Volume 10, Issue 1 (2022)
Health Educ Health Promot 2022, 10(1): 109-114 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sharif Nia H, Mahmoudi H, Ebadi A, Moayed M. Mediating Role of Safety Policy on Contact Care in the Stress of Exposure to Sharps Injuries in Iranian Nurses. Health Educ Health Promot 2022; 10 (1) :109-114
URL: http://hehp.modares.ac.ir/article-5-53063-en.html
URL: http://hehp.modares.ac.ir/article-5-53063-en.html
1- Department of Nursing, Mazandaran University of Medical Science, Sari, Iran
2- Trauma Research Center, Nursing Faculty, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- “Behavioral Sciences Research Center, Lifestyle institute” and “Department of Nursing Management, Nursing Faculty”, Baqiyatallah University of Medical Sciences, Tehran, Iran
2- Trauma Research Center, Nursing Faculty, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- “Behavioral Sciences Research Center, Lifestyle institute” and “Department of Nursing Management, Nursing Faculty”, Baqiyatallah University of Medical Sciences, Tehran, Iran
Keywords: Needlestick Injury [MeSH], Occupational Safety [MeSH], Psychological Stress [MeSH], Mediation Analysis [MeSH], Risk Management [MeSH], Theoretical Model [MeSH]
Full-Text [PDF 452 kb]
(3232 Downloads)
| Abstract (HTML) (2201 Views)
Full-Text: (392 Views)
Introduction
Nurses and other healthcare workers (HCWs) are at risk of exposure to bloodborne pathogens, drops, and secretions that potentially result in infections every day while caring for patients [1]. The incidence rates of sharps injuries have been thus reported ranging from 1.4 to 9.5 per 100 HCWs [2]. However, modern technologies have allowed for conducting many laboratory tests and diagnostic procedures at the bedside particularly in critical care units (i.e., cardiac care units (CCUs) and intensive care units (ICUs)), operating rooms, and emergency departments (EDs), whose tests can be consequently achieved faster and an appropriate and immediate treatment can be further started as soon as possible. Although such technologies are useful for patients, the risks of injuries have thus far had a rising trend among nurses [3]. The consequences of diseases transmitted by blood-to-blood contact are not merely limited to such infections, but nurses might suffer from higher levels of anxiety and stress based on their perceptions of the risk of needlestick injuries and predicting others’ reactions [4]. They are frequently subjected to unpleasant thoughts, impaired mental focus, sleep disturbances, anger, and even low sex drive. As a motivating factor, this experience can thus exacerbate all previous mental problems [5].
In this sense, contact care, safety policy, occupational safety, as well as mental-environmental conditions (MECs) are among the most important factors shaping the levels of stress in nurses [6]. Direct or indirect patient contact is also one of the significant factors that can affect nurses’ performance and psychological conditions. The uncertainty of infections transmitted by needlestick injuries or other patient secretions might accordingly raise anxiety in HCWs, especially when patients have been known to be burdened with chronic viral infections and thus much time has been spent on direct contact with them [5, 7, 8]. In Safety Policy, HCWs have obligations to themselves and their patients to work safely [9, 10]. In one study, the highest levels of needlestick-related stress had been thus reported in nurses regarding this factor [11]. On the other hand, Safety Policy statements to prevent the transmission of such infections require robust and well-standardized infection control programs within healthcare delivery systems. The use of needlestick-prevention devices by nurses was accordingly suggested in the World Health Organization guidelines in 2016 [10]. In this sense, providing needle safety equipment in the clinical workplace combined with satisfactory training can significantly reduce the number of occupationally exposed needlestick injuries [12]. Vaccines as a means to prevent and eradicate bloodborne infectious diseases can be further developed [13]. occupational safety can thus refer to having an efficient vaccination schedule as well as sufficient skills in injury prevention and practicing timely treatment in case of injury with sharp objects [6]. One strategy to improve occupational safety is the identification of interactions between personal and situational factors [14]. MECs also represent the conditions nurses are working in, reprimands after injuries, services provided to patients in different situations that can increase the risk of injuries, and other situations that affect the mental status of nurses [6]. In one study, the role of safety climate and culture in enhancing safety performance in 31 selected studies had been evaluated, in which increasing the levels of safety climate and culture had diminished injuries and enriched safety performance indicators [15]. The theoretical model developed here (comprised of occupational safety, contact care, Safety Policy, and MECs) is thus a comprehensive model that includes not only organizational factors but also individual and environmental ones, in which failure to comply with any of these items, as well as deficiency, disturbance, or lack of the subsets of each one can cause the stress of exposure to sharp objects in nurses.
No study has so far investigated the relationship between these factors and their mediating role. Therefore, this path analysis was fulfilled to test a theoretical model to reflect on the relationship between safety policy, occupational safety, mental-environmental conditions, and contact care.
Instrument and Methods
This predictive cross-sectional study was conducted during the August 2018 to May 2019 on nurses of 4 provinces of Iran. The cluster sampling method was used to select 11 hospitals in 4 provinces in Iran, including Tehran (n=4), Kerman (n=2), Isfahan (n=3), and Shiraz (n=2). All the nurses (n=530), who have at least one year of work experience (in EDs, CCUs, and ICUs for pediatrics, neonates, open-heart surgery, surgery, internal medicine, and neurology as well as hemodialysis, surgery, and internal wards) with no history of severe stress such as the death of relatives were included in this study based on the convenience sampling method.
The data were further collected by a two-part questionnaire, containing demographic information (such as age, gender, marital status, level of education, and work experience) and the Stress of Exposure to Sharps Injury Scale [6] consisting of 20 closed statements scored using a 5-point Likert scale (very high=5, high=4, average=3, low=2, very low=1), wherein the maximum and minimum total scores could be 100 and 20, respectively. The scale has four dimensions including safety policy (5 items), occupational safety (5 items), contact care (4 items), and MECs (6 items). This self-report scale had been designed and its psychometric properties had been determined in 2014 [6]. Moreover, the test-retest reliability method was utilized to measure the scale consistency. Accordingly, 20 nurses completed this scale twice with a two-week interval. The reliability of this scale with Cronbach’s alpha was 0.89 and its intraclass correlation coefficient (ICC) was 0.9.
The study was approved by the ethical committee of Mazandaran University of Medical Sciences.
A path analysis was utilized to measure the effect of the factors on Contact Care by IBM SPSS Amos 24.0 software.
Findings
Three of the nurses were excluded from the study because some of the questions were not responded. More than half of the participants were female and married. Their mean age was 35.72±7.78 years, and the mean of work experience was 12.05±8.02 years (Table 1).
The correlation matrix between variables showed that the relationship between all variables included Occupational Safety (Mean±SD=16.78±5.49), Safety policy (Mean±SD=14.20±4.32), MECs (Mean±SD=14.31±3.61) with Contact care (Mean±SD=13.08±4.81) were statistically significant (Table 2).
Path analysis showed that all factors were positive and had significant effects on each other (Table 3;
Figure 1). In the final model of the stress of exposure to needlestick injury, safety policy has mediated between occupational safety, MECs, and contact care. This final model provided an acceptable fit for the data (χ2=1.02; p=0.007; CFI=0.989; TLI=0.936; IFI=0.975; RMSEA=0.032), with all individual paths significant at p<0.05 (Figure 1).
Table 1) Demographic characteristic of participants (N=527)
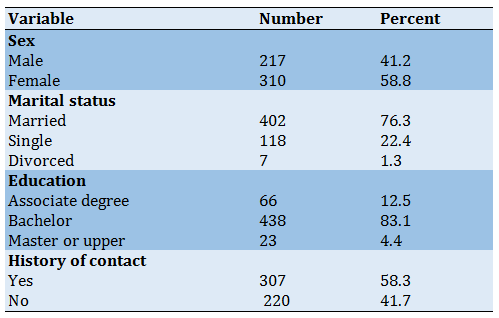
Table 2) Results of the correlation coefficient between factors (p<0.01)
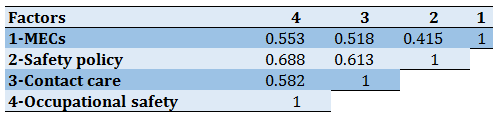
Table 3) Direct and indirect relationship between variables (p<0.001 for all)
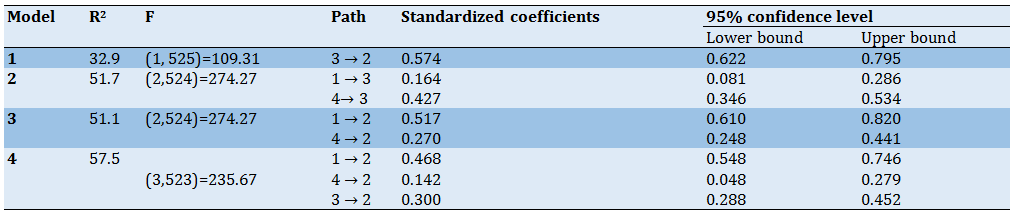
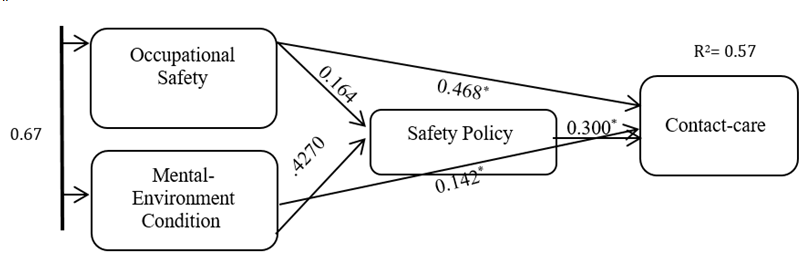
Figure 1) The relation between factors and the final model of the stress of exposure to sharps injury in Iranian nurses (N=527)
Discussion
A healthy and safe workplace is the most valuable asset in different communities [17]. In the theoretical model of the stress of exposure to sharps injury in Iranian nurses in this study, the relationship between occupational safety, Safety Policy, MECs, and contact care was determined. The study results also suggested that Safety Policy could mediate the relationship between these factors.
There was a direct effect between occupational safety and contact care. The consequences of such factors had been also evaluated in some studies. In one survey, the results had demonstrated that the ability to perform occupational safety procedures could be characterized based on attitudes toward risk, leader commitment as a role model, group norms, and beliefs [10]. Moreover, one study had found that safety performance or contact care was positively correlated with autonomy at work and organizational policy perceptions; therefore, nurse managers and hospital administrators had been required to make efforts to upgrade autonomy at work and boost positive perceptions of organizational policy to contribute to improved patient safety [15].
There was an indirect relationship between safety policy and occupational safety and MECs. This highlighted the identification of the interaction between situational and personal factors as a way to promote occupational safety. As well, Safety Policy could contain personal protection protocols and preventive actions against work-related risks. Moreover, these policies needed to be respected by HCWs at healthcare facilities to prevent the extension of infections [18]. The indirect relationship between occupational safety and health climate (namely, MECs) could further influence safety performance [10]. One other survey had similarly revealed that a limited number of nursing assistants and nurses had access to proper personal protective equipment. Unfortunately, the levels of stress in nurses had increased due to lack of special instructions, related to inadequate protective equipment (e.g., masks, face shields, gloves, and goggles) in some wards, individual safety, and work-related incidents [19]. Accordingly, needlestick injuries require immediate medical interventions, which can cause the stress of exposure to sharps injury. Wound disinfection, rapid wound cleaning, determination of the immune status, and if necessary, post-exposure prophylaxes are the most significant actions. Adequate prevention training related to post-injury care is also necessary for healthcare situations. All HCWs should thus know how to manage needlestick injuries. In addition, checkups are required for up to six months after exposure. Information about the infectious condition of the index case can extremely facilitate this process [9].
The fact that occupational safety, as one of the most important factors, could affect the levels of stress in nurses was investigated. Improving the environment of wards, vaccination, and the use of safety gloves and needlestick-protection devices concerning safety aspects could thus reduce the infection risk [20]. The studies in this field had documented that the high prevalence rate of needlestick injuries among HCWs was related to inadequate occupational safety services, lack of safety devices, and no standard precautions to diminish and prevent needlestick injuries. Organizational strategies to prevent exposure are thus essential to minimize the risk of such injuries and post-exposure prophylaxes. Besides, follow-ups to lower the risk of possible infections among HCWs and poor work routines have been so far suggested as factors contributing to needlestick injury prevention [5, 21].
A suitable and effective reporting system can be also an important factor. However, one study had reported that records had been most often about the cases with an important exposure and other exposures had not been documented [22]. Here, high anxiety scores would be attributed to inadequate treatment measures against exposures. Previous studies in Korea had further reported that the levels of anxiety could be higher when HCWs had not been vaccinated [23]. Vaccination and its continuation is thus an important subset of occupational safety. The research findings in this field accordingly call for comprehensive health and injection safety programs for HCWs involved in clinical practices, especially in developing countries [4, 24].
The stress related to MECs also cover the organizational climate caused by stressful working conditions, working in hazardous conditions, high-risk wards, being threatened and reprimanded, the insufficient number of nurses and medical devices in the workplace, distractions at work, heavy workload, poor organization, multiple or repeated attempts to complete some procedures, less experienced nurses, and burnout, as reported in previous studies [21, 25].
Finally, safety policy was investigated as a mediator between other three factors, i.e., occupational safety, contact care, and MECs. These results also had practical implications for organizations’ efforts to provide and implement SPs, indicating that safety interventions and programs needed to be considered as key targets. Moreover, the study results supported the mediating role of this factor in the theoretical model, demonstrating that safety attitudes among HCWs could partially mediate the relationship between safety knowledge and behaviors [14].
In additions, results of the study [26] showed that safety scales could predict injuries and this relationship could be mediated by safety performance. Moreover, this study demonstrated relationships between personality, safety performance, injuries, training, and organizational safety culture.
The limitation of the present study was the use of a cross-sectional approach. Time management was done by the researcher to ensure the accuracy and trustworthiness of the results. The participants completed the questionnaire during their rest time. It is recommended in future studies that Special attention should be paid to the development and evaluation of the subsets of safety policy to reduce the levels of stress in nurses about contact care, which could be further affected by occupational safety as well as mental-environmental conditions.
Conclusion
Safety Policy is a mediator, playing an important role in the model of the stress of exposure to sharps injury.
Acknowledgments: We wish to acknowledge of Mazandaran University of Medical Science. The authors hereby would like to extend their gratitude to all those who participated in this study and appreciate the Clinical Research Development Unit of Baqiyatallah Hospital affiliated to Baqiyatallah University of Medical Sciences, Tehran, Iran.
Ethical Permissions: The study was approved by the ethical committee of Mazandaran University of Medical Sciences (Ethical Code: IR. MAZUMS. REC.1399.6954. Approved Code: 6954).
Conflicts of Interests: -
Authors’ Contributions: Sharif Nia H. (First Author), Statistical Analyst (25%); Mahmoudi H. (Second Author), Introduction Writer (15%); Ebadi A. (Third Author) Methodologist (20%); Moayed M.S. (Fourth Author), Discussion writer/Main Researcher (40%).
Funding/Support: Mazandaran University of Medical Science was supported this study.
Nurses and other healthcare workers (HCWs) are at risk of exposure to bloodborne pathogens, drops, and secretions that potentially result in infections every day while caring for patients [1]. The incidence rates of sharps injuries have been thus reported ranging from 1.4 to 9.5 per 100 HCWs [2]. However, modern technologies have allowed for conducting many laboratory tests and diagnostic procedures at the bedside particularly in critical care units (i.e., cardiac care units (CCUs) and intensive care units (ICUs)), operating rooms, and emergency departments (EDs), whose tests can be consequently achieved faster and an appropriate and immediate treatment can be further started as soon as possible. Although such technologies are useful for patients, the risks of injuries have thus far had a rising trend among nurses [3]. The consequences of diseases transmitted by blood-to-blood contact are not merely limited to such infections, but nurses might suffer from higher levels of anxiety and stress based on their perceptions of the risk of needlestick injuries and predicting others’ reactions [4]. They are frequently subjected to unpleasant thoughts, impaired mental focus, sleep disturbances, anger, and even low sex drive. As a motivating factor, this experience can thus exacerbate all previous mental problems [5].
In this sense, contact care, safety policy, occupational safety, as well as mental-environmental conditions (MECs) are among the most important factors shaping the levels of stress in nurses [6]. Direct or indirect patient contact is also one of the significant factors that can affect nurses’ performance and psychological conditions. The uncertainty of infections transmitted by needlestick injuries or other patient secretions might accordingly raise anxiety in HCWs, especially when patients have been known to be burdened with chronic viral infections and thus much time has been spent on direct contact with them [5, 7, 8]. In Safety Policy, HCWs have obligations to themselves and their patients to work safely [9, 10]. In one study, the highest levels of needlestick-related stress had been thus reported in nurses regarding this factor [11]. On the other hand, Safety Policy statements to prevent the transmission of such infections require robust and well-standardized infection control programs within healthcare delivery systems. The use of needlestick-prevention devices by nurses was accordingly suggested in the World Health Organization guidelines in 2016 [10]. In this sense, providing needle safety equipment in the clinical workplace combined with satisfactory training can significantly reduce the number of occupationally exposed needlestick injuries [12]. Vaccines as a means to prevent and eradicate bloodborne infectious diseases can be further developed [13]. occupational safety can thus refer to having an efficient vaccination schedule as well as sufficient skills in injury prevention and practicing timely treatment in case of injury with sharp objects [6]. One strategy to improve occupational safety is the identification of interactions between personal and situational factors [14]. MECs also represent the conditions nurses are working in, reprimands after injuries, services provided to patients in different situations that can increase the risk of injuries, and other situations that affect the mental status of nurses [6]. In one study, the role of safety climate and culture in enhancing safety performance in 31 selected studies had been evaluated, in which increasing the levels of safety climate and culture had diminished injuries and enriched safety performance indicators [15]. The theoretical model developed here (comprised of occupational safety, contact care, Safety Policy, and MECs) is thus a comprehensive model that includes not only organizational factors but also individual and environmental ones, in which failure to comply with any of these items, as well as deficiency, disturbance, or lack of the subsets of each one can cause the stress of exposure to sharp objects in nurses.
No study has so far investigated the relationship between these factors and their mediating role. Therefore, this path analysis was fulfilled to test a theoretical model to reflect on the relationship between safety policy, occupational safety, mental-environmental conditions, and contact care.
Instrument and Methods
This predictive cross-sectional study was conducted during the August 2018 to May 2019 on nurses of 4 provinces of Iran. The cluster sampling method was used to select 11 hospitals in 4 provinces in Iran, including Tehran (n=4), Kerman (n=2), Isfahan (n=3), and Shiraz (n=2). All the nurses (n=530), who have at least one year of work experience (in EDs, CCUs, and ICUs for pediatrics, neonates, open-heart surgery, surgery, internal medicine, and neurology as well as hemodialysis, surgery, and internal wards) with no history of severe stress such as the death of relatives were included in this study based on the convenience sampling method.
The data were further collected by a two-part questionnaire, containing demographic information (such as age, gender, marital status, level of education, and work experience) and the Stress of Exposure to Sharps Injury Scale [6] consisting of 20 closed statements scored using a 5-point Likert scale (very high=5, high=4, average=3, low=2, very low=1), wherein the maximum and minimum total scores could be 100 and 20, respectively. The scale has four dimensions including safety policy (5 items), occupational safety (5 items), contact care (4 items), and MECs (6 items). This self-report scale had been designed and its psychometric properties had been determined in 2014 [6]. Moreover, the test-retest reliability method was utilized to measure the scale consistency. Accordingly, 20 nurses completed this scale twice with a two-week interval. The reliability of this scale with Cronbach’s alpha was 0.89 and its intraclass correlation coefficient (ICC) was 0.9.
The study was approved by the ethical committee of Mazandaran University of Medical Sciences.
A path analysis was utilized to measure the effect of the factors on Contact Care by IBM SPSS Amos 24.0 software.
Findings
Three of the nurses were excluded from the study because some of the questions were not responded. More than half of the participants were female and married. Their mean age was 35.72±7.78 years, and the mean of work experience was 12.05±8.02 years (Table 1).
The correlation matrix between variables showed that the relationship between all variables included Occupational Safety (Mean±SD=16.78±5.49), Safety policy (Mean±SD=14.20±4.32), MECs (Mean±SD=14.31±3.61) with Contact care (Mean±SD=13.08±4.81) were statistically significant (Table 2).
Path analysis showed that all factors were positive and had significant effects on each other (Table 3;
Figure 1). In the final model of the stress of exposure to needlestick injury, safety policy has mediated between occupational safety, MECs, and contact care. This final model provided an acceptable fit for the data (χ2=1.02; p=0.007; CFI=0.989; TLI=0.936; IFI=0.975; RMSEA=0.032), with all individual paths significant at p<0.05 (Figure 1).
Table 1) Demographic characteristic of participants (N=527)
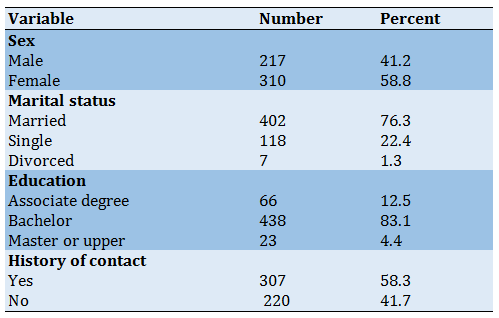
Table 2) Results of the correlation coefficient between factors (p<0.01)
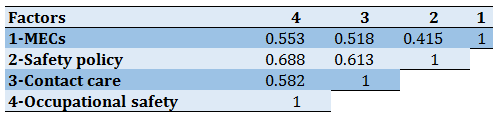
Table 3) Direct and indirect relationship between variables (p<0.001 for all)
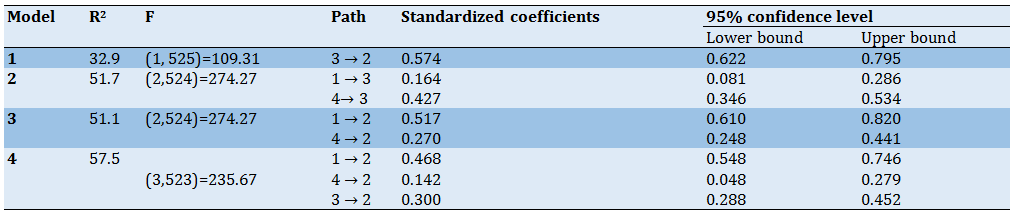
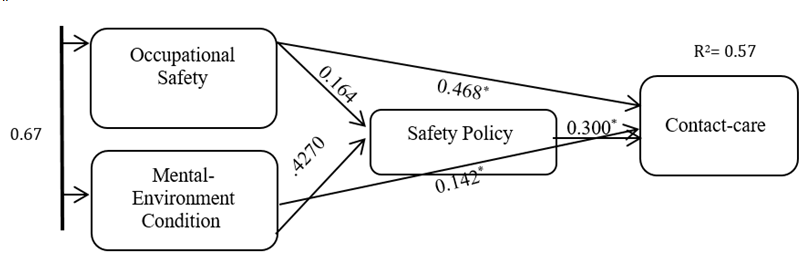
Figure 1) The relation between factors and the final model of the stress of exposure to sharps injury in Iranian nurses (N=527)
Discussion
A healthy and safe workplace is the most valuable asset in different communities [17]. In the theoretical model of the stress of exposure to sharps injury in Iranian nurses in this study, the relationship between occupational safety, Safety Policy, MECs, and contact care was determined. The study results also suggested that Safety Policy could mediate the relationship between these factors.
There was a direct effect between occupational safety and contact care. The consequences of such factors had been also evaluated in some studies. In one survey, the results had demonstrated that the ability to perform occupational safety procedures could be characterized based on attitudes toward risk, leader commitment as a role model, group norms, and beliefs [10]. Moreover, one study had found that safety performance or contact care was positively correlated with autonomy at work and organizational policy perceptions; therefore, nurse managers and hospital administrators had been required to make efforts to upgrade autonomy at work and boost positive perceptions of organizational policy to contribute to improved patient safety [15].
There was an indirect relationship between safety policy and occupational safety and MECs. This highlighted the identification of the interaction between situational and personal factors as a way to promote occupational safety. As well, Safety Policy could contain personal protection protocols and preventive actions against work-related risks. Moreover, these policies needed to be respected by HCWs at healthcare facilities to prevent the extension of infections [18]. The indirect relationship between occupational safety and health climate (namely, MECs) could further influence safety performance [10]. One other survey had similarly revealed that a limited number of nursing assistants and nurses had access to proper personal protective equipment. Unfortunately, the levels of stress in nurses had increased due to lack of special instructions, related to inadequate protective equipment (e.g., masks, face shields, gloves, and goggles) in some wards, individual safety, and work-related incidents [19]. Accordingly, needlestick injuries require immediate medical interventions, which can cause the stress of exposure to sharps injury. Wound disinfection, rapid wound cleaning, determination of the immune status, and if necessary, post-exposure prophylaxes are the most significant actions. Adequate prevention training related to post-injury care is also necessary for healthcare situations. All HCWs should thus know how to manage needlestick injuries. In addition, checkups are required for up to six months after exposure. Information about the infectious condition of the index case can extremely facilitate this process [9].
The fact that occupational safety, as one of the most important factors, could affect the levels of stress in nurses was investigated. Improving the environment of wards, vaccination, and the use of safety gloves and needlestick-protection devices concerning safety aspects could thus reduce the infection risk [20]. The studies in this field had documented that the high prevalence rate of needlestick injuries among HCWs was related to inadequate occupational safety services, lack of safety devices, and no standard precautions to diminish and prevent needlestick injuries. Organizational strategies to prevent exposure are thus essential to minimize the risk of such injuries and post-exposure prophylaxes. Besides, follow-ups to lower the risk of possible infections among HCWs and poor work routines have been so far suggested as factors contributing to needlestick injury prevention [5, 21].
A suitable and effective reporting system can be also an important factor. However, one study had reported that records had been most often about the cases with an important exposure and other exposures had not been documented [22]. Here, high anxiety scores would be attributed to inadequate treatment measures against exposures. Previous studies in Korea had further reported that the levels of anxiety could be higher when HCWs had not been vaccinated [23]. Vaccination and its continuation is thus an important subset of occupational safety. The research findings in this field accordingly call for comprehensive health and injection safety programs for HCWs involved in clinical practices, especially in developing countries [4, 24].
The stress related to MECs also cover the organizational climate caused by stressful working conditions, working in hazardous conditions, high-risk wards, being threatened and reprimanded, the insufficient number of nurses and medical devices in the workplace, distractions at work, heavy workload, poor organization, multiple or repeated attempts to complete some procedures, less experienced nurses, and burnout, as reported in previous studies [21, 25].
Finally, safety policy was investigated as a mediator between other three factors, i.e., occupational safety, contact care, and MECs. These results also had practical implications for organizations’ efforts to provide and implement SPs, indicating that safety interventions and programs needed to be considered as key targets. Moreover, the study results supported the mediating role of this factor in the theoretical model, demonstrating that safety attitudes among HCWs could partially mediate the relationship between safety knowledge and behaviors [14].
In additions, results of the study [26] showed that safety scales could predict injuries and this relationship could be mediated by safety performance. Moreover, this study demonstrated relationships between personality, safety performance, injuries, training, and organizational safety culture.
The limitation of the present study was the use of a cross-sectional approach. Time management was done by the researcher to ensure the accuracy and trustworthiness of the results. The participants completed the questionnaire during their rest time. It is recommended in future studies that Special attention should be paid to the development and evaluation of the subsets of safety policy to reduce the levels of stress in nurses about contact care, which could be further affected by occupational safety as well as mental-environmental conditions.
Conclusion
Safety Policy is a mediator, playing an important role in the model of the stress of exposure to sharps injury.
Acknowledgments: We wish to acknowledge of Mazandaran University of Medical Science. The authors hereby would like to extend their gratitude to all those who participated in this study and appreciate the Clinical Research Development Unit of Baqiyatallah Hospital affiliated to Baqiyatallah University of Medical Sciences, Tehran, Iran.
Ethical Permissions: The study was approved by the ethical committee of Mazandaran University of Medical Sciences (Ethical Code: IR. MAZUMS. REC.1399.6954. Approved Code: 6954).
Conflicts of Interests: -
Authors’ Contributions: Sharif Nia H. (First Author), Statistical Analyst (25%); Mahmoudi H. (Second Author), Introduction Writer (15%); Ebadi A. (Third Author) Methodologist (20%); Moayed M.S. (Fourth Author), Discussion writer/Main Researcher (40%).
Funding/Support: Mazandaran University of Medical Science was supported this study.
Article Type: Original Research |
Subject:
Health Promotion Approaches
Received: 2021/06/5 | Accepted: 2021/10/29 | Published: 2022/04/10
Received: 2021/06/5 | Accepted: 2021/10/29 | Published: 2022/04/10
References
1. Abd El Satter R, Ibrahim Abd Al-Moniem I, Amin Morsy M. Effect of a blood-borne diseases prevention program on nurses' performance in Pediatric Critical Care Units. Egypt J Health Care. 2019;10(3):22-36. [Link] [DOI:10.21608/ejhc.2019.46249]
2. Elseviers MM, Arias‐Guillén M, Gorke A, Arens HJ. Sharps injuries amongst healthcare workers: review of incidence, transmissions and costs. J Renal Care. 2014;40(3):150-6. [Link] [DOI:10.1111/jorc.12050]
3. Akande T. Point-of-care testing (POCT): implementation and management in healthcare services. J Adv Med Med Res. 2018:1-5. [Link] [DOI:10.9734/JAMMR/2018/43875]
4. Matsubara C, Sakisaka K, Sychareun V, Phensavanh A, Ali M. Anxiety and perceived psychological impact associated with needle stick and sharp device injury among tertiary hospital workers, Vientiane, Lao PDR. Ind Health. 2020;58(4):388-396. [Link] [DOI:10.2486/indhealth.2019-0088]
5. Wicker S, Stirn A, Rabenau H, Von Gierke L, Wutzler S, Stephan C. Needlestick injuries: causes, preventability and psychological impact. Infection. 2014;42(3):549-52. [Link] [DOI:10.1007/s15010-014-0598-0]
6. Moayed MS, Mahmoudi H, Ebadi A, Salari M. Needlestick stress in nurses: A questionnaire development. Intl J Cur Life Sci. 2014;4(12):12865-70. [Link]
7. Sharew NT, Mulu GB, Habtewold TD, Gizachew KD. Occupational exposure to sharps injury among healthcare providers in Ethiopia regional hospitals. Ann Occup Environ Med. 2017;29:7. [Link] [DOI:10.1186/s40557-017-0163-2]
8. Broussard IM, Kahwaji CI. Treasure Island (FL); Universal precautions. Unknown city: StatPearls Publishing LLC; 2021. [Link]
9. Moayed MS, Mahmoudi H, Ebadi A, Salary MM, Danial Z. Effect of education on stress of exposure to sharps among nurses in emergency and trauma care wards. Trauma monthly. 2015;20(2):e17709. [Link] [DOI:10.5812/traumamon.20(2)2015.17709]
10. Cheetham S, Ngo H, Liira J, Lee E, Pethrick C, Andrews A, et al. Education and devices to prevent blood and body fluid exposures. Occup Med. 2020;70(1):38-44. [Link] [DOI:10.1093/occmed/kqz156]
11. Moayed MS, Mahmoudi H, Ebadi A, Nia HS. Stress and fear of exposure to sharps in nurses. Iranian J Psychiatry Behav Sci. 2016;10(3):e3813. [Link] [DOI:10.17795/ijpbs-3813]
12. Bianco V, Spera AM, Maraolo AE, Parente S, Donno D, Moriello NS, et al. Risk of professional accidental exposure to biological agents in health care workers: A retrospective analysis carried out in a southern Italian tertiary hospital. Infez Med. 2019;27(1):40-5. [Link]
13. Szollosi DE, Mathias CB, Lucero V, Ahmad S, Donato J. Immunopathogenesis, Immunization, and Treatment of Infectious Diseases. In: Mathias CB, McAleer JP, Szollosi DE, editors.Pharmacology of Immunotherapeutic Drugs. Berlin: Springer; 2020. p. 277-319. [Link] [DOI:10.1007/978-3-030-19922-7_9]
14. Kao K-Y, Spitzmueller C, Cigularov K, Thomas CL. Linking safety knowledge to safety behaviours: a moderated mediation of supervisor and worker safety attitudes. Eur J Work Organiz Psychol. 2019;28(2):206-20. [Link] [DOI:10.1080/1359432X.2019.1567492]
15. Kalteh HO, Mortazavi SB, Mohammadi E, Salesi M. The relationship between safety culture and safety climate and safety performance: a systematic review. Int J Occup Saf Ergon. 2021;27(1):206-16. [Link] [DOI:10.1080/10803548.2018.1556976]
16. Rucker DD, Preacher KJ, Tormala ZL, Petty RE. Mediation analysis in social psychology: Current practices and new recommendations. Soc Person Psychol Compass. 2011;5(6):359-71. [Link] [DOI:10.1111/j.1751-9004.2011.00355.x]
17. Staun JMC. Occupational health nursing and the European dimension. Workplace Health Saf. 2012;60(3):122-6. [Link] [DOI:10.1177/216507991206000307]
18. Almost JM, VanDenKerkhof EG, Strahlendorf P, Caicco Tett L, Noonan J, Hayes T, et al. A study of leading indicators for occupational health and safety management systems in healthcare. BMC Health Serv Res. 2018;18(1):1-7. [Link] [DOI:10.1186/s12913-018-3103-0]
19. Katanami Y, Hayakawa K, Shimazaki T, Sugiki Y, Takaya S, Yamamoto K, et al. Adherence to contact precautions by different types of healthcare workers through video monitoring in a tertiary hospital. J Hosp Infect. 2018;100(1):70-5. [Link] [DOI:10.1016/j.jhin.2018.01.001]
20. Ochmann U, Wicker S. Needlestick injuries of healthcare workers. Medizinische Klinik, Intensivmedizin und Notfallmedizin. 2020;115(1):67-78. [Link] [DOI:10.1007/s00063-019-00651-5]
21. Kebede G, Molla M, Sharma HR. Needle stick and sharps injuries among health care workers in Gondar city, Ethiopia. Saf Sci. 2012;50(4):1093-7. [Link] [DOI:10.1016/j.ssci.2011.11.017]
22. Mahajan S, Gupta E. Needle stick injury in healthcare workers. Indian J Health Sci Care. 2019;6(2):80-91. [Link] [DOI:10.5958/2394-2800.2019.00016.6]
23. Sohn JW, Kim BG, Kim SH, Han C. Mental health of healthcare workers who experience needlestick and sharps injuries. J Occup Health. 2006;48(6):474-9. [Link] [DOI:10.1539/joh.48.474]
24. Matsubara C, Sakisaka K, Sychareun V, Phensavanh A, Ali M. Prevalence and risk factors of needle stick and sharp injury among tertiary hospital workers, Vientiane, Lao PDR. J Occup Health. 2017:59(6):581-5. [Link] [DOI:10.1539/joh.17-0084-FS]
25. Clarke SP, Rockett JL, Sloane DM, Aiken LH. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. Am J Infect Control. 2002;30(4):207-16. [Link] [DOI:10.1067/mic.2002.123392]
26. Hogan J, Foster J. Multifaceted personality predictors of workplace safety performance: More than conscientiousness. Human Perform. 2013;26(1):20-43. [Link] [DOI:10.1080/08959285.2012.736899]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





