coronary heart disease. ARYA atheroscler. 2019;15(6):281-7. [Link]
35. Soler J, Pascual JC, Tiana T, Cebrià A, Barrachina J, Campins MJ, et al. Dialectical behaviour therapy skills training compared to standard group therapy in borderline personality disorder: a 3-month randomised controlled clinical trial. Behav Res Ther. 2009;47(5):353-8. [Link] [DOI:10.1016/j.brat.2009.01.013]
36. Jamilian HR, Malekirad AA, Farhadi MF, Habibi M, Zamani N. Effectiveness of group dialectical behavior therapy (based on core distress tolerance and emotion regulation components) on expulsive anger and impulsive behaviors. Glob J Health Sci. 2014;6(7):116-23. [Link] [DOI:10.5539/gjhs.v6n7p116]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





