Volume 10, Issue 2 (2022)
Health Educ Health Promot 2022, 10(2): 377-383 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Saboohi Z, Hoseini Koukamari P, Rohani M, Rawlins J, Karimy M. Health Promoting Behaviors in Iranian Female Adolescents during the COVID-19 Pandemic. Health Educ Health Promot 2022; 10 (2) :377-383
URL: http://hehp.modares.ac.ir/article-5-58000-en.html
URL: http://hehp.modares.ac.ir/article-5-58000-en.html
1- Health Promotion Research Center, Iran University of Medical Sciences, Tehran, Iran
2- Department of Public Health, Social Determinants of Health Research Center, Saveh University of Medical Sciences, Saveh, Iran
3- Department of Nursing, Saveh University of Medical Sciences, Saveh, Iran
4- Department of Psychology” and “Department of Health Sciences”, University of Rhode Island, Rhode Island, USA
2- Department of Public Health, Social Determinants of Health Research Center, Saveh University of Medical Sciences, Saveh, Iran
3- Department of Nursing, Saveh University of Medical Sciences, Saveh, Iran
4- Department of Psychology” and “Department of Health Sciences”, University of Rhode Island, Rhode Island, USA
Full-Text [PDF 993 kb]
(3745 Downloads)
| Abstract (HTML) (1811 Views)
Table 2) The Mean±SD score of HPLPII and its dimensions according to demographic and socioeconomic variables

Table 3) The Mean±SD score of HPL and its dimensions

Discussion
The current study focused on assessing health-promoting activities among adolescent females in Saveh, Iran. The HPLP II mean score among participants was moderate (89.3±11.2), which was consistent with previous research conducted in Iran before the COVID-19 pandemic [16, 23, 25, 27]. Similar studies in other Asian countries have yielded almost identical results pre-COVID-19 pandemic, finding moderate health-promoting behaviors among teenagers [28-30]. Given the critical significance of adolescent health-promoting behavior and the fact that misbehavior and an unhealthy lifestyle are among the world's leading causes of mortality [29], as well as the necessity of health-promoting behavior to avoid chronic illnesses [30], our findings highlight the importance of planning for teaching health-promoting habits to adolescents. In our study, students who picked exercise and study as their favorite hobbies scored considerably higher on the HPLP II than students who selected mobile phones for their entertainment. This finding is expected because exercise and study are among the basic factors and variables affecting health promotion. On the other hand, smartphones and computer games cause inactivity, weight gain, and high-risk behaviors in adolescents [31]. Given that in our study, most students mentioned the mobile phone as a means of entertainment, it seems that by informing and encouraging students to use appropriate applications [16] designed to promote health, mobile capacity can be used as a useful tool to improve health-promoting behavior in students.
In the “Health Promoting Lifestyle” section, the Health Responsibility subscale scored above average. In line with our study findings, research has found that high overall HPLP II scores were associated with high health responsibility scores [30, 32]. However, several studies indicated that despite high overall HPLP II scores, the health responsibility domain had a low score across the dimensions [33, 34]. Possible reasons for the discrepancy between the current study findings and previous research are the differences in ages of students and the fact that the current study was conducted during an ongoing global pandemic, which may have increased health responsibility among adolescents via training provided by the media and the increased sensitivity and perceived severity of the COVID-19 disease.
Our result also indicated that scores of nutrition dimensions were higher than average. Almutairi et al. [30] also acquired similar findings regarding nutrition. An analytical study of behaviors in this domain indicated that having breakfast produced the highest nutritional score. Possible explanations for high scores on this item include students being confined at home instead of going to school, which may provide more time and convince them for eating breakfast without the stress of being late to school. Fruit and vegetable consumption were the lowest scoring items within the nutrition domain, which is consistent with recent UNICEF report findings that fruit and vegetable consumption decreased by 33% during the COVID-19 crisis [35]. This occurrence may be explained by more opportunities for youth to consume unhealthy foods over fruits and vegetables while at home, such as engaging in more baking and “snacking”.
We found that the mean score for the physical activity dimension was lower than the mean score for health responsibility and nutrition. This is in line with the findings of previous studies in Iran that show that Iranian female adolescents have a sedentary lifestyle [16]. Research has found that low physical activity among female adolescents in Iran is associated with a lack of sports facilities, insufficient outdoor space in schools, low self-efficacy to engage in exercise among female youth, air pollution, academic responsibilities, and cultural restrictions on girls’ participation in physical and sports activities [28]. In addition, in Iranian schools, adolescents spend an average of one hour a week exercising. One of the negative consequences of the COVID-19 pandemic was the closure of schools, and sports venues, and restrictions on holding ceremonies and gatherings, which have been effective in further reducing female students' physical activity by providing additional barriers [36]. It is important to note that pre-COVID-19 pandemic studies have also indicated that adolescents' physical activity was already decreased in association with the increasing expansion of virtual media [25, 37].
Our findings showed that the lowest score across the domains of HPLP II was stress management. Previous studies have shown that adolescence is associated with increased stress due to hormonal and physical changes, challenges brought on by the transition from childhood to adolescence, and inadequate stress management skills [25, 38]. The COVID-19 pandemic has further compacted poor management of stress due to a lack of adequate education and modeling of stress management while schools and educational centers were closed [36]. Furthermore, female youth have a greater need for stress management skills during the COVID-19 pandemic, as anxiety-related risk factors were found to predominantly endanger female students [34]. Using the capacity of counselors and teaching stress management skills in student textbooks and family education can be effective in managing student stress.
Our findings show several significant associations between demographic variables and adolescent health-promoting behaviors. The employment status of participant fathers has a substantial impact on the average HPLP II score and the nutrition domain. One probable explanation for this link is a decline in family income owing to unemployment, which is consistent with previous study findings [33, 39]. There was also a significant relationship between maternal education level and students' nutrition domain and average HPLP II score, which is consistent with the previous studies [18, 27]; however, the relationship between parental health literacy level and youth health-promoting behaviors has been proven in previous studies [18, 40]. This difference in the literature and the current findings is expected given that this study did not examine health literacy specifically. The study limitations included the use of self-report tools and the cross-sectional nature of research; hence, we could not infer the causal relationships.
Conclusion
A moderate mean score of HPLP II was identified in our study. The domains of stress management and physical activities received the lowest score among the HPLP II subscales. Given that the pandemic is ongoing and continuing to affect adolescents in numerous ways, it is suggested that necessary interventions to improve health-promoting behavior among female adolescents be adapted and implemented within the limitations and context of the pandemic.
Acknowledgments: We gratefully acknowledge the very helpful participation of the adolescents; without whose contribution the present study would not have been completed.
Ethical Permissions: The study was approved by the Institutional Review Board and the Ethics Committee of Saveh University of Medical Sciences, Saveh, Iran (approval code: IR.SAVEHUMS.REC.1399.016). Also, all participants in this study completed a written informed consent.
Conflicts of Interests: None declared.
Authors’ Contributions: Saboohi Z (First Author), Introduction Writer/Methodologist/Main Researcher (35%); Hoseini Koukamari P (Second Author), Methodologist/Assistant Researcher (10%); Rohani MR (Third Author), Assistant Researcher/Discussion Writer (10%); Rawlins J (Forth Author), Methodologist (10%); Karimy M (Fifth Author), Main Researcher/Statistical Analyst/Discussion Writer (35%)
Funding/Support: The research was fully funded by Saveh University of Medical Sciences, Iran. The funding body didn’t play any role in the design of the study and collection, analysis, and interpretation of data and the writing the manuscript.
Full-Text: (697 Views)
Introduction
Adolescents are an incredibly important group within society, as they make up 16 percent of the global population and are the future of humanity [1]. Adolescence is defined as the life development period between the ages of 10 and 19 and is associated with significant physical, psychological, and social changes [2]. Recent census reports estimate that 5697111 million individuals in Iran's total population are adolescents and young people, ranging in age from 10 to 19 years [3]. Although adolescent health is critical for a country's social, economic, and political growth, it is evident that their health needs are not always prioritized in national policy [4].
Although mortality rates have improved throughout time, rates among Iranian female children remain relatively high, with 13.3 deaths per 1,000 live births [5]. A major of the deaths among this group are avoidable, often the result of road accidents, high-risk health behaviors (e.g. Unprotected sex, smoking), respiratory tract infections, mental illnesses, early pregnancy and delivery, alcoholism, nutritional deficiencies, malnutrition, and lack of physical exercise. All of these factors can jeopardize not just the current health of youth, but also the health of future generations. Promoting healthy habits throughout puberty and adopting preventative measures against high-risk behaviors are essential for the health and future of youth populations [6].
The COVID-19 pandemic has brought about quick and extraordinary changes in the lives of all people, particularly adolescents, all across the world [7]. The pandemic has been associated with negative physical and mental health consequences, including muscle loss, decreased cardiac and respiratory fitness, weight gain, psychological distress, interpersonal difficulties, and poor academic performance. These negative effects can last into adulthood [8, 9]. Global female youth experienced numerous negative consequences of the COVID-19 pandemic, such as increased dropout from school, child labor, internet addiction [6], gender gaps within home responsibilities [10], high levels of stress and mental health disorders [11], increased alcohol consumption, drug use and smoking rates [12], premature and forced marriage [13], nutritional problems, and physical violence and neglect [14]. A health-promoting lifestyle is an important determinant of health status and is recognized as a key factor in maintaining and improving health [15].
Adolescent health-promoting behavior consists of four important dimensions, which include health responsibility, stress management, nutrition, and physical activity [16]. A healthy lifestyle such as regular physical activities, maintaining a healthy body weight, a healthy diet, and avoiding smoking and stress, play a key role in health promotion strategy [17, 18]. The Wang et al. [19] research indicated that good health-promoting behavior depends on the habits of life adopted in the early years of life. Previous research provided evidence of the association between the lack of physical activity with many chronic diseases [20, 21]. Lifestyle changes towards stress management behaviors and a healthy diet are also important factors in the prevention of chronic diseases [16]. Evidence suggests that habits established during childhood and adolescence would continue for the whole life [18, 22]. Musavian et al. [16] indicated that to healthy lifestyle among adolescents, health policymakers need to pay special attention to their nutrition, stress management skills, physical activity, health responsibility, and social support.
In today's society, lifestyle is widely acknowledged as a key predictor of one's health. According to WHO research, lifestyle and personal health behavior influence about 65 percent of an individual's health and quality of life [23]. Because lifestyle and unhealthy behaviors account for roughly 53% of fatalities [2, 6], changing lifestyle and adopting a healthy lifestyle reduces the incidence and severity of many chronic illnesses and even mortality [16]. Adolescence is a critical period for establishing any health-related habits, especially for females, since these habits will be carried over into adulthood [20, 21]. Because it is more difficult to alter harmful habits in adulthood, research on what impacts lifestyle behaviors among adolescents is vital for health prevention and intervention measures [24].
Several studies have examined the health-promoting behaviors among adolescents before the COVID-19 pandemic; however, there is a dearth of research examining health behaviors among youth during the pandemic. The present study aimed to evaluate the health-promoting behaviors among female Iranian adolescents during the COVID-19 pandemic.
Instrument and Methods
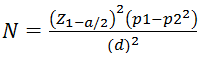
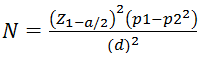
The present descriptive-analytical study recruited female high school students in Saveh, Iran, in 2021. A target sample size of 480 was determined by taking into account accuracy of 0.05 and 95% confidence, using the following formula,
and was increased to 529 in consideration of the probability of dropout. Participants were selected through a multi-stage sampling process, starting with a list of all female high schools in two districts of Saveh (n=14). Next, three high schools were selected at random from each district, for a total of six schools included in the study. The research involved randomly a class from each grade of high school and, from the 10th, 11th, and 12th grades. Finally, using random sampling, 90 subjects were chosen from each school's student list and 11 students were excluded from the final sample due to not completing all questionnaire items.
Due to the COVID-19 pandemic, the data collection method takes place entirely online through SHAD student software. The anonymous self-administration questionnaire was sent to students, and to ensure data confidentiality. Besides sufficient time was given to the students to answer the questionnaire. It took around 14 days to fill in the entire questionnaire. Background Questions on demographic information and personal characteristics were included in the background data collecting tool. Seven items regarding personal characteristics were included in the questionnaire, including age, BMI, education levels and employment of father and mother, hobbies, and Grade point average (GPA range for low “<14 scores”, the average “14-17” and high “>17”). The HPLP II (Health-promoting Lifestyle Profile II) [26] was utilized to assess health-promoting behaviors across four domains: nutrition (9 items), physical activity (8 items), health responsibility (9 items), and stress management (stressors identification and stress management measures, 8 items). The responses were recorded on a four-point Likert scale: never (1 point), occasionally (2 points), frequently (3 points), and always (4 points). The total scores obtained in all domains were used to calculate a total and average health-promoting behavior score with a minimum possible score of 34 and a maximum score of 136. A higher score implies a greater health-promoting lifestyle. The scores for items from each sub-category were used to calculate behavioral dimension scores for each domain. The study found low (34-68), moderate (68-102), and high (102-136) health-promoting lifestyle scores. Mohamadian et al. translated and validated the questionnaire for use in Iran [26]. Cronbach's alpha for each behavior domain (physical activity, α=0.75; health responsibility, α=0.77; nutrition, α=0.70; stress management, α=0.71) and overall questionnaire (α=0.76) indicated good reliability.
Individuals were eligible for participation if they were studying at one of the female high schools in Saveh, did not have dietary and activity restrictions possessed a smartphone and had informed consent from their parents to participate in the study. All participants were informed about the purpose of the study and confidentiality protocols and gave written informed consent. The present study was taken at Saveh University of Medical Sciences, questionnaires were anonymous and participation in the study was optional and free. Participants completed several questionnaires to assess background information, personal characteristics, and health behaviors.
Data analyses were performed using IBM SPSS ver. 21.0. The Kolmogorov–Smirnov test was used to assess the normality of the data. Descriptive statistics of background variables and health-promoting behaviors were analyzed. One-way analysis of variance (ANOVA) and independent t-test were used to compare means across categories of demographic characteristics (i.e., GPA, parental employment and education, BMI, and hobbies) and health-promoting behaviors of the HPLP II, and post hoc tests were used for significant differences.
Findings
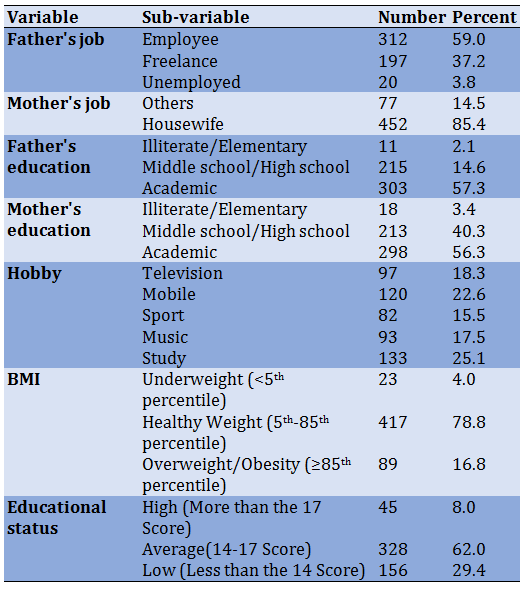
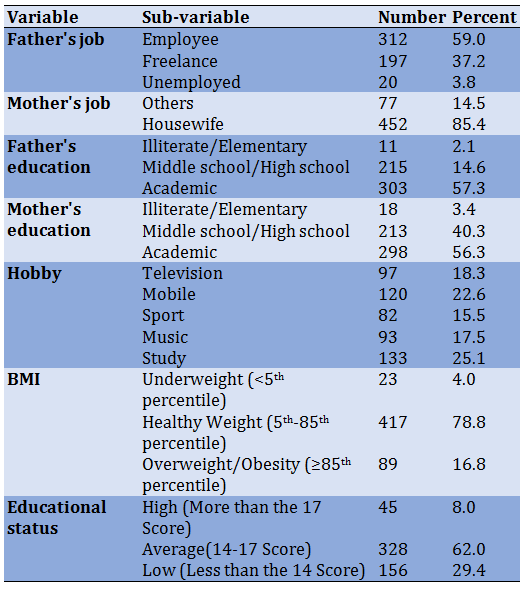
A total of 529 respondents completed the survey. All of the participants were female. The mean age of participants was 17.2±3.7 and the prevalence rate of overweight and obesity based on the BMI index was 16.8%. In total, 62% of adolescents had an average educational status regarding their GPA. More than half of the participants mothers and fathers had university-level education, 56.3%, and 57.3%, respectively. Roughly 60% of participants’ fathers were employees and nearly 85% of mothers were housewives (Table 1).
Table 1) Demographic characteristics and socioeconomic status of the participants
Results indicated moderate and high overall health-promoting behavior among 44% (n= 206) and 51% (n= 271) of youth, respectively, while the remaining participants indicated low overall health-promoting behavior. There was a significant difference in total health-promoting behavior mean score across hobby type, father’s occupation status, and mother’s education level (p<0.05; Table 2). The result of the Post hoc test showed Students with sports as their hobby had significantly higher average total health-promoting behavior scores, while participants who reported mobile phone usage as their hobby had unemployed fathers or mothers with only an elementary school education had significantly lower average total health-promoting behavior scores (Table 2).
The health responsibility domain mean scores were significantly different across hobby type and participant academic status i.e., GPA. Participants who indicated their hobby was sports activities had the highest average health responsibility score and those who reported mobile phones as their hobby had the lowest average health responsibility score. The result of the Post hoc test showed participants with high and average academic performance also reported significantly higher average health responsibility scores than those with low academic status. Findings showed that average nutrition domain scores were significantly different across the mother’s education level, father's occupation status, and hobby type. Similar to the results reported above, the result of the Post hoc test showed participants who indicated mobile phones as a hobby type had significantly lower nutrition averages compared to sports activities. Furthermore, significantly lower nutrition scores were of participants who had unemployed fathers and mothers with elementary educations. The physical activity domain mean scores were only significantly different across hobby types, such that participants who reported sports activities as their hobby type had the highest average physical activity scores, and those who reported mobile phones as their hobby type had significantly lower average physical activity scores. The stress management domain mean scores were significantly different across the father's occupation status, hobby type, and participant’s academic status. The result of the Post hoc test r showed female adolescents with unemployed fathers, mobile phone hobby preference, and low academic status had significantly lower stress management scores than those with employee fathers, sports activities as a hobby, and high academic performance (Table 2).
The mean scores of all the structures of Health Promoting Lifestyle (health responsibility, stress management, physical activity, and healthy eating) for participants were higher than average (Table3).
Adolescents are an incredibly important group within society, as they make up 16 percent of the global population and are the future of humanity [1]. Adolescence is defined as the life development period between the ages of 10 and 19 and is associated with significant physical, psychological, and social changes [2]. Recent census reports estimate that 5697111 million individuals in Iran's total population are adolescents and young people, ranging in age from 10 to 19 years [3]. Although adolescent health is critical for a country's social, economic, and political growth, it is evident that their health needs are not always prioritized in national policy [4].
Although mortality rates have improved throughout time, rates among Iranian female children remain relatively high, with 13.3 deaths per 1,000 live births [5]. A major of the deaths among this group are avoidable, often the result of road accidents, high-risk health behaviors (e.g. Unprotected sex, smoking), respiratory tract infections, mental illnesses, early pregnancy and delivery, alcoholism, nutritional deficiencies, malnutrition, and lack of physical exercise. All of these factors can jeopardize not just the current health of youth, but also the health of future generations. Promoting healthy habits throughout puberty and adopting preventative measures against high-risk behaviors are essential for the health and future of youth populations [6].
The COVID-19 pandemic has brought about quick and extraordinary changes in the lives of all people, particularly adolescents, all across the world [7]. The pandemic has been associated with negative physical and mental health consequences, including muscle loss, decreased cardiac and respiratory fitness, weight gain, psychological distress, interpersonal difficulties, and poor academic performance. These negative effects can last into adulthood [8, 9]. Global female youth experienced numerous negative consequences of the COVID-19 pandemic, such as increased dropout from school, child labor, internet addiction [6], gender gaps within home responsibilities [10], high levels of stress and mental health disorders [11], increased alcohol consumption, drug use and smoking rates [12], premature and forced marriage [13], nutritional problems, and physical violence and neglect [14]. A health-promoting lifestyle is an important determinant of health status and is recognized as a key factor in maintaining and improving health [15].
Adolescent health-promoting behavior consists of four important dimensions, which include health responsibility, stress management, nutrition, and physical activity [16]. A healthy lifestyle such as regular physical activities, maintaining a healthy body weight, a healthy diet, and avoiding smoking and stress, play a key role in health promotion strategy [17, 18]. The Wang et al. [19] research indicated that good health-promoting behavior depends on the habits of life adopted in the early years of life. Previous research provided evidence of the association between the lack of physical activity with many chronic diseases [20, 21]. Lifestyle changes towards stress management behaviors and a healthy diet are also important factors in the prevention of chronic diseases [16]. Evidence suggests that habits established during childhood and adolescence would continue for the whole life [18, 22]. Musavian et al. [16] indicated that to healthy lifestyle among adolescents, health policymakers need to pay special attention to their nutrition, stress management skills, physical activity, health responsibility, and social support.
In today's society, lifestyle is widely acknowledged as a key predictor of one's health. According to WHO research, lifestyle and personal health behavior influence about 65 percent of an individual's health and quality of life [23]. Because lifestyle and unhealthy behaviors account for roughly 53% of fatalities [2, 6], changing lifestyle and adopting a healthy lifestyle reduces the incidence and severity of many chronic illnesses and even mortality [16]. Adolescence is a critical period for establishing any health-related habits, especially for females, since these habits will be carried over into adulthood [20, 21]. Because it is more difficult to alter harmful habits in adulthood, research on what impacts lifestyle behaviors among adolescents is vital for health prevention and intervention measures [24].
Several studies have examined the health-promoting behaviors among adolescents before the COVID-19 pandemic; however, there is a dearth of research examining health behaviors among youth during the pandemic. The present study aimed to evaluate the health-promoting behaviors among female Iranian adolescents during the COVID-19 pandemic.
Instrument and Methods
The present descriptive-analytical study recruited female high school students in Saveh, Iran, in 2021. A target sample size of 480 was determined by taking into account accuracy of 0.05 and 95% confidence, using the following formula,
and was increased to 529 in consideration of the probability of dropout. Participants were selected through a multi-stage sampling process, starting with a list of all female high schools in two districts of Saveh (n=14). Next, three high schools were selected at random from each district, for a total of six schools included in the study. The research involved randomly a class from each grade of high school and, from the 10th, 11th, and 12th grades. Finally, using random sampling, 90 subjects were chosen from each school's student list and 11 students were excluded from the final sample due to not completing all questionnaire items.
Due to the COVID-19 pandemic, the data collection method takes place entirely online through SHAD student software. The anonymous self-administration questionnaire was sent to students, and to ensure data confidentiality. Besides sufficient time was given to the students to answer the questionnaire. It took around 14 days to fill in the entire questionnaire. Background Questions on demographic information and personal characteristics were included in the background data collecting tool. Seven items regarding personal characteristics were included in the questionnaire, including age, BMI, education levels and employment of father and mother, hobbies, and Grade point average (GPA range for low “<14 scores”, the average “14-17” and high “>17”). The HPLP II (Health-promoting Lifestyle Profile II) [26] was utilized to assess health-promoting behaviors across four domains: nutrition (9 items), physical activity (8 items), health responsibility (9 items), and stress management (stressors identification and stress management measures, 8 items). The responses were recorded on a four-point Likert scale: never (1 point), occasionally (2 points), frequently (3 points), and always (4 points). The total scores obtained in all domains were used to calculate a total and average health-promoting behavior score with a minimum possible score of 34 and a maximum score of 136. A higher score implies a greater health-promoting lifestyle. The scores for items from each sub-category were used to calculate behavioral dimension scores for each domain. The study found low (34-68), moderate (68-102), and high (102-136) health-promoting lifestyle scores. Mohamadian et al. translated and validated the questionnaire for use in Iran [26]. Cronbach's alpha for each behavior domain (physical activity, α=0.75; health responsibility, α=0.77; nutrition, α=0.70; stress management, α=0.71) and overall questionnaire (α=0.76) indicated good reliability.
Individuals were eligible for participation if they were studying at one of the female high schools in Saveh, did not have dietary and activity restrictions possessed a smartphone and had informed consent from their parents to participate in the study. All participants were informed about the purpose of the study and confidentiality protocols and gave written informed consent. The present study was taken at Saveh University of Medical Sciences, questionnaires were anonymous and participation in the study was optional and free. Participants completed several questionnaires to assess background information, personal characteristics, and health behaviors.
Data analyses were performed using IBM SPSS ver. 21.0. The Kolmogorov–Smirnov test was used to assess the normality of the data. Descriptive statistics of background variables and health-promoting behaviors were analyzed. One-way analysis of variance (ANOVA) and independent t-test were used to compare means across categories of demographic characteristics (i.e., GPA, parental employment and education, BMI, and hobbies) and health-promoting behaviors of the HPLP II, and post hoc tests were used for significant differences.
Findings
A total of 529 respondents completed the survey. All of the participants were female. The mean age of participants was 17.2±3.7 and the prevalence rate of overweight and obesity based on the BMI index was 16.8%. In total, 62% of adolescents had an average educational status regarding their GPA. More than half of the participants mothers and fathers had university-level education, 56.3%, and 57.3%, respectively. Roughly 60% of participants’ fathers were employees and nearly 85% of mothers were housewives (Table 1).
Table 1) Demographic characteristics and socioeconomic status of the participants
Results indicated moderate and high overall health-promoting behavior among 44% (n= 206) and 51% (n= 271) of youth, respectively, while the remaining participants indicated low overall health-promoting behavior. There was a significant difference in total health-promoting behavior mean score across hobby type, father’s occupation status, and mother’s education level (p<0.05; Table 2). The result of the Post hoc test showed Students with sports as their hobby had significantly higher average total health-promoting behavior scores, while participants who reported mobile phone usage as their hobby had unemployed fathers or mothers with only an elementary school education had significantly lower average total health-promoting behavior scores (Table 2).
The health responsibility domain mean scores were significantly different across hobby type and participant academic status i.e., GPA. Participants who indicated their hobby was sports activities had the highest average health responsibility score and those who reported mobile phones as their hobby had the lowest average health responsibility score. The result of the Post hoc test showed participants with high and average academic performance also reported significantly higher average health responsibility scores than those with low academic status. Findings showed that average nutrition domain scores were significantly different across the mother’s education level, father's occupation status, and hobby type. Similar to the results reported above, the result of the Post hoc test showed participants who indicated mobile phones as a hobby type had significantly lower nutrition averages compared to sports activities. Furthermore, significantly lower nutrition scores were of participants who had unemployed fathers and mothers with elementary educations. The physical activity domain mean scores were only significantly different across hobby types, such that participants who reported sports activities as their hobby type had the highest average physical activity scores, and those who reported mobile phones as their hobby type had significantly lower average physical activity scores. The stress management domain mean scores were significantly different across the father's occupation status, hobby type, and participant’s academic status. The result of the Post hoc test r showed female adolescents with unemployed fathers, mobile phone hobby preference, and low academic status had significantly lower stress management scores than those with employee fathers, sports activities as a hobby, and high academic performance (Table 2).
The mean scores of all the structures of Health Promoting Lifestyle (health responsibility, stress management, physical activity, and healthy eating) for participants were higher than average (Table3).
Table 2) The Mean±SD score of HPLPII and its dimensions according to demographic and socioeconomic variables

Table 3) The Mean±SD score of HPL and its dimensions

Discussion
The current study focused on assessing health-promoting activities among adolescent females in Saveh, Iran. The HPLP II mean score among participants was moderate (89.3±11.2), which was consistent with previous research conducted in Iran before the COVID-19 pandemic [16, 23, 25, 27]. Similar studies in other Asian countries have yielded almost identical results pre-COVID-19 pandemic, finding moderate health-promoting behaviors among teenagers [28-30]. Given the critical significance of adolescent health-promoting behavior and the fact that misbehavior and an unhealthy lifestyle are among the world's leading causes of mortality [29], as well as the necessity of health-promoting behavior to avoid chronic illnesses [30], our findings highlight the importance of planning for teaching health-promoting habits to adolescents. In our study, students who picked exercise and study as their favorite hobbies scored considerably higher on the HPLP II than students who selected mobile phones for their entertainment. This finding is expected because exercise and study are among the basic factors and variables affecting health promotion. On the other hand, smartphones and computer games cause inactivity, weight gain, and high-risk behaviors in adolescents [31]. Given that in our study, most students mentioned the mobile phone as a means of entertainment, it seems that by informing and encouraging students to use appropriate applications [16] designed to promote health, mobile capacity can be used as a useful tool to improve health-promoting behavior in students.
In the “Health Promoting Lifestyle” section, the Health Responsibility subscale scored above average. In line with our study findings, research has found that high overall HPLP II scores were associated with high health responsibility scores [30, 32]. However, several studies indicated that despite high overall HPLP II scores, the health responsibility domain had a low score across the dimensions [33, 34]. Possible reasons for the discrepancy between the current study findings and previous research are the differences in ages of students and the fact that the current study was conducted during an ongoing global pandemic, which may have increased health responsibility among adolescents via training provided by the media and the increased sensitivity and perceived severity of the COVID-19 disease.
Our result also indicated that scores of nutrition dimensions were higher than average. Almutairi et al. [30] also acquired similar findings regarding nutrition. An analytical study of behaviors in this domain indicated that having breakfast produced the highest nutritional score. Possible explanations for high scores on this item include students being confined at home instead of going to school, which may provide more time and convince them for eating breakfast without the stress of being late to school. Fruit and vegetable consumption were the lowest scoring items within the nutrition domain, which is consistent with recent UNICEF report findings that fruit and vegetable consumption decreased by 33% during the COVID-19 crisis [35]. This occurrence may be explained by more opportunities for youth to consume unhealthy foods over fruits and vegetables while at home, such as engaging in more baking and “snacking”.
We found that the mean score for the physical activity dimension was lower than the mean score for health responsibility and nutrition. This is in line with the findings of previous studies in Iran that show that Iranian female adolescents have a sedentary lifestyle [16]. Research has found that low physical activity among female adolescents in Iran is associated with a lack of sports facilities, insufficient outdoor space in schools, low self-efficacy to engage in exercise among female youth, air pollution, academic responsibilities, and cultural restrictions on girls’ participation in physical and sports activities [28]. In addition, in Iranian schools, adolescents spend an average of one hour a week exercising. One of the negative consequences of the COVID-19 pandemic was the closure of schools, and sports venues, and restrictions on holding ceremonies and gatherings, which have been effective in further reducing female students' physical activity by providing additional barriers [36]. It is important to note that pre-COVID-19 pandemic studies have also indicated that adolescents' physical activity was already decreased in association with the increasing expansion of virtual media [25, 37].
Our findings showed that the lowest score across the domains of HPLP II was stress management. Previous studies have shown that adolescence is associated with increased stress due to hormonal and physical changes, challenges brought on by the transition from childhood to adolescence, and inadequate stress management skills [25, 38]. The COVID-19 pandemic has further compacted poor management of stress due to a lack of adequate education and modeling of stress management while schools and educational centers were closed [36]. Furthermore, female youth have a greater need for stress management skills during the COVID-19 pandemic, as anxiety-related risk factors were found to predominantly endanger female students [34]. Using the capacity of counselors and teaching stress management skills in student textbooks and family education can be effective in managing student stress.
Our findings show several significant associations between demographic variables and adolescent health-promoting behaviors. The employment status of participant fathers has a substantial impact on the average HPLP II score and the nutrition domain. One probable explanation for this link is a decline in family income owing to unemployment, which is consistent with previous study findings [33, 39]. There was also a significant relationship between maternal education level and students' nutrition domain and average HPLP II score, which is consistent with the previous studies [18, 27]; however, the relationship between parental health literacy level and youth health-promoting behaviors has been proven in previous studies [18, 40]. This difference in the literature and the current findings is expected given that this study did not examine health literacy specifically. The study limitations included the use of self-report tools and the cross-sectional nature of research; hence, we could not infer the causal relationships.
Conclusion
A moderate mean score of HPLP II was identified in our study. The domains of stress management and physical activities received the lowest score among the HPLP II subscales. Given that the pandemic is ongoing and continuing to affect adolescents in numerous ways, it is suggested that necessary interventions to improve health-promoting behavior among female adolescents be adapted and implemented within the limitations and context of the pandemic.
Acknowledgments: We gratefully acknowledge the very helpful participation of the adolescents; without whose contribution the present study would not have been completed.
Ethical Permissions: The study was approved by the Institutional Review Board and the Ethics Committee of Saveh University of Medical Sciences, Saveh, Iran (approval code: IR.SAVEHUMS.REC.1399.016). Also, all participants in this study completed a written informed consent.
Conflicts of Interests: None declared.
Authors’ Contributions: Saboohi Z (First Author), Introduction Writer/Methodologist/Main Researcher (35%); Hoseini Koukamari P (Second Author), Methodologist/Assistant Researcher (10%); Rohani MR (Third Author), Assistant Researcher/Discussion Writer (10%); Rawlins J (Forth Author), Methodologist (10%); Karimy M (Fifth Author), Main Researcher/Statistical Analyst/Discussion Writer (35%)
Funding/Support: The research was fully funded by Saveh University of Medical Sciences, Iran. The funding body didn’t play any role in the design of the study and collection, analysis, and interpretation of data and the writing the manuscript.
Article Type: Descriptive & Survey |
Subject:
Health Education and Health Behavior
Received: 2021/12/18 | Accepted: 2022/02/13 | Published: 2022/06/14
Received: 2021/12/18 | Accepted: 2022/02/13 | Published: 2022/06/14
References
1. Jalili Z, Saboohi Z, Tavakoli R. Effect of training program on snack consumption in elementary school girls: application of the BASNEF model. J Educ Community Health. 2021;8:3-9. [Link] [DOI:10.52547/jech.8.1.3]
2. Sarkhani N, Pashaeypoor S, Negarandeh R. Student health ambassadors: a new program to promote health among the adolescent. Int J Community Based Nurs Midwifery. 2021;9(1):88-90. [Link]
3. amar.org.ir [Internet]. Tehran: Statistical Center of Iran; 2021 [Cited 2022 Apr 1]. Available from: https://www.amar.org.ir/ [Persian] [Link]
4. Gaete J, Olivares E, Godoy MI, Cárcamo M, Montero-Marín J. ConstanceHendrickset al., Adolescent lifestyle profile-revised 2: validity and reliability among adolescents in chile. Jornal de Pediatria. 2021;97(1):52-60. [Link] [DOI:10.1016/j.jped.2019.11.005]
5. Khazaei S, Najafi F, Armanmehr V, Hajipour M, Karami M, Rezaeian S. Trend analysis of mortality rates for leading causes of death among under-five children in Iran, 2000-2015. J Compr Pediatr. 2019;10(2). [Persian] [Link] [DOI:10.5812/compreped.86902]
6. Kumar MM, Karpaga PP, Panigrahi SK, Raj U, Pathak VK. Impact of COVID-19 pandemic on adolescent health in India. J Fam Med Primary Care. 2020;9(11):5484. [Link] [DOI:10.4103/jfmpc.jfmpc_1266_20]
7. Fazeli S, Zeidi IM, Lin CY, Namdar P, Griffiths MD, Ahorsu DK, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep. 2020;12:100307. [Link] [DOI:10.1016/j.abrep.2020.100307]
8. United Nations. Policy brief: the impact of COVID-19 on children. New York: United Nations; 2020. [Link]
9. Orben A, Tomova L, Blakemore SJ. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc Health. 2020;4(8):634-40. [Link] [DOI:10.1016/S2352-4642(20)30186-3]
10. Hupkau C, Petrongolo B. COVID-19 and gender gaps: Latest evidence and lessons from the UK. VoxEU; 2020. [Link]
11. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4(6):421. [Link] [DOI:10.1016/S2352-4642(20)30109-7]
12. Bao X, Qu H, Zhang R, Hogan TP. Modeling reading ability gain in kindergarten children during COVID-19 school closures. Int J Environ Res Public Health. 2020;17(17):6371. [Link] [DOI:10.3390/ijerph17176371]
13. Brides GN. COVID-19 and child, early and forced marriage: an agenda for action. London: Girls Not Brides; 2020. [Link]
14. Nowiński A, Ufnal M. Trimethylamine N-oxide: a harmful, protective or diagnostic marker in lifestyle diseases?. Nutrition. 2018;46:7-12. [Link] [DOI:10.1016/j.nut.2017.08.001]
15. Hamed Bieyabanie M, Mohammad-Alizadeh Charandabi S, Mirghafourvand M. Effect of Counseling on the Health-Promoting Lifestyle and Quality of Life among Mastectomised Women. Health Educ Health Promot. 2021;9(4):317-324. [Link]
16. Musavian AS, Pasha A, Rahebi SM, Roushan ZA, Ghanbari A. Health promoting behaviors among adolescents: A cross-sectional study. Nurs Midwifery Stud. 2014;3(1). [Link] [DOI:10.17795/nmsjournal14560]
17. Araban M, Baharzadeh K, Karimy M. Nutrition modification aimed at enhancing dietary iron and folic acid intake: an application of health belief model in practice. Eur J Public Health. 2017;27(2):287-92. [Link] [DOI:10.1093/eurpub/ckx014]
18. Armoon B, Karimy M. Epidemiology of childhood overweight, obesity and their related factors in a sample of preschool children from Central Iran. BMC Pediatr. 2019;19(1):1-8. [Link] [DOI:10.1186/s12887-019-1540-5]
19. Wang D, Ou CQ, Chen MY, Duan N. Health-promoting lifestyles of university students in Mainland China. BMC Public Health. 2009;9(1):1-9. [Link] [DOI:10.1186/1471-2458-9-379]
20. De Boer DR, Hoekstra F, Huetink KI, Hoekstra T, Krops LA, Hettinga FJ. Physical activity, sedentary behavior and well-being of adults with physical disabilities and/or chronic diseases during the first wave of the COVID-19 pandemic: A rapid review. Int J Environ Res Public Health. 2021;18(12):6342. [Link] [DOI:10.3390/ijerph18126342]
21. Mazzucca S, Arredondo EM, Hoelscher DM, Haire-Joshu D, Tabak RG, Kumanyika SK, et al., Expanding implementation research to prevent chronic diseases in community settings. Ann Rev Public Health. 2021;42:135. [Link] [DOI:10.1146/annurev-publhealth-090419-102547]
22. Karimy M, Higgs P, Abadi SS, Armoon B, Araban M, Rouhani MR, et al., Oral health behavior among school children aged 11-13 years in Saveh, Iran: an evaluation of a theory-driven intervention. BMC Pediatr 2020;20(1):1-9. [Link] [DOI:10.1186/s12887-020-02381-6]
23. Mehri A, Solhi M, Garmaroudi G, Nadrian H, Sighaldeh SS. Health promoting lifestyle and its determinants among university students in Sabzevar, Iran. Int J Prevent Med. 2016;7. [Link] [DOI:10.4103/2008-7802.180411]
24. Bessa CC, Silva LA, Sousa TM, Silva VM, Galvão MT, Guedes NG. Health control for celiac patients: an analysis according to the Pender health promotion model. Texto Contexto-Enfermagem. 2019;29. [Link] [DOI:10.1590/1980-265x-tce-2018-0420]
25. Sharifi N, Sharifi F, Amel Barez M, Esmaily H. Assessment of health-promoting lifestyle in female students. J Midwifery Reprod Health. 2020;8(3):2303-9. [Persian] [Link]
26. Mohamadian H, Ardebili HE, Taghdisi MH, Mousavi GA, Sabahi-Bidgoli M. Psychometric properties of the health-promoting lifestyle profile (HPLP II) in a sample of Iranian adolescents. PAYESH. 2013;12(2):167-76. [Persian] [Link]
27. Motaghi M, Afsar M. Health behaviors among high school girls. Intl J Sch Health. 2015;2(1):1-6. [Link] [DOI:10.17795/intjsh-24994]
28. Karimi N, Gharin SS, Tol A, Sadeghi R, Yaseri M, Mohebbi B. Role of health literacy and demographic variables in determining health-promoting behaviors among high school female students in the city of Tehran, Iran. J Sch Public Health Instit Public Health Res. 2019;17(3):212-28. [Persian] [Link]
29. Huang CL, Yang SC, Chiang CH. The associations between individual factors, eHealth literacy, and health behaviors among college students. Int J Environ Res Public Health. 2020;17(6):2108. [Link] [DOI:10.3390/ijerph17062108]
30. Almutairi KM, Alonazi WB, Vinluan JM, Almigbal TH, Batais MA, Alodhayani AA, et al., Health promoting lifestyle of university students in Saudi Arabia: a cross-sectional assessment. BMC Public Health. 2018;18(1):1-10. [Link] [DOI:10.1186/s12889-018-5999-z]
31. Karimy M, Parvizi F, Rouhani MR, Griffiths MD, Armoon B, Fattah Moghaddam L. The association between internet addiction, sleep quality, and health-related quality of life among Iranian medical students. J Addict Dis. 2020;38(3):317-25. [Link] [DOI:10.1080/10550887.2020.1762826]
32. AlAteeq DA, Aljhani S, AlEesa D. Perceived stress among students in virtual classrooms during the COVID-19 outbreak in KSA. J Taibah UnivMed Sci. 2020;15(5):398-403. [Link] [DOI:10.1016/j.jtumed.2020.07.004]
33. Alzahrani SH, Malik AA, Bashawri J, Shaheen SA, Shaheen MM, Alsaib AA, et al. Health-promoting lifestyle profile and associated factors among medical students in a Saudi University. SAGE Open Med. 2019;7:2050312119838426. [Link] [DOI:10.1177/2050312119838426]
34. Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55-64. [Link] [DOI:10.1016/j.jad.2020.08.001]
35. Litton MM, Beavers AW. The relationship between food security status and fruit and vegetable intake during the COVID-19 pandemic. Nutrients. 2021;13(3):712. [Link] [DOI:10.3390/nu13030712]
36. Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Progress Cardiovasc Dis. 2020;63(4):531. [Link] [DOI:10.1016/j.pcad.2020.04.013]
37. Lotfi M, Hosseini S, Rafie A, Dostifar K, Kassiri H. A study on the life style of high school girls in relation to the prevention of osteoporosis, Ahvaz, Iran. Int J Adv Biotechnoly Res. 2017;8(4):371-9. [Link]
38. Solhi M, Azar FE, Maheri M, Khalili S, Abolghasemi J. The assessment of health-promoting lifestyle status and its determinants among students of Iran University of Medical Sciences. Iran J Health Safety Environ. 2021;7(2):1457-63. [Persian] [Link]
39. Balali Meybodi F, Hasani M, Mehdinejad M. Evaluating health-promoting life style and its related factors among adolescent girls of Kerman in 2015. Health Dev J. 2020;6(2):85-96. [Link]
40. Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Ann Rev Public Health. 2018;39:273-89. [Link] [DOI:10.1146/annurev-publhealth-031816-044628]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





