Volume 9, Issue 3 (2021)
Health Educ Health Promot 2021, 9(3): 209-220 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Samimi T, MohammadEbrahimi S, Tara F, Mostafavi S, Ebrahimi Miandehi E, Tara M. Improving Information Adequacy of Clinical Morning Reports; Development of a Structured Model in the Obstetrics and Gynecology Department. Health Educ Health Promot 2021; 9 (3) :209-220
URL: http://hehp.modares.ac.ir/article-5-51452-en.html
URL: http://hehp.modares.ac.ir/article-5-51452-en.html
1- Department of Medical Informatics, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
2- Department of Obstetrics and Gynecology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
3- Department of Medical Informatics, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran ,taram@mums.ac.ir
2- Department of Obstetrics and Gynecology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
3- Department of Medical Informatics, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran ,
Keywords: Morning Report [MeSH], Medical Education [MeSH], Obstetrics [MeSH], Gynecology [MeSH], Iran [MeSH]
Full-Text [PDF 1233 kb]
(3665 Downloads)
| Abstract (HTML) (2243 Views)
Table 3) The current status survey in hospitals A, B, and C
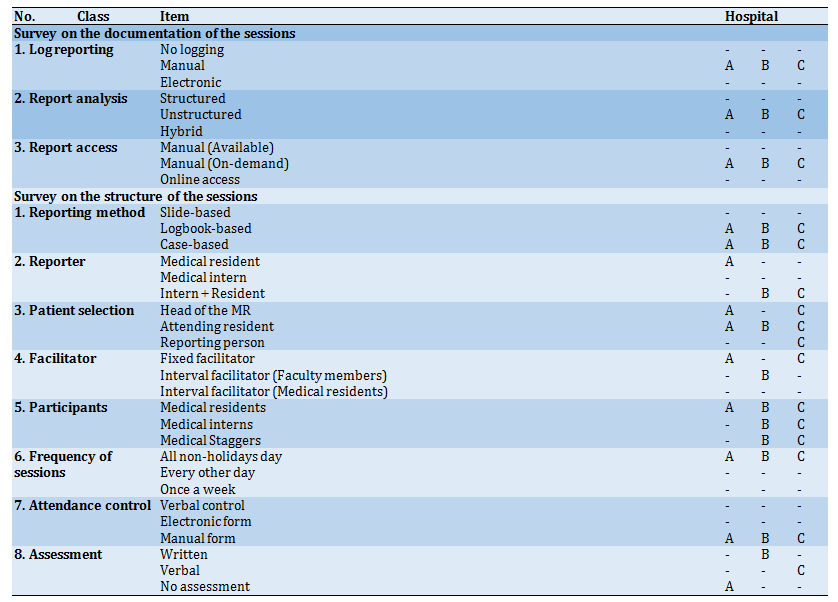
Table 4) Delphi's first-round; Experts agreement quotient and new items suggestion
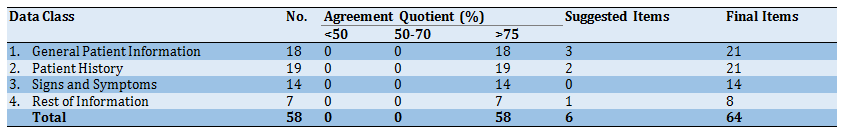
Table 5) Delphi's second-round; scoring the items using the 5-point Likert Scale by ten experts
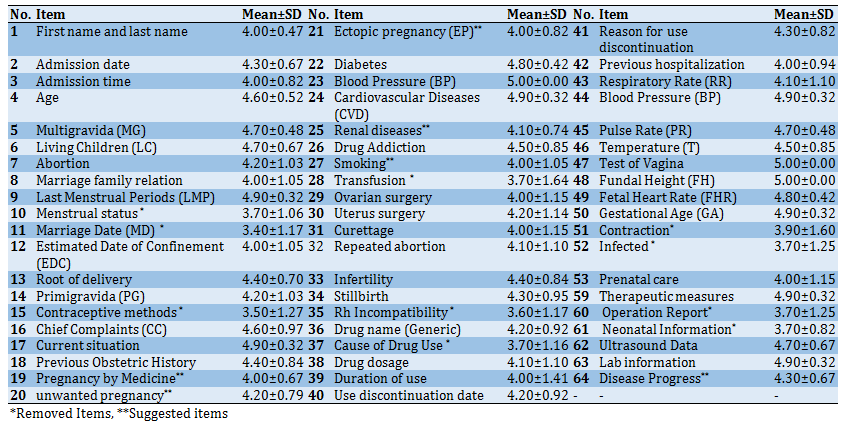
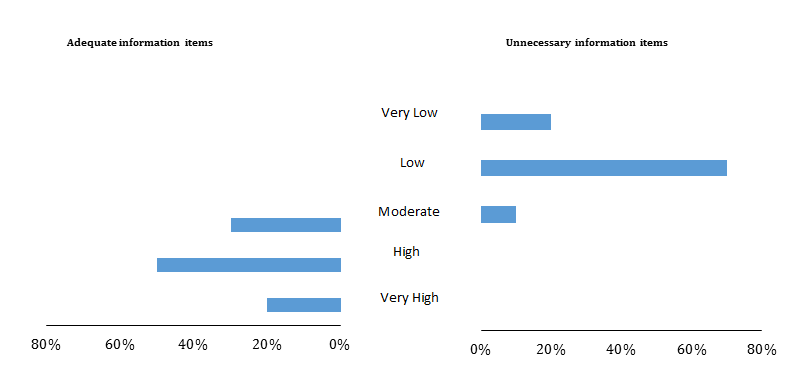
Diagram 1) Results of investigating adequate and unnecessary information items in structured morning reporting model

Diagram 2) Comparison assessment of all three formats
Full-Text: (1064 Views)
Introduction
Clinical education is considered the heart of medical education, emphasizing individualized patient-related issues [1]. Much of the educational process for medical students is done in real-world settings and through interaction with patients. As such, clinical education is fundamentally different from teaching in other disciplines [2]. Matching theoretical knowledge with objective examples helps the learning process and long-term memorization of teaching material. Patient-based learning helps students correct their theoretical knowledge misconceptions and reinforces the right ones [3]. Among the different methods of clinical education, morning report (MR) is the most widely used routine in the world [2]. A standard morning report is a session attended by clinical professors, their assistants, and the interns and externs focused on presenting selected clinical cases from the most recent admissions, particularly the ones from the last 24 hours [4].
Morning reports are practiced in various ways using different locally to globally known methods. MRs cover a wide range of activities, including an overall report of recent clinical events, analysis of various differential diagnoses and the choices of therapeutic, evaluation of residents' performance, assessment of the care provided to patients, identification and discussion of potential adverse events, and managing case-based controversies [5]. The main purpose of MR sessions is to discuss clinical cases and, subsequently, master how to make an informed clinical decision [6].
The MR format may vary from institute to institute, but they all share some common features. For instance, there is often a case-based presentation, during which a case is discussed from various angles and perspectives. Over the years, various learning approaches have attempted to improve the case-based presentation in MR sessions [5]. Research has shown that structuring clinical report improves the quality [7], reduces ambiguity, and increases accuracy, clarity, and value of clinical documents [8]. Although preparing structured clinical reports is a considerably time-demanding process for physicians as compared to the choice of free-text format, evidence has shown that, in the end, such reports are the most satisfying forms to the medical team [9].
Literature shows little evidence regarding attempts to propose structures for morning report case presentation items, while there seems to be no doubt that a coherent, structured report form with expert-agreed information items would make immersive improvements. This study aimed to improve clinical morning reports' information adequacy by developing a structured reporting model.
Participants & Methods
This qualitative study included the investigation of information adequacy and also development, validation, and evaluation of a model to produce structured clinical morning reports was conducted at the Department of Obstetrics and Gynecology of three teaching hospitals in northeastern Iran including Om-al-Banin, Ghaem, and Emam-Reza in 2018. This structured report is developed in two separate formats, and the study was conducted in three phases, as follows.
Phase I: Studying the current status of MR documentations
In the first phase, a survey was conducted to examine the current quality of MR documentation in the participating hospitals. For this purpose, a checklist was developed in two sections focusing on the structure and documentation of clinical MR sessions, borrowing items from previous studies [5, 10, 11], followed by an expert panel check and verification step. The initially developed checklist was completed by three gynecologists and obstetricians in charge of MR session management at the time of research conduction in the three mentioned hospitals.
A total of 120 MR reports were selected based on random sampling among the currently available reports within the report archive. All reports were in "free-text" format. Every report was thoroughly read and analyzed to extract informational items.
In the next stage, the list of extracted items was provided to the four members of the panel (Table 1; involved experts: C01, C02, C03, C04).
After review by the panel, all extracted items were approved and subsequently classified into four thematic categories. The pre-approved list of items and categories were then shared for two rounds of enhancement and approval of a modified Delphi technique as follow:
A) In the first round, all final items were assessed by ten clinical experts from the participating hospitals; none was part of the expert panel. Table 2 showed the general characteristics of the experts who participated in the Delphi study. Each item was allowed to be tagged for removal or to be kept based on the agreement quotient. Accordingly, the items with greater than 75% agreement quotient were kept in the first round and were not passed to the second round. The items with a 50% to 75% agreement quotient were reassessed in the second round, and items with an agreement quotient of below 50% were omitted. After the end of the first round, all extracted items obtained more than 75% agreement quotient. However, new items were also suggested by experts.
B) In the second round, clinical experts were requested to score the value of each item. Accordingly, the Likert Scale was used in a discrete and typical format of an interval scale, ranging from one (strongly disagree) to five (strongly agree). Then, the mean±SD of scores for each item was calculated, and then a cut-off point was selected. The mean scores below this point were those items that were to be removed from the list.
Phase II: Developing a Structured Model for Clinical Morning Reports
In this phase, a structured model of clinical MR was developed based on the previously validated items. This model was created in two formats: structured paper-based form (SPF) and structured electronic format (SEF). The SPF format was developed in two parts: general and specific. In the first part, based on the opinions of the two expert panel members (Table 1; Involved experts: C01, C02), the general information items for report forms were added. The specific part included all confirmed items from the Delphi technique, like general patient information, previous obstetric history, disease background, surgical history, obstetrics history, drug use history, previous hospitalization, signs and symptoms, lab information, ultrasound data, as well as an attachment option for clinical images (Appendix 1).
In order to create the SEF format, an electronic version of the SPF was produced using Windows-based software built using Microsoft Visual Studio 2010. Additionally, we built an MR SEF archive using Microsoft SQL Server 2008 Database and Stimulsoft Reports 2010 software.
The face and content validity of the developed structured forms were checked by three members of the expert panel (Table 1; involved experts: C01, C02, C03). As a result, some item classes were revised, and some items of the initial form were merged, split, or replaced.
Phase III: Evaluation of the proposed model
In order to evaluate the quality of the proposed structure model, a questionnaire was designed by researchers consisted of two sections. Section 1 was aimed at measuring the adequacy of the finally selected items, and Section 2 was focused on the comparative assessment between the three clinical MR formats (conventional, SPF, and SEF), in terms of readability, clarity of patient status, ease of reporting, future research application, ease of archiving and retrieval, and preference for use. Both sections were using independent questions. The questionnaire was initially provided to the expert panel members (Table 1; Involved experts: C03, C04, C05) for review and approval.
A total of 16 MR documents were selected based on the opinions of the consulting experts containing different scenarios. Afterward, the reports older than three months were taken into consideration.
To prepare the three formats, the same residents in charge of the original report were asked to produce the SPF format for the same patients. Later, the research team produced the SEF format of each report using the completed SPF content.
For the final evaluation, all three formats, including the SPF, SEF, and the conventional formats, were shared with the selected experts for comparison and evaluation. Overall, sixteen MR documents in three formats (n=48) were provided to 20 residents of Obstetrics and Gynecology in the participating hospitals (excluding those who participated in previous tasks) along with the designed questionnaire.
Excel 2010 software was used for the analysis of the results.
Table 1) The expert-panel characteristics with identification codes

Table 2) General information about the experts who participated in the items validation stage (n=10)

Findings
Survey of Current Status
The survey results showed that the current MR documentation in all three hospitals was based on non-structured case-based reports reflecting on the patients' logbooks (Table 3).
Items extraction, validation, and categorization
Fifty-eight information items were extracted from 120 reports. They were then validated and categorized by ten experts into four categories using the two-round Delphi technique. In the first round, all items with a score above 75% entered the second round. Experts also suggested six new items in this round, and a total of 64 items was achieved
(Table 4).
In the second round, the experts scored the 64 items using a 5-point Likert Scale. An initial investigation of the assigned scores showed that the scores did not follow a scattered pattern, and therefore, calculation of the mean score was practical. Accordingly, a cut-off point of 4 was set, and the items with a lower score were omitted.
Table 5 shows the mean±SD of the scores assigned to each item. "Test of Vagina" and "Fundal Height" from the "Signs and Symptoms" category and "Blood Pressure" from the "Patient History" category were assigned the perfect score (5.00±0.00). Based on the cut-off point of 4, "Menstrual Status" (3.70±1.06), "Date of Marriage" (3.40±1.17), and "Contraceptive Methods" (3.50±1.27) from the category of "General Patient Information", "Transfusion" (3.70±1.64), "Rh Incompatibility" (3.60±1.17), and "Cause of Drug Use" (3.70±1.16) from the "Patient History" category, "Contraction" (3.90±1.6), "Infected" (3.70±1.25) and "Estimated Fetal Weight" (3.70±0.95) from the "Signs and Symptoms" category, and also "Operation Report" (3.70±1.25) and "Neonatal Information" (3.7±0.82) from the category of "Rest of Information", were removed based on the selected cut-off.
Structured Model of Clinical Morning Report
The structured clinical MR model was designed in two sections. The first section included general information about the MR, and the second section contained patient-specific information. As shown in Appendix 2, the structured report consisted of 64 items classified into eleven categories based on experts' opinions.
Model Evaluation
Initial Structure Evaluation
In the initial evaluation of the structured model of MR based on the face and content validity check, the "Gestational Age" item was moved from the "Signs and Symptoms" category to the "General Patient Information" category and then separated into two items of "Gestational Age based on LMP" and "Gestational Age based on Ultrasound". Furthermore, the "Prenatal Care" item from the "Signs and Symptoms" category was moved to the "General Patient Information". To enrich the content of the structured model, appropriate sub-items were defined by two experienced Gynecologists for the items (Table 1; involved experts: C01, C02). Appendix 3 shows the sub-items that were defined for the main items of structured form. Finally, space was added to the structured model for attaching clinical images and entering the individual characteristics of the individual completing the report.
Information Adequacy Evaluation
To assess the information adequacy of the structured MR, the items were assessed from the perspective of adequacy (and non-necessity on the other side) by the residents (n=20) while allowing them to suggest their desired items. Diagram 1 shows that 20% of residents (n=4) rated the adequacy level of the model as very high, 50% (n=10) as high, and 30% (n=6) as moderate. In this part, no assessor classified the items as low or very low. Moreover, 20% of residents (n=4) rated the presence of unnecessary items in the structured MR as very low, 70% (n=14) rated as low, and 10% (n=2) rated as moderate. In this part, no assessor classified the items as high or very high (in non-necessity). It should be noted that at this stage, "PPH (Postpartum Hemorrhage)" item in the "General Information" category, "Start date of use" item in the "Drug use History" category, "Abdominal Examination", "Pelvic Examination", and "Speculum Examination" item in the "Signs and Symptoms" category, and "Non-pregnancy Ultrasound" item in the "Ultrasound Data" category were proposed by the residents.
Comparative Evaluation of All Three Formats
The analysis for the comparative evaluation of all three formats is shown in Diagram 2. Based on this assessment, the SPF format scored highest on the items of "Preference for use" (50%), "Ease of archiving and retrieval" (80%), "Application in future research" (80%), and "ease of reporting" (50%). The SEF format also scored the highest on the two items, including "Clear understanding of patient status" (60%) and "Readability" (75%). The conventional format received a lower score than the other two formats - except for the item of "Preference for use", which had a score between the SPF and SEF (30%).
Clinical education is considered the heart of medical education, emphasizing individualized patient-related issues [1]. Much of the educational process for medical students is done in real-world settings and through interaction with patients. As such, clinical education is fundamentally different from teaching in other disciplines [2]. Matching theoretical knowledge with objective examples helps the learning process and long-term memorization of teaching material. Patient-based learning helps students correct their theoretical knowledge misconceptions and reinforces the right ones [3]. Among the different methods of clinical education, morning report (MR) is the most widely used routine in the world [2]. A standard morning report is a session attended by clinical professors, their assistants, and the interns and externs focused on presenting selected clinical cases from the most recent admissions, particularly the ones from the last 24 hours [4].
Morning reports are practiced in various ways using different locally to globally known methods. MRs cover a wide range of activities, including an overall report of recent clinical events, analysis of various differential diagnoses and the choices of therapeutic, evaluation of residents' performance, assessment of the care provided to patients, identification and discussion of potential adverse events, and managing case-based controversies [5]. The main purpose of MR sessions is to discuss clinical cases and, subsequently, master how to make an informed clinical decision [6].
The MR format may vary from institute to institute, but they all share some common features. For instance, there is often a case-based presentation, during which a case is discussed from various angles and perspectives. Over the years, various learning approaches have attempted to improve the case-based presentation in MR sessions [5]. Research has shown that structuring clinical report improves the quality [7], reduces ambiguity, and increases accuracy, clarity, and value of clinical documents [8]. Although preparing structured clinical reports is a considerably time-demanding process for physicians as compared to the choice of free-text format, evidence has shown that, in the end, such reports are the most satisfying forms to the medical team [9].
Literature shows little evidence regarding attempts to propose structures for morning report case presentation items, while there seems to be no doubt that a coherent, structured report form with expert-agreed information items would make immersive improvements. This study aimed to improve clinical morning reports' information adequacy by developing a structured reporting model.
Participants & Methods
This qualitative study included the investigation of information adequacy and also development, validation, and evaluation of a model to produce structured clinical morning reports was conducted at the Department of Obstetrics and Gynecology of three teaching hospitals in northeastern Iran including Om-al-Banin, Ghaem, and Emam-Reza in 2018. This structured report is developed in two separate formats, and the study was conducted in three phases, as follows.
Phase I: Studying the current status of MR documentations
In the first phase, a survey was conducted to examine the current quality of MR documentation in the participating hospitals. For this purpose, a checklist was developed in two sections focusing on the structure and documentation of clinical MR sessions, borrowing items from previous studies [5, 10, 11], followed by an expert panel check and verification step. The initially developed checklist was completed by three gynecologists and obstetricians in charge of MR session management at the time of research conduction in the three mentioned hospitals.
A total of 120 MR reports were selected based on random sampling among the currently available reports within the report archive. All reports were in "free-text" format. Every report was thoroughly read and analyzed to extract informational items.
In the next stage, the list of extracted items was provided to the four members of the panel (Table 1; involved experts: C01, C02, C03, C04).
After review by the panel, all extracted items were approved and subsequently classified into four thematic categories. The pre-approved list of items and categories were then shared for two rounds of enhancement and approval of a modified Delphi technique as follow:
A) In the first round, all final items were assessed by ten clinical experts from the participating hospitals; none was part of the expert panel. Table 2 showed the general characteristics of the experts who participated in the Delphi study. Each item was allowed to be tagged for removal or to be kept based on the agreement quotient. Accordingly, the items with greater than 75% agreement quotient were kept in the first round and were not passed to the second round. The items with a 50% to 75% agreement quotient were reassessed in the second round, and items with an agreement quotient of below 50% were omitted. After the end of the first round, all extracted items obtained more than 75% agreement quotient. However, new items were also suggested by experts.
B) In the second round, clinical experts were requested to score the value of each item. Accordingly, the Likert Scale was used in a discrete and typical format of an interval scale, ranging from one (strongly disagree) to five (strongly agree). Then, the mean±SD of scores for each item was calculated, and then a cut-off point was selected. The mean scores below this point were those items that were to be removed from the list.
Phase II: Developing a Structured Model for Clinical Morning Reports
In this phase, a structured model of clinical MR was developed based on the previously validated items. This model was created in two formats: structured paper-based form (SPF) and structured electronic format (SEF). The SPF format was developed in two parts: general and specific. In the first part, based on the opinions of the two expert panel members (Table 1; Involved experts: C01, C02), the general information items for report forms were added. The specific part included all confirmed items from the Delphi technique, like general patient information, previous obstetric history, disease background, surgical history, obstetrics history, drug use history, previous hospitalization, signs and symptoms, lab information, ultrasound data, as well as an attachment option for clinical images (Appendix 1).
In order to create the SEF format, an electronic version of the SPF was produced using Windows-based software built using Microsoft Visual Studio 2010. Additionally, we built an MR SEF archive using Microsoft SQL Server 2008 Database and Stimulsoft Reports 2010 software.
The face and content validity of the developed structured forms were checked by three members of the expert panel (Table 1; involved experts: C01, C02, C03). As a result, some item classes were revised, and some items of the initial form were merged, split, or replaced.
Phase III: Evaluation of the proposed model
In order to evaluate the quality of the proposed structure model, a questionnaire was designed by researchers consisted of two sections. Section 1 was aimed at measuring the adequacy of the finally selected items, and Section 2 was focused on the comparative assessment between the three clinical MR formats (conventional, SPF, and SEF), in terms of readability, clarity of patient status, ease of reporting, future research application, ease of archiving and retrieval, and preference for use. Both sections were using independent questions. The questionnaire was initially provided to the expert panel members (Table 1; Involved experts: C03, C04, C05) for review and approval.
A total of 16 MR documents were selected based on the opinions of the consulting experts containing different scenarios. Afterward, the reports older than three months were taken into consideration.
To prepare the three formats, the same residents in charge of the original report were asked to produce the SPF format for the same patients. Later, the research team produced the SEF format of each report using the completed SPF content.
For the final evaluation, all three formats, including the SPF, SEF, and the conventional formats, were shared with the selected experts for comparison and evaluation. Overall, sixteen MR documents in three formats (n=48) were provided to 20 residents of Obstetrics and Gynecology in the participating hospitals (excluding those who participated in previous tasks) along with the designed questionnaire.
Excel 2010 software was used for the analysis of the results.
Table 1) The expert-panel characteristics with identification codes

Table 2) General information about the experts who participated in the items validation stage (n=10)

Findings
Survey of Current Status
The survey results showed that the current MR documentation in all three hospitals was based on non-structured case-based reports reflecting on the patients' logbooks (Table 3).
Items extraction, validation, and categorization
Fifty-eight information items were extracted from 120 reports. They were then validated and categorized by ten experts into four categories using the two-round Delphi technique. In the first round, all items with a score above 75% entered the second round. Experts also suggested six new items in this round, and a total of 64 items was achieved
(Table 4).
In the second round, the experts scored the 64 items using a 5-point Likert Scale. An initial investigation of the assigned scores showed that the scores did not follow a scattered pattern, and therefore, calculation of the mean score was practical. Accordingly, a cut-off point of 4 was set, and the items with a lower score were omitted.
Table 5 shows the mean±SD of the scores assigned to each item. "Test of Vagina" and "Fundal Height" from the "Signs and Symptoms" category and "Blood Pressure" from the "Patient History" category were assigned the perfect score (5.00±0.00). Based on the cut-off point of 4, "Menstrual Status" (3.70±1.06), "Date of Marriage" (3.40±1.17), and "Contraceptive Methods" (3.50±1.27) from the category of "General Patient Information", "Transfusion" (3.70±1.64), "Rh Incompatibility" (3.60±1.17), and "Cause of Drug Use" (3.70±1.16) from the "Patient History" category, "Contraction" (3.90±1.6), "Infected" (3.70±1.25) and "Estimated Fetal Weight" (3.70±0.95) from the "Signs and Symptoms" category, and also "Operation Report" (3.70±1.25) and "Neonatal Information" (3.7±0.82) from the category of "Rest of Information", were removed based on the selected cut-off.
Structured Model of Clinical Morning Report
The structured clinical MR model was designed in two sections. The first section included general information about the MR, and the second section contained patient-specific information. As shown in Appendix 2, the structured report consisted of 64 items classified into eleven categories based on experts' opinions.
Model Evaluation
Initial Structure Evaluation
In the initial evaluation of the structured model of MR based on the face and content validity check, the "Gestational Age" item was moved from the "Signs and Symptoms" category to the "General Patient Information" category and then separated into two items of "Gestational Age based on LMP" and "Gestational Age based on Ultrasound". Furthermore, the "Prenatal Care" item from the "Signs and Symptoms" category was moved to the "General Patient Information". To enrich the content of the structured model, appropriate sub-items were defined by two experienced Gynecologists for the items (Table 1; involved experts: C01, C02). Appendix 3 shows the sub-items that were defined for the main items of structured form. Finally, space was added to the structured model for attaching clinical images and entering the individual characteristics of the individual completing the report.
Information Adequacy Evaluation
To assess the information adequacy of the structured MR, the items were assessed from the perspective of adequacy (and non-necessity on the other side) by the residents (n=20) while allowing them to suggest their desired items. Diagram 1 shows that 20% of residents (n=4) rated the adequacy level of the model as very high, 50% (n=10) as high, and 30% (n=6) as moderate. In this part, no assessor classified the items as low or very low. Moreover, 20% of residents (n=4) rated the presence of unnecessary items in the structured MR as very low, 70% (n=14) rated as low, and 10% (n=2) rated as moderate. In this part, no assessor classified the items as high or very high (in non-necessity). It should be noted that at this stage, "PPH (Postpartum Hemorrhage)" item in the "General Information" category, "Start date of use" item in the "Drug use History" category, "Abdominal Examination", "Pelvic Examination", and "Speculum Examination" item in the "Signs and Symptoms" category, and "Non-pregnancy Ultrasound" item in the "Ultrasound Data" category were proposed by the residents.
Comparative Evaluation of All Three Formats
The analysis for the comparative evaluation of all three formats is shown in Diagram 2. Based on this assessment, the SPF format scored highest on the items of "Preference for use" (50%), "Ease of archiving and retrieval" (80%), "Application in future research" (80%), and "ease of reporting" (50%). The SEF format also scored the highest on the two items, including "Clear understanding of patient status" (60%) and "Readability" (75%). The conventional format received a lower score than the other two formats - except for the item of "Preference for use", which had a score between the SPF and SEF (30%).
Table 3) The current status survey in hospitals A, B, and C
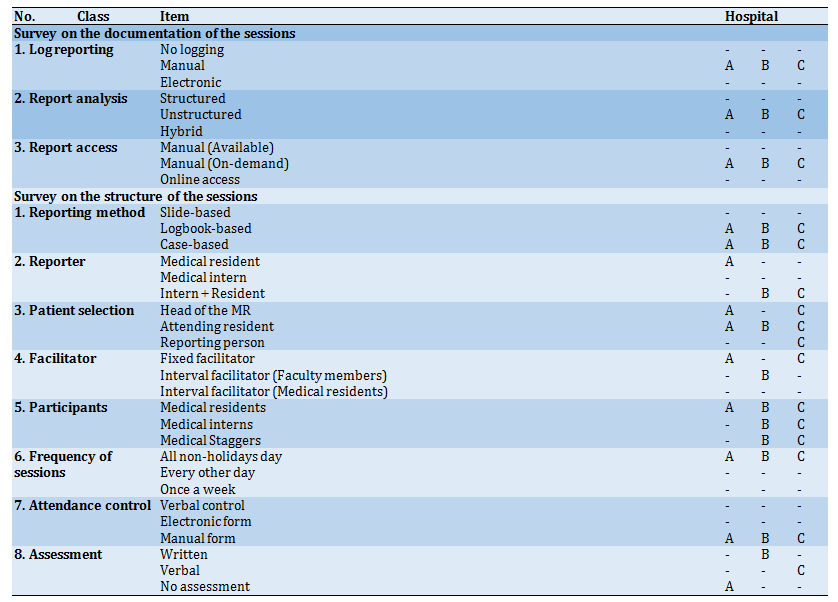
Table 4) Delphi's first-round; Experts agreement quotient and new items suggestion
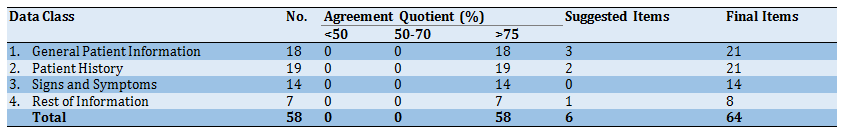
Table 5) Delphi's second-round; scoring the items using the 5-point Likert Scale by ten experts
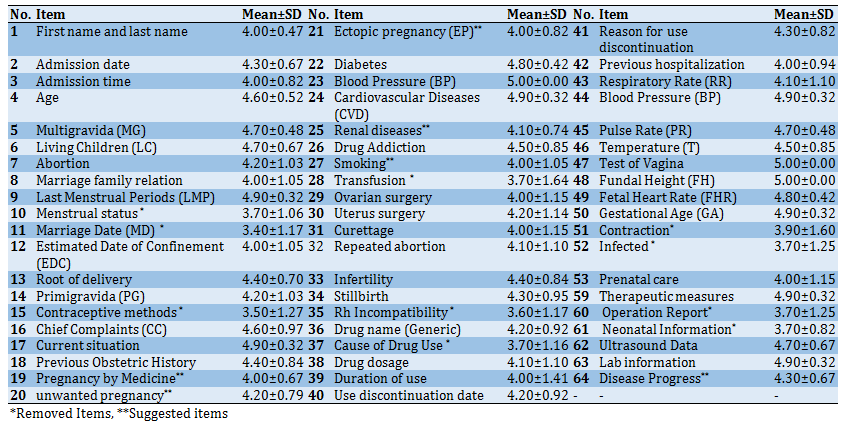
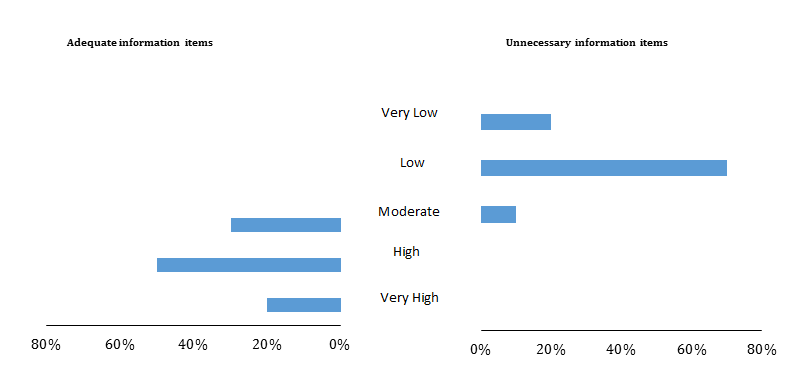
Diagram 1) Results of investigating adequate and unnecessary information items in structured morning reporting model

Diagram 2) Comparison assessment of all three formats
Discussion
This study was aimed to develop a structured model for clinical MR documentation and presentation in the Obstetrics and Gynecology department of three teaching hospitals to improve the overall informational and presentation quality of morning report sessions. The model was developed in two formats: Structured Paper-based Form (SPF) and Structured Electronic Format (SEF). The overall format was developed in two sections: General Information and Patient-specific Information, including 64 items in 11 categories. The prospective users of such a model are gynecological residents in charge of running MR sessions almost every morning.
One of the crucial problems in clinical education is the lack of standardized documentation and, consequently, weakness in evidence-based medicine [12]. We also face problems such as widespread data, high data volume, and poor documentation [13]. Our initial literature review, globally and nationally, showed no evidence of any proposed uniform structure for morning report documentation and presentation. However, there were similarities among the practicing countries (including Iran), such as the number of meetings over a specific period [4, 5, 14], the person in charge of case presentation [14-16], session facilitators [4, 14, 17], the person responsible for patient selection, and type of individuals regularly attending sessions [4, 5, 18].
One of the purposes of MR sessions is to discuss different aspects of patients' diagnosis and therapeutic options. Therefore, avoiding unnecessary information and having adequate and accurate information about patients is indisputable [5, 19]. According to the back-to-back chart regarding information adequacy of the structured form (Diagram 2), 70% of residents estimated the presence of adequate items as high and very high, while 90% estimated the presence of unnecessary items as low and very low. Confirming the results on both sides of the chart showed that the developed structured model reliably covers information items to patients' presentations in the MR sessions. The result of previous similar studies also confirms the results of our study [20-22].
In this study, twenty gynecological residents were provided 16 clinical MRs to compare three formats, including conventional forms, SPF, and SEF (n=48). The results showed that 75% of residents indicated that the SEF format has more readability and 60% considered it a format providing a clearer understanding of patient status. This result can be interpreted as the potential benefits of electronic records as compared to paper formats. In another study, two formats of structured and free-text reporting were compared, evaluating 330 reports by eleven experts from content and clarity. The results showed that an individual's satisfaction and preference for using structured reports were significantly different from unstructured reports [23].
More than half of our residents believed that using the SPF format will facilitate the reporting workflow. In a similar study, eleven experts from eight countries examined structured reports of radiology at the focus group meetings. Similar to our findings, this study concluded that workflow facilitation benefited from using structured reports [24]. Selectivity in creating data elements for recording and collecting data is considered a central part of Medicine Art [25]. Therefore, the selection and use of predefined datasets to generate reports can improve the workflow process of patient reports and data.
According to the results of Ganeshan's study, one of the benefits of structured reporting is its positive impact on research and the facilitation of data mining [26]. The results of another study have also shown that using the structured form is useful for future research [27]. It has also been shown that data mining and integration with decision support systems and clinical guidelines will improve [26]. In the current study, with a significant difference, 80% of residents considered the SPF format a more appropriate option for use in future research studies, which is in line with the results of the studies as mentioned above.
Archiving, maintaining, and retrieving reports documentation is a continuous communication process between clinical care team members that provides information on patients' health care status [28]. This is essential for various educational and assessment purposes during MR sessions but is nevertheless challenging MR sessions [5, 29]. Our study covered this challenge as our initial results showed no standard system to archive and retrieved MR documents (Table 3). In the current study, for 80% of residents, the SPF format was a better option for ease of archiving and information retrieval that could meet the information needs and improve documentation flow. Wrenn et al. used a structured form for patients referring to the emergency department over eight months, in which the results indicated a significant improvement in archiving and retrieval [27]. Since the use of electronic databases can undoubtedly lead to better archiving and retrieval of information sources [30], it seems that the reason for this paradoxical deviation in residents' attitudes towards the paper format is mostly due to its structured appearance rather than the comparable potential values of SEF format, which contains both structure and achievability.
As the results showed, the preferred format for use by half of the residents was SPF, and the other half preferred the conventional format (30%) and the SET format (20%), respectively. This comparison shows that practitioners prefer to use paper forms, whether in structured or free-text formats, compared to computer systems. Using computer systems to enter clinical information is more difficult and less flexible than paper forms [31], and also data entry into the structured electronic form is a more time-demanding process [32]. It is also worth noting that there is no teaching for ten-fingers typing in the Iranian education system, and most residents are no exception. This is a very important observation, which explains why much time is spent on typing, which results in an unwillingness to use electronic systems which require rapid typing. Therefore, it seems that it will speed up reporting and increase the workload and demand more time on the part of residents.
There were some limitations in our study. First, focusing on the opinions of local experts may reduce the generalizability of the developed model universally. However, we believe that the proposed methodology will still be useful in designing a similar local model in other countries. The study also had a limited view in its medical focus on gynecology and obstetrics; however, we find no reason why our core proposition of giving structures to MR documentation could not benefit other departments.
Future studies in this area could take more advanced steps into incorporating automatic production of structured MR from free-text reports using Natural Language Processing (NLP). For this purpose, the obtained structure in this study can be used as a strong basis, particularly in obstetrics and gynecology. We also recommend that future researchers apply our methods to develop similar standards for structuring MR documentation in other areas of clinical specialties.
Conclusion
Investigating the information adequacy of the reports and providing the necessary items for the presentation of cases in the MR sessions can enrich the clinical content and improve the educational and research quality of the reports. From the perspectives of the experts involved in the MR sessions of the gynecology department, the structured model was more valuable than the conventional format in terms of readability, improved documentation, easier archiving and retrieval, and a better understanding of the patient's condition.
Acknowledgments: We would like to thank all clinical experts and medical residents of Om-al-Banin Specialized Women's Hospital and the specialists and medical residents of the Obstetrics and Gynecology departments of Ghaem and Emam-Reza hospitals. We are also thankful to Dr. Tabesh for his contributions to data analysis.
Ethical Permissions: Ethics approval and consent to participate informed consent were not required to be obtained due to the nature of the study.
Conflicts of Interests: There are no conflicts of interest for any of the authors.
Authors’ Contribution: Samimi T. (First Author), Introduction Writer/Main Researcher (25%); MohammadEbrahimi Sh. (Second Author), Discussion Writer/Statistical Analyst (25%); Tara F. (Third Author), Assistant Researcher (10%); Mostafavi S.M. (Fourth Author) Assistant Researcher (10%); Ebrahimi Miandehi E. (Fifth Author), Assistant Researcher (10%); Tara M. (Sixth Author), Methodologist/Main Researcher (20%).
Funding/Support: This article was developed as part of a master thesis funded and supported by Mashhad University of Medical Sciences; Grant no. 921915.
This study was aimed to develop a structured model for clinical MR documentation and presentation in the Obstetrics and Gynecology department of three teaching hospitals to improve the overall informational and presentation quality of morning report sessions. The model was developed in two formats: Structured Paper-based Form (SPF) and Structured Electronic Format (SEF). The overall format was developed in two sections: General Information and Patient-specific Information, including 64 items in 11 categories. The prospective users of such a model are gynecological residents in charge of running MR sessions almost every morning.
One of the crucial problems in clinical education is the lack of standardized documentation and, consequently, weakness in evidence-based medicine [12]. We also face problems such as widespread data, high data volume, and poor documentation [13]. Our initial literature review, globally and nationally, showed no evidence of any proposed uniform structure for morning report documentation and presentation. However, there were similarities among the practicing countries (including Iran), such as the number of meetings over a specific period [4, 5, 14], the person in charge of case presentation [14-16], session facilitators [4, 14, 17], the person responsible for patient selection, and type of individuals regularly attending sessions [4, 5, 18].
One of the purposes of MR sessions is to discuss different aspects of patients' diagnosis and therapeutic options. Therefore, avoiding unnecessary information and having adequate and accurate information about patients is indisputable [5, 19]. According to the back-to-back chart regarding information adequacy of the structured form (Diagram 2), 70% of residents estimated the presence of adequate items as high and very high, while 90% estimated the presence of unnecessary items as low and very low. Confirming the results on both sides of the chart showed that the developed structured model reliably covers information items to patients' presentations in the MR sessions. The result of previous similar studies also confirms the results of our study [20-22].
In this study, twenty gynecological residents were provided 16 clinical MRs to compare three formats, including conventional forms, SPF, and SEF (n=48). The results showed that 75% of residents indicated that the SEF format has more readability and 60% considered it a format providing a clearer understanding of patient status. This result can be interpreted as the potential benefits of electronic records as compared to paper formats. In another study, two formats of structured and free-text reporting were compared, evaluating 330 reports by eleven experts from content and clarity. The results showed that an individual's satisfaction and preference for using structured reports were significantly different from unstructured reports [23].
More than half of our residents believed that using the SPF format will facilitate the reporting workflow. In a similar study, eleven experts from eight countries examined structured reports of radiology at the focus group meetings. Similar to our findings, this study concluded that workflow facilitation benefited from using structured reports [24]. Selectivity in creating data elements for recording and collecting data is considered a central part of Medicine Art [25]. Therefore, the selection and use of predefined datasets to generate reports can improve the workflow process of patient reports and data.
According to the results of Ganeshan's study, one of the benefits of structured reporting is its positive impact on research and the facilitation of data mining [26]. The results of another study have also shown that using the structured form is useful for future research [27]. It has also been shown that data mining and integration with decision support systems and clinical guidelines will improve [26]. In the current study, with a significant difference, 80% of residents considered the SPF format a more appropriate option for use in future research studies, which is in line with the results of the studies as mentioned above.
Archiving, maintaining, and retrieving reports documentation is a continuous communication process between clinical care team members that provides information on patients' health care status [28]. This is essential for various educational and assessment purposes during MR sessions but is nevertheless challenging MR sessions [5, 29]. Our study covered this challenge as our initial results showed no standard system to archive and retrieved MR documents (Table 3). In the current study, for 80% of residents, the SPF format was a better option for ease of archiving and information retrieval that could meet the information needs and improve documentation flow. Wrenn et al. used a structured form for patients referring to the emergency department over eight months, in which the results indicated a significant improvement in archiving and retrieval [27]. Since the use of electronic databases can undoubtedly lead to better archiving and retrieval of information sources [30], it seems that the reason for this paradoxical deviation in residents' attitudes towards the paper format is mostly due to its structured appearance rather than the comparable potential values of SEF format, which contains both structure and achievability.
As the results showed, the preferred format for use by half of the residents was SPF, and the other half preferred the conventional format (30%) and the SET format (20%), respectively. This comparison shows that practitioners prefer to use paper forms, whether in structured or free-text formats, compared to computer systems. Using computer systems to enter clinical information is more difficult and less flexible than paper forms [31], and also data entry into the structured electronic form is a more time-demanding process [32]. It is also worth noting that there is no teaching for ten-fingers typing in the Iranian education system, and most residents are no exception. This is a very important observation, which explains why much time is spent on typing, which results in an unwillingness to use electronic systems which require rapid typing. Therefore, it seems that it will speed up reporting and increase the workload and demand more time on the part of residents.
There were some limitations in our study. First, focusing on the opinions of local experts may reduce the generalizability of the developed model universally. However, we believe that the proposed methodology will still be useful in designing a similar local model in other countries. The study also had a limited view in its medical focus on gynecology and obstetrics; however, we find no reason why our core proposition of giving structures to MR documentation could not benefit other departments.
Future studies in this area could take more advanced steps into incorporating automatic production of structured MR from free-text reports using Natural Language Processing (NLP). For this purpose, the obtained structure in this study can be used as a strong basis, particularly in obstetrics and gynecology. We also recommend that future researchers apply our methods to develop similar standards for structuring MR documentation in other areas of clinical specialties.
Conclusion
Investigating the information adequacy of the reports and providing the necessary items for the presentation of cases in the MR sessions can enrich the clinical content and improve the educational and research quality of the reports. From the perspectives of the experts involved in the MR sessions of the gynecology department, the structured model was more valuable than the conventional format in terms of readability, improved documentation, easier archiving and retrieval, and a better understanding of the patient's condition.
Acknowledgments: We would like to thank all clinical experts and medical residents of Om-al-Banin Specialized Women's Hospital and the specialists and medical residents of the Obstetrics and Gynecology departments of Ghaem and Emam-Reza hospitals. We are also thankful to Dr. Tabesh for his contributions to data analysis.
Ethical Permissions: Ethics approval and consent to participate informed consent were not required to be obtained due to the nature of the study.
Conflicts of Interests: There are no conflicts of interest for any of the authors.
Authors’ Contribution: Samimi T. (First Author), Introduction Writer/Main Researcher (25%); MohammadEbrahimi Sh. (Second Author), Discussion Writer/Statistical Analyst (25%); Tara F. (Third Author), Assistant Researcher (10%); Mostafavi S.M. (Fourth Author) Assistant Researcher (10%); Ebrahimi Miandehi E. (Fifth Author), Assistant Researcher (10%); Tara M. (Sixth Author), Methodologist/Main Researcher (20%).
Funding/Support: This article was developed as part of a master thesis funded and supported by Mashhad University of Medical Sciences; Grant no. 921915.
Article Type: Qualitative Research |
Subject:
Technology of Health Education
Received: 2021/04/7 | Accepted: 2021/06/3 | Published: 2021/07/4
Received: 2021/04/7 | Accepted: 2021/06/3 | Published: 2021/07/4
References
1. Spencer J. Learning and teaching in the clinical environment. BMJ. 2003;326(7389):591-4. [Link] [DOI:10.1136/bmj.326.7389.591] [PMID] [PMCID]
2. Parrino TA, Villanueva AG. The principles and practice of morning report. JAMA. 1986;256(6):730-3.
https://doi.org/10.1001/jama.256.6.730 [Link] [DOI:10.1001/jama.1986.03380060056025]
3. Ranse K, Grealish L. Nursing students' perceptions of learning in the clinical setting of the dedicated education unit. J Adv Nurs. 2007;58(2):171-9. [Link] [DOI:10.1111/j.1365-2648.2007.04220.x] [PMID]
4. Amin Z, Guajardo J, Wisniewski W, Bordage G, Tekian A, Niederman LG. Morning report: Focus and methods over the past three decades. Acad Med. 2000;75(10 Suppl):1-5. [Link] [DOI:10.1097/00001888-200010001-00002] [PMID]
5. Mowla M. Morning report: A tool for improving medical education. J Bangladesh Coll Physicians Surg. 2012;30(2):91-5. [Link] [DOI:10.3329/jbcps.v30i2.11410]
6. Boushehri E, Khamseh ME, Farshchi A, Aghili R, Malek M, Valojerdi AE. Effects of morning report case presentation on length of stay and hospitalisation costs. Med Educ. 2013;47(7):711-6. [Link] [DOI:10.1111/medu.12152] [PMID]
7. Wildman-Tobriner B, Allen BC, Bashir MR, Camp M, Miller C, Fiorillo LE, et al. Structured reporting of CT enterography for inflammatory bowel disease: Effect on key feature reporting, accuracy across training levels, and subjective assessment of disease by referring physicians. Abdom Radiol. 2017;42(9):2243-50. [Link] [DOI:10.1007/s00261-017-1136-1] [PMID]
8. Hussein R, Engelmann U, Schroeter A, Meinzer HP. DICOM structured reporting: Part 2, problems and challenges in implementation for PACS workstations. Radiographics. 2004;24(3):897-909. [Link] [DOI:10.1148/rg.243035722] [PMID]
9. Kuhn K, Gaus W, Wechsler JG, Janowitz P, Tudyka J, Kratzer W, et al. Structured reporting of medical findings: Evaluation of a system in gastroenterology. Methods Inf Med. 1992;31(4):268-74. [Link] [DOI:10.1055/s-0038-1634885]
10. Atlas MC, Smigielski EM, Wulff JL, Coleman MT. Case studies from morning report. Med Ref Serv Q. 2003;22(3):1-14. [Link] [DOI:10.1300/J115v22n03_01] [PMID]
11. Ramratnam B, Kelly G, Mega A, Tilkemeier P, Schiffman FJ. Determinants of case selection at morning report. J Gen Intern Med. 1997;12(5):263-6. [Link] [DOI:10.1007/s11606-006-5061-1]
12. Yazdani S, Arab M, Hosseini F, Mansouri B, Yaghmaei M, Khoshgoftar Z, et al. Evaluation of the structure of morning report sessions of the wards of type one educational hospitals and comparison with announced standards of the ministry of health and medical education. Qom Univ Med Sci J. 2013;7(1):43-50. [Persian] [Link]
13. Ahmadian L, Cornet R, Kalkman C, De Keizer NF. Development of a national core dataset for preoperative assessment. Methods Inf Med. 2009;48(2):155-61. [Link] [DOI:10.3414/ME9218] [PMID]
14. Razavi SM, Shahbaz Ghazvini S, Dabiran S. Students' benefit rate from morning report sessions and its related factors in Tehran university of medical sciences. Iran J Med Educ. 2012;11(7):798-806. [Persian] [Link]
15. Banks DE, Shi R, Timm DF, Christopher KA, Duggar DC, Comegys M, et al. Decreased hospital length of stay associated with presentation of cases at morning report with librarian support. J Med Libr Assoc. 2007;95(4):381-7. [Link] [DOI:10.3163/1536-5050.95.4.381] [PMID] [PMCID]
16. Reilly B, Lemon M. Evidence-based morning report: A popular new format in a large teaching hospital. Am J Med. 1997;103(5):419-26. [Link] [DOI:10.1016/S0002-9343(97)00173-3]
17. Farhadifar F, Bahrami M, Yousefi F, Farazi E, Bahrami A. Comparative study of morning report in conventional & evidence based medicine forms, from the viewpoint of medical students. Res Med Educ. 2016;8(1):47-56. [Persian] [Link] [DOI:10.18869/acadpub.rme.8.1.47]
18. Rabiei M, Saeidi M, Kiani MA, Mohebi Amin S, Ahanchian H, Jafari SA, et al. Selecting the patients for morning report sessions: Case-based vs. conventional method. Electron Physician. 2015;7(4):1163-7. [Persian] [Link]
19. Hosseini A, Moghaddasi H, Jahanbakhsh M. Designing minimum data sets of diabetes mellitus: Basis of effectiveness indicators of diabetes management. Health Inf Manag. 2010;7(3):330-40. [Persian] [Link]
20. Kanegaye JT, Cheng JC, Ian McCaslin R, Trocinski D, Silva PD. Improved documentation of wound care with a structured encounter form in the pediatric emergency department. Ambul Pediatr. 2005;5(4):253-7. [Link] [DOI:10.1367/A04-196R.1] [PMID]
21. Johnson AJ, Chen MYM, Swan JS, Applegate KE, Littenberg B. Cohort study of structured reporting compared with conventional dictation. Radiology. 2009;253(1):74-80. [Link] [DOI:10.1148/radiol.2531090138] [PMID]
22. Marcovici PA, Taylor GA. Journal club: Structured radiology reports are more complete and more effective than unstructured reports. AJR Am J Roentgenol. 2014;203(6):1265-71. [Link] [DOI:10.2214/AJR.14.12636] [PMID]
23. Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011;260(1):174-81. [Link] [DOI:10.1148/radiol.11101913] [PMID] [PMCID]
24. Bosmans JML, Peremans L, Menni M, De Schepper AM, Duyck PO, Parizel PM. Structured reporting: If, why, when, how-and at what expense? results of a focus group meeting of radiology professionals from eight countries. Insights Imaging. 2012;3(3):295-302. [Link] [DOI:10.1007/s13244-012-0148-1] [PMID] [PMCID]
25. Shortliffe EH. Biomedical informatics: The science and the pragmatics. In: Shortliffe EH, Cimino JJ. Biomedical informatics. London: Springer; 2014. [Link] [DOI:10.1007/978-1-4471-4474-8]
26. Ganeshan D, Duong PAT, Probyn L, Lenchik L, McArthur TA, Retrouvey M, et al. Structured Reporting in Radiology. Acad Radiol. 2018;25(1):66-73. [Link] [DOI:10.1016/j.acra.2017.08.005] [PMID]
27. Wrenn K, Rodewald L, Lumb E, Slovis C. The use of structured, complaint-specific patient encounter forms in the emergency department. Ann Emerg Med. 1993;22(5):805-12. [Link] [DOI:10.1016/S0196-0644(05)80796-6]
28. Khorasani P, Rassouli M, Zagheri-Tafreshi M, Parvizy S, Nasr Esfahani M. Development and evaluation of patient education record for structured documentation of patient education process. J Health Promot Manag. 2014;3(4):1-16. [Persian] [Link]
29. Yazdani S, Arab M, Noghabaei G, Hosseini F. Quality dimensions of educational morning report sessions; short communication. J Med Edu. 2015;14(2):81-5. [Persian] [Link]
30. Kassab MKI, Abu-Naser SS, Al Shobaki MJ. An analytical study of the reality of electronic documents and electronic archiving in the management of electronic documents in the palestinian pension agency (PPA). Eur Acad Res. 2017;4(12):10052-102. [Link]
31. Poon AD, Fagan LM. PEN-Ivory: The design and evaluation of a pen-based computer system for structured data entry. Proc Annu Symp Comput Appl Med Care. 1994;447-51. [Link]
32. Bush RA, Kuelbs C, Ryu J, Jiang W, Chiang G. Structured data entry in the electronic medical record: perspectives of pediatric specialty physicians and surgeons. J Med Syst. 2017;41(5):75. [Link] [DOI:10.1007/s10916-017-0716-5] [PMID] [PMCID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |