Volume 11, Issue 1 (2023)
Health Educ Health Promot 2023, 11(1): 21-27 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Cheraghi P, Sadri M, Moradi L, Cheraghi Z. Assessment of Health-related Needs in Older Adults:
A Systematic Review. Health Educ Health Promot 2023; 11 (1) :21-27
URL: http://hehp.modares.ac.ir/article-5-64542-en.html
URL: http://hehp.modares.ac.ir/article-5-64542-en.html
1- School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
2- Department of Gerontology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
3- Department of Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
4- Modeling of Noncommunicable Diseases Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
2- Department of Gerontology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
3- Department of Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
4- Modeling of Noncommunicable Diseases Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
Full-Text [PDF 1563 kb]
(733 Downloads)
| Abstract (HTML) (756 Views)
Full-Text: (209 Views)
Introduction
Over the past years, more attention has been paid to the health-related needs of the elderly population as a vulnerable subgroup [1]. According to the World Health Organization report in 2021, the total number of older adults worldwide was around 1.4 billion. It is predicted that it will reach two billion people in 2050, and two-thirds of this population will belong to developing countries [2, 3].
The persistent increase in the elderly population is a major challenge for societies and health systems [4]. In addition to physical disorders, the elderly face psychological, social, environmental, and health-related problems and often have complex and unknown needs [5]. On the other hand, issues such as lack of security and social participation, unsuitable family environment, and mental problems have been expressed as significant and essential needs of this group [6].
Health Needs Assessment (HNA) should be comprehensive, multidimensional, and systematic to ensure that the real needs of the individual are well identified [4]. Meeting the particular needs of the elderly in society to promote active and prosperous aging in them finds new and broader dimensions [5].
Assessment of the real needs of the elderly and planning for their better and more practical provision can be considered as one of the actions of the health care centers that provide services to the elderly. Also, a comprehensive assessment of needs can help to focus the health service force on critical identified needs [7].
Finally, in this area, older adults' health needs assessment and intervention will increase their quality of life and satisfaction, prevent living in Long-Term Care (LTC) and extended hospital stays, and reduce the death rate among them [8].
If the assessment of the needs of the elderly is accompanied by effective long-term management, it can improve survival and performance. However, older adults' needs assessment has not received the attention of researchers in geriatrics, and the lack of assessment of the needs of the elderly in the health system seriously threatens the condition of the elderly [7, 9]. The experience of advanced societies has shown that the un-estimated needs of the elderly can impose a significant burden on the social, economic, and health systems [10]. Therefore, concurrently, as the elderly population increases in different societies, the needs and factors affecting their health promotion should be identified for adequate interventions [11]. In this regard, this study aimed to design and implement a health-related need assessment of the elderly under a systematic review.
Information and Methods
Eligibility criteria
In this systematic review, we included all studies to identify all types of health-related needs in older adults. The study population in this review was the world's older adults, regardless of gender, residence, and ethnicity. There were no restrictions on the study time, location, and language. A 27-item checklist of PRISMA was used for reporting the introduction, methods, results, and discussion of this study [12].
Search strategy
The following keywords were used to design the search strategy: (aged OR aging OR "older adults" OR "older people" OR "older person" OR elderly) AND (need OR "needs assessment" OR "health-related needs" OR" health need assessment").
International databases, including the Web of Sciences (ISI), Medline, Scopus, and ProQuest, were searched up to June 2022. To find additional studies, we scanned the reference lists of all retrieved studies. Two investigators (Z.Ch and L.M) were independently and simultaneously responsible for screening the titles and abstracts of the retrieved studies. In case of any disagreement, it was resolved upon discussion and judgment of a third investigator (P. Ch). Also, the kappa index was calculated to evaluate the investigators' agreement rate. The inter-authors' reliability based on kappa statistics was 88%. Afterward, the full texts of the selected studies were reviewed to assess the eligibility criteria. Finally, the studies that met the inclusion criteria were selected for analysis.
Data extraction
Two authors (Z.Ch and L.M) extracted the data from the included studies. The following data were extracted using a pre-designed datasheet from the studies that met the inclusion criteria: the first author's name, year of publication, study location, the mean age of the participant, gender, sample size, and the aim of the study. We contacted the authors in case of missing data in the included studies.
Risk of bias assessment
The quality of the included studies was assessed using the Critical Appraisal Skills Programme (CASP) [13]. The following items were used for quality assessment:
1. Address a focused question
2. Appropriateness of method for answering the research question
3. Description of methods of selection
4. Un-biases of sampling
5. Representative of sampling
6. Sample size based on pre-study considerations of statistical power
6. Satisfactory response rate
7. Measurements likely to be valid and reliable.
8. The statistical significance assessed, and confidence intervals given for the main results
9. Confounding factors that are not taken into account.
10. The score range of the questionnaire was 0-24. 0-12 was rated as poor, 13-18 as moderate, and above 19 as good quality.
Findings
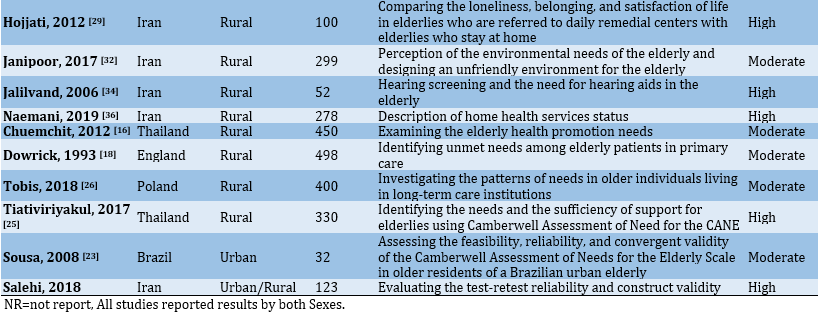
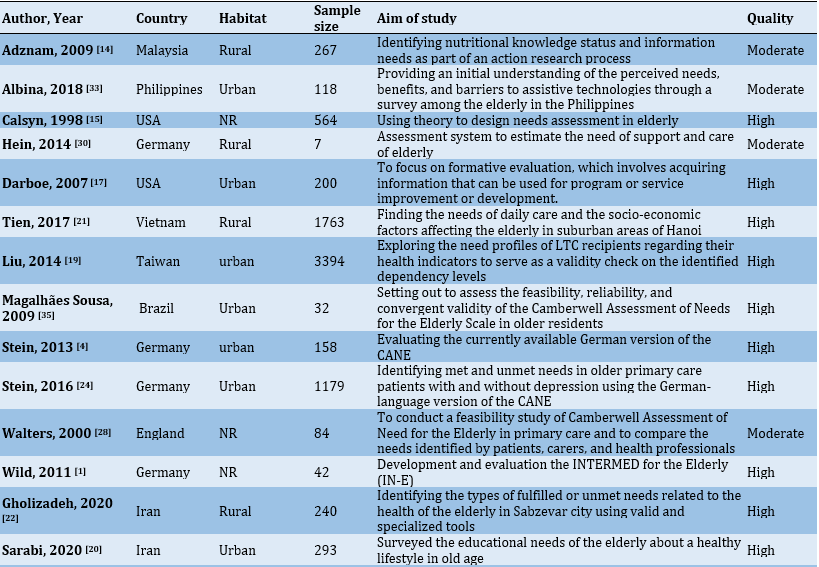
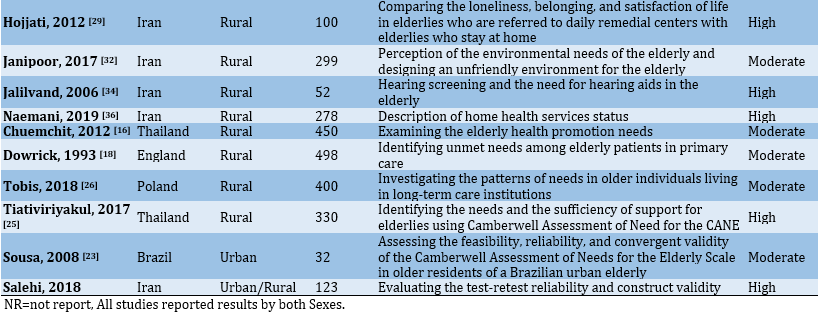
This review retrieved 469 studies through international databases, and 82 were excluded because of duplication. In the next stage, 43 articles were excluded upon checking the titles and abstracts, and another 20 were excluded upon checking the full texts as they did not meet the eligibility criteria. Finally, 24 studies remained in the final analysis (Figure 1).
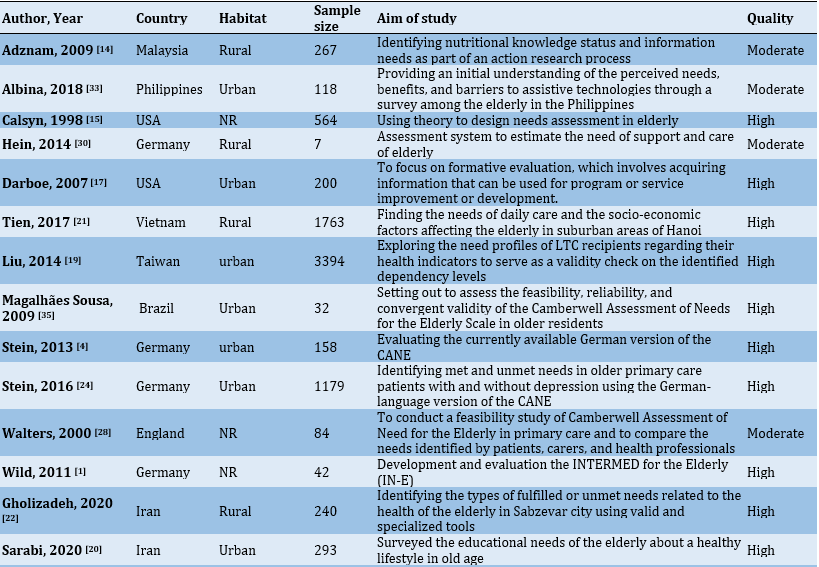
The total sample size was 10780 subjects. The mean age of the participants was 73.7±8.2 years (Table 1).
Six main areas of health-related needs were identified during this study as follows: 1) physical needs, 2) psychological needs, 3) social needs, 4) environmental needs, 5) health literacy needs, and 6) intelligent assistive technology.
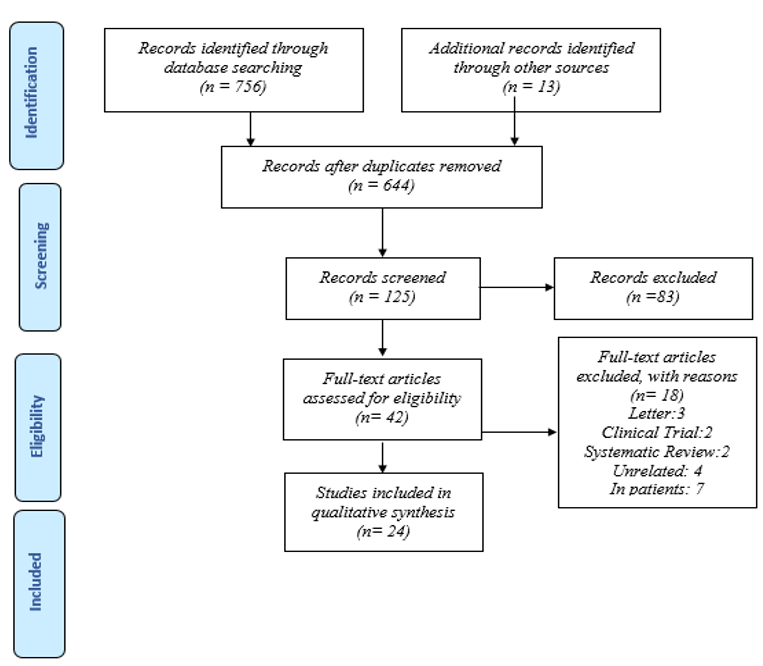
Figure 1) Steps of searching databases and registers
Physical needs: This domain included the various scales as follows: physical health, eyesight/hearing/communication, mobility/falls, medication, self-care, continence, functional needs (ADL/IADL), skilled nurse visit, adult day care, palliative care, drugs, treatment, home, and community-based rehabilitation home nursing care and prosthetics. Several studies mentioned these things as the physical needs of older adults [14-21].
Psychological needs: This domain included the various scales: psychological distress, memory, behavior, alcohol, psychotic symptoms, deliberate self-harm, inadvertent self-harm, coordination of care, mental health threat, depression, belonging, life satisfaction, and support for the bereaved. Eight studies reported the mentioned scales [4, 22-28].
Social needs: This domain included the various scales: company, intimate relationships, daytime activities, information abuse/neglect, health insurance, communication, Home and Community-Based Care Services, Social vulnerability, social support, home-monitoring system, environmental safety, aged-friendly city, and transportation. Eleven studies were reported on the mentioned scales [4, 21-30].
Over the past years, more attention has been paid to the health-related needs of the elderly population as a vulnerable subgroup [1]. According to the World Health Organization report in 2021, the total number of older adults worldwide was around 1.4 billion. It is predicted that it will reach two billion people in 2050, and two-thirds of this population will belong to developing countries [2, 3].
The persistent increase in the elderly population is a major challenge for societies and health systems [4]. In addition to physical disorders, the elderly face psychological, social, environmental, and health-related problems and often have complex and unknown needs [5]. On the other hand, issues such as lack of security and social participation, unsuitable family environment, and mental problems have been expressed as significant and essential needs of this group [6].
Health Needs Assessment (HNA) should be comprehensive, multidimensional, and systematic to ensure that the real needs of the individual are well identified [4]. Meeting the particular needs of the elderly in society to promote active and prosperous aging in them finds new and broader dimensions [5].
Assessment of the real needs of the elderly and planning for their better and more practical provision can be considered as one of the actions of the health care centers that provide services to the elderly. Also, a comprehensive assessment of needs can help to focus the health service force on critical identified needs [7].
Finally, in this area, older adults' health needs assessment and intervention will increase their quality of life and satisfaction, prevent living in Long-Term Care (LTC) and extended hospital stays, and reduce the death rate among them [8].
If the assessment of the needs of the elderly is accompanied by effective long-term management, it can improve survival and performance. However, older adults' needs assessment has not received the attention of researchers in geriatrics, and the lack of assessment of the needs of the elderly in the health system seriously threatens the condition of the elderly [7, 9]. The experience of advanced societies has shown that the un-estimated needs of the elderly can impose a significant burden on the social, economic, and health systems [10]. Therefore, concurrently, as the elderly population increases in different societies, the needs and factors affecting their health promotion should be identified for adequate interventions [11]. In this regard, this study aimed to design and implement a health-related need assessment of the elderly under a systematic review.
Information and Methods
Eligibility criteria
In this systematic review, we included all studies to identify all types of health-related needs in older adults. The study population in this review was the world's older adults, regardless of gender, residence, and ethnicity. There were no restrictions on the study time, location, and language. A 27-item checklist of PRISMA was used for reporting the introduction, methods, results, and discussion of this study [12].
Search strategy
The following keywords were used to design the search strategy: (aged OR aging OR "older adults" OR "older people" OR "older person" OR elderly) AND (need OR "needs assessment" OR "health-related needs" OR" health need assessment").
International databases, including the Web of Sciences (ISI), Medline, Scopus, and ProQuest, were searched up to June 2022. To find additional studies, we scanned the reference lists of all retrieved studies. Two investigators (Z.Ch and L.M) were independently and simultaneously responsible for screening the titles and abstracts of the retrieved studies. In case of any disagreement, it was resolved upon discussion and judgment of a third investigator (P. Ch). Also, the kappa index was calculated to evaluate the investigators' agreement rate. The inter-authors' reliability based on kappa statistics was 88%. Afterward, the full texts of the selected studies were reviewed to assess the eligibility criteria. Finally, the studies that met the inclusion criteria were selected for analysis.
Data extraction
Two authors (Z.Ch and L.M) extracted the data from the included studies. The following data were extracted using a pre-designed datasheet from the studies that met the inclusion criteria: the first author's name, year of publication, study location, the mean age of the participant, gender, sample size, and the aim of the study. We contacted the authors in case of missing data in the included studies.
Risk of bias assessment
The quality of the included studies was assessed using the Critical Appraisal Skills Programme (CASP) [13]. The following items were used for quality assessment:
1. Address a focused question
2. Appropriateness of method for answering the research question
3. Description of methods of selection
4. Un-biases of sampling
5. Representative of sampling
6. Sample size based on pre-study considerations of statistical power
6. Satisfactory response rate
7. Measurements likely to be valid and reliable.
8. The statistical significance assessed, and confidence intervals given for the main results
9. Confounding factors that are not taken into account.
10. The score range of the questionnaire was 0-24. 0-12 was rated as poor, 13-18 as moderate, and above 19 as good quality.
Findings
This review retrieved 469 studies through international databases, and 82 were excluded because of duplication. In the next stage, 43 articles were excluded upon checking the titles and abstracts, and another 20 were excluded upon checking the full texts as they did not meet the eligibility criteria. Finally, 24 studies remained in the final analysis (Figure 1).
The total sample size was 10780 subjects. The mean age of the participants was 73.7±8.2 years (Table 1).
Six main areas of health-related needs were identified during this study as follows: 1) physical needs, 2) psychological needs, 3) social needs, 4) environmental needs, 5) health literacy needs, and 6) intelligent assistive technology.
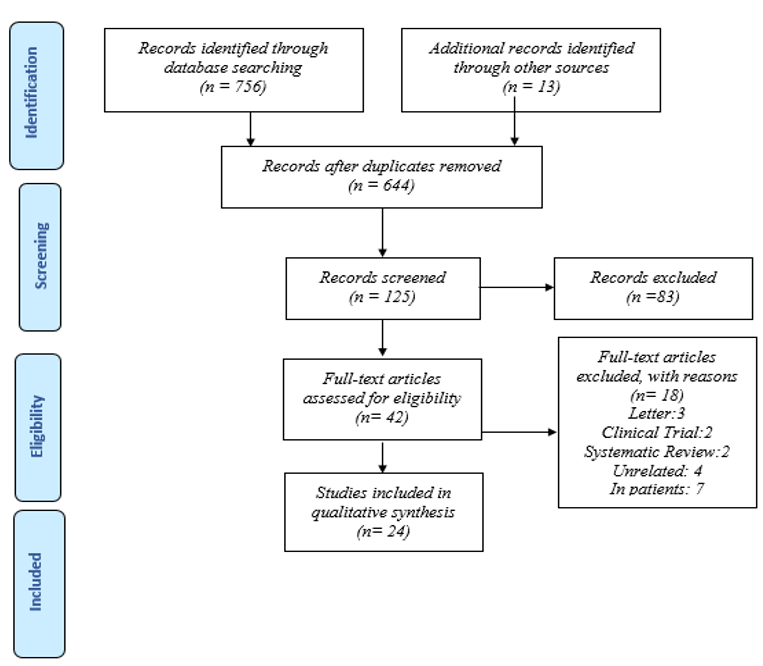
Figure 1) Steps of searching databases and registers
Physical needs: This domain included the various scales as follows: physical health, eyesight/hearing/communication, mobility/falls, medication, self-care, continence, functional needs (ADL/IADL), skilled nurse visit, adult day care, palliative care, drugs, treatment, home, and community-based rehabilitation home nursing care and prosthetics. Several studies mentioned these things as the physical needs of older adults [14-21].
Psychological needs: This domain included the various scales: psychological distress, memory, behavior, alcohol, psychotic symptoms, deliberate self-harm, inadvertent self-harm, coordination of care, mental health threat, depression, belonging, life satisfaction, and support for the bereaved. Eight studies reported the mentioned scales [4, 22-28].
Social needs: This domain included the various scales: company, intimate relationships, daytime activities, information abuse/neglect, health insurance, communication, Home and Community-Based Care Services, Social vulnerability, social support, home-monitoring system, environmental safety, aged-friendly city, and transportation. Eleven studies were reported on the mentioned scales [4, 21-30].
Table 1) Characteristics of included studies
Environmental (basic) needs: This domain included various scales such as accommodation, looking after a home, money, benefits, caring for someone else, food, proper home meal, and home deals delivery. Ten studies reported the mentioned scales [4, 22-28, 31, 32].
Health education and health literacy needs: This domain included the various scales: valuable health information resources, caregiver's need for information, healthy lifestyle, health education, and health promotion needs. Two studies reported the mentioned scales [1, 33].
Intelligent assistive technology: This domain included the various scales: intelligent assistive technology, assistive devices or environmental improvement, and smart devices. Three studies reported the mentioned scales [1, 33, 34].
Discussion
The purpose of this study was to assess the health needs of older adults, which was done after a review of the needs related to the health of older adults, including six areas: physical, psychological, social, environmental, health literacy, and technology.
Health-related needs, including medication and care by others, have been introduced as met needs. Moreover, 60% of the unmet needs of older adults are related to adaptation to the living environment, 58% are related to hearing and vision problems, 48% are related to daily activities, and 42% are related to illness. 34% of physical problems are related to close encounters, and 32% are related to self-care. Also, issues such as the lack of social security and participation in social activities, the inappropriateness of the family environment, and incontinence and psychological problems have been mentioned as significant needs of older adults in society [6].
Based on the results of Cheraghi et al.'s study among the unmet needs of older adults, the highest need was related to physical (eyesight/hearing impairment, mobility/fall, and incontinence) and social (company, intimate relationships, and daytime activities) needs, and the lowest unmet needs were related to the psychological dimension [37].
The existence of a family and social support network that protects older adults is like a shield from the stresses of old age. Also, in the social dimension, family support, especially children's support for older adults' parents, is one of the elements of successful older adults in eastern societies [38, 39]. Fry states that a comfortable and good old age in eastern countries is defined by the family and social relations between them, which increases resilience among older adults. On the contrary, successful aging in western societies becomes meaningful with activity and social participation [40].
In the reviewed studies, the psychological needs of older adults are also mentioned as a general need. One of the dimensions of successful aging is psychological well-being, which Havighurst considers synonymous with life satisfaction [41]. Nagalingam also points out that life satisfaction is one of the aspects of successful aging in eastern societies [39]. There was also a correlation between psychological symptoms and needs. Symptoms that need treatment increase the need, and if these needs remain unmet, they can increase the symptoms of mental disorders [37].
This study showed that health education and health literacy are the basic needs of older adults. Using health education programs to raise awareness of health promotion behaviors is beneficial to the health of the older adult community. Even though educating health promotion behaviors was initially emphasized on adults of younger age. Several studies have highlighted the effectiveness of health education programs in maintaining functional independence, preventing the effects of age-related chronic diseases, and increasing self-care in the elderly. Hence paying attention to older adults' self-care and responsibility for various diseases is a support solution requiring a high level of health literacy [42-45]. The World Health Organization introduced health literacy as one of the most significant determinants of health. It advised the world's countries to monitor and coordinate strategic activities to improve health literacy in their society [46]. Many studies have pointed out the effect of health literacy on increasing the quality of life in old age and the positive effect of education on adopting a healthy lifestyle in older adults [47-49].
Finally, the last category of the needs of the older adults in this study was the technological needs, which include assistive rehabilitation technologies and smart tools in the care of older adults. Assistive rehabilitation technologies are considered adequate for older adults to be healthy, independent, safe, and socially active. These technologies, with their role in improving the quality of life and well-being of older adults, are attracting increasing attention as a potential solution [50-53].
The limitations of the study were as follows: In the reviewed studies, the needs of the older adults were not examined from the perspective of the official and informal caregivers of the older adults. Only the needs assessment was done by the older adults, likely to underestimate or exceed the reality of the needs. Therefore, a close estimate will be obtained when the opinions of both groups (older adults and formal and informal caregivers) are reported and compared.
Another limitation of the current study was the lack of needs assessment studies of older adults in communities with different socioeconomic statuses. In comparison, socioeconomic status is directly related to the older adults' estimated needs.
Since old age is divided into different age subgroups and the needs of each age group are different from other groups, it is suggested to consider this point in future studies. Also, it seems necessary to pay attention to the diverse needs of older adults in different settings and communities. It should also be done better to identify the priority and unmet needs of older adults and use their results in interventions and decisions for the health promotion of older adults.
Conclusion
Achieving the goal of successful aging is possible with health needs assessment in all dimensions, including physical health, social well-being, psychological well-being, financial security, and an older adults-friendly environment. Accordingly, to identify new needs and accurately estimate the met and unmet needs of older adults and perform timely interventions, a periodical needs assessment is necessary so that information is available to policymakers.
Acknowledgments: We would like to thank from Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences for financial support.
Ethical Permission: This study was approved by the Research Committee of the Hamadan University of Medical Sciences (UMSHA), Hamadan, Iran (Code: 1400131717, IR. UMSHA. REC.1399.960).
Conflict of interest: The authors declare no conflict of interest.
Authors Contribution: Cheraghi P (First Author), Methodologist/Main Researcher/Discussion Writer (25%); Sadri M (Second Author), Introduction Writer/Main Researcher/Discussion Writer (25%); Moradi L (Third Author), Introduction Writer/Discussion Writer (25%); Cheraghi Z (Fourth Author), Methodologist/Discussion Writer (25%)
Funding: This study was funded by the Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences.
Environmental (basic) needs: This domain included various scales such as accommodation, looking after a home, money, benefits, caring for someone else, food, proper home meal, and home deals delivery. Ten studies reported the mentioned scales [4, 22-28, 31, 32].
Health education and health literacy needs: This domain included the various scales: valuable health information resources, caregiver's need for information, healthy lifestyle, health education, and health promotion needs. Two studies reported the mentioned scales [1, 33].
Intelligent assistive technology: This domain included the various scales: intelligent assistive technology, assistive devices or environmental improvement, and smart devices. Three studies reported the mentioned scales [1, 33, 34].
Discussion
The purpose of this study was to assess the health needs of older adults, which was done after a review of the needs related to the health of older adults, including six areas: physical, psychological, social, environmental, health literacy, and technology.
Health-related needs, including medication and care by others, have been introduced as met needs. Moreover, 60% of the unmet needs of older adults are related to adaptation to the living environment, 58% are related to hearing and vision problems, 48% are related to daily activities, and 42% are related to illness. 34% of physical problems are related to close encounters, and 32% are related to self-care. Also, issues such as the lack of social security and participation in social activities, the inappropriateness of the family environment, and incontinence and psychological problems have been mentioned as significant needs of older adults in society [6].
Based on the results of Cheraghi et al.'s study among the unmet needs of older adults, the highest need was related to physical (eyesight/hearing impairment, mobility/fall, and incontinence) and social (company, intimate relationships, and daytime activities) needs, and the lowest unmet needs were related to the psychological dimension [37].
The existence of a family and social support network that protects older adults is like a shield from the stresses of old age. Also, in the social dimension, family support, especially children's support for older adults' parents, is one of the elements of successful older adults in eastern societies [38, 39]. Fry states that a comfortable and good old age in eastern countries is defined by the family and social relations between them, which increases resilience among older adults. On the contrary, successful aging in western societies becomes meaningful with activity and social participation [40].
In the reviewed studies, the psychological needs of older adults are also mentioned as a general need. One of the dimensions of successful aging is psychological well-being, which Havighurst considers synonymous with life satisfaction [41]. Nagalingam also points out that life satisfaction is one of the aspects of successful aging in eastern societies [39]. There was also a correlation between psychological symptoms and needs. Symptoms that need treatment increase the need, and if these needs remain unmet, they can increase the symptoms of mental disorders [37].
This study showed that health education and health literacy are the basic needs of older adults. Using health education programs to raise awareness of health promotion behaviors is beneficial to the health of the older adult community. Even though educating health promotion behaviors was initially emphasized on adults of younger age. Several studies have highlighted the effectiveness of health education programs in maintaining functional independence, preventing the effects of age-related chronic diseases, and increasing self-care in the elderly. Hence paying attention to older adults' self-care and responsibility for various diseases is a support solution requiring a high level of health literacy [42-45]. The World Health Organization introduced health literacy as one of the most significant determinants of health. It advised the world's countries to monitor and coordinate strategic activities to improve health literacy in their society [46]. Many studies have pointed out the effect of health literacy on increasing the quality of life in old age and the positive effect of education on adopting a healthy lifestyle in older adults [47-49].
Finally, the last category of the needs of the older adults in this study was the technological needs, which include assistive rehabilitation technologies and smart tools in the care of older adults. Assistive rehabilitation technologies are considered adequate for older adults to be healthy, independent, safe, and socially active. These technologies, with their role in improving the quality of life and well-being of older adults, are attracting increasing attention as a potential solution [50-53].
The limitations of the study were as follows: In the reviewed studies, the needs of the older adults were not examined from the perspective of the official and informal caregivers of the older adults. Only the needs assessment was done by the older adults, likely to underestimate or exceed the reality of the needs. Therefore, a close estimate will be obtained when the opinions of both groups (older adults and formal and informal caregivers) are reported and compared.
Another limitation of the current study was the lack of needs assessment studies of older adults in communities with different socioeconomic statuses. In comparison, socioeconomic status is directly related to the older adults' estimated needs.
Since old age is divided into different age subgroups and the needs of each age group are different from other groups, it is suggested to consider this point in future studies. Also, it seems necessary to pay attention to the diverse needs of older adults in different settings and communities. It should also be done better to identify the priority and unmet needs of older adults and use their results in interventions and decisions for the health promotion of older adults.
Conclusion
Achieving the goal of successful aging is possible with health needs assessment in all dimensions, including physical health, social well-being, psychological well-being, financial security, and an older adults-friendly environment. Accordingly, to identify new needs and accurately estimate the met and unmet needs of older adults and perform timely interventions, a periodical needs assessment is necessary so that information is available to policymakers.
Acknowledgments: We would like to thank from Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences for financial support.
Ethical Permission: This study was approved by the Research Committee of the Hamadan University of Medical Sciences (UMSHA), Hamadan, Iran (Code: 1400131717, IR. UMSHA. REC.1399.960).
Conflict of interest: The authors declare no conflict of interest.
Authors Contribution: Cheraghi P (First Author), Methodologist/Main Researcher/Discussion Writer (25%); Sadri M (Second Author), Introduction Writer/Main Researcher/Discussion Writer (25%); Moradi L (Third Author), Introduction Writer/Discussion Writer (25%); Cheraghi Z (Fourth Author), Methodologist/Discussion Writer (25%)
Funding: This study was funded by the Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences.
Article Type: Systematic Review |
Subject:
Health Promotion Setting
Received: 2022/10/1 | Accepted: 2022/12/19 | Published: 2023/02/5
Received: 2022/10/1 | Accepted: 2022/12/19 | Published: 2023/02/5
References
1. Wild B, Lechner S, Herzog W, Maatouk I, Wesche D, Raum E, et al. Reliable integrative assessment of health care needs in elderly persons: the INTERMED for the Elderly (IM-E). J Psychosom Res. 2011;70(2):169-78. [Link] [DOI:10.1016/j.jpsychores.2010.09.003]
2. Shaw MP, Peart DJ, Fairhead OJW. Perceived stress in university students studying in a further education college. Res Post Compuls Educ. 2017;22(3):442-52. [Link] [DOI:10.1080/13596748.2017.1362534]
3. World Health Organization. International day of older persons [Internet]. Geneva: World Health Organization;2018 [cited 2021 Dec 23]. Available from: http://www.who.int/life-course/news/events/intl-day-of-older-persons-2018/en/. [Link]
4. Stein J, Luppa M, König H-H, Riedel-Heller SG. Assessing met and unmet needs in the oldest-old and psychometric properties of the German version of the Camberwell assessment of need for the elderly (CANE)-a pilot study. Int Psychogeriatr. 2014;26(2):285-95. [Link] [DOI:10.1017/S1041610213001993]
5. Rasel M, Ardalan A. The future of ageing and its health care costs: A warning for health system. Iran J Ageing. 2007;2(2):300-5. [Persian] [Link]
6. Ashokkumar T, Chacko T, Munuswamy S. Health care and social needs of the elderly: Assessed by the tool Camberwell Assessment of need for the elderly. Int J Trop Med. 2011;6(5):97-9. [Link]
7. Reynolds T, Thornicroft G, Abas M, Woods B, Hoe J, Leese M, et al. Camberwell Assessment of Need for the Elderly (CANE): Development, validity and reliability. Br J Psychiatry. 2000;176(5):444-52. [Link] [DOI:10.1192/bjp.176.5.444]
8. Miranda-Castillo C, Woods B, Galboda K, Oomman S, Olojugba C, Orrell M. Unmet needs, quality of life and support networks of people with dementia living at home. Health Qual Life Outcomes. 2010;8(1):132. [Link] [DOI:10.1186/1477-7525-8-132]
9. Smith F, Orrell M. Does the patient-centred approach help identify the needs of older people attending primary care? Age Ageing. 2007;36(6):628-31. [Link] [DOI:10.1093/ageing/afm131]
10. Yamada T, Chen C-C, Murata C, Hirai H, Ojima T, Kondo K, et al. Access disparity and health inequality of the elderly: unmet needs and delayed healthcare. Int J Environ Res Public Health. 2015;12(2):1745-72. [Link] [DOI:10.3390/ijerph120201745]
11. Fernandes L, Gonçalves-Pereira M, Leuschner A, Martins S, Sobral M, Azevedo LF, et al. Validation study of the Camberwell Assessment of Need for the Elderly (CANE) in Portugal. Int Psychogeriatr. 2009;21(1):94-102. [Link] [DOI:10.1017/S1041610208008041]
12. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. [Link] [DOI:10.1016/j.ijsu.2021.105906]
13. Firooznia R, Dargahi H, Khaledian Z, Jafari -Koshki T. Strengths and weaknesses of maternal health program evaluation tools in Iranian primary health care system. Payesh. 2018;17(5):521-30. [Persian] [Link]
14. Adznam S, Shahar S, Rahman SA, Yusof NAM, Arshad F, Yassin Z, et al. An action research on promotion of healthy ageing and risk reduction of chronic disease: A need assessment study among rural elderly Malays, care givers and health professionals. J Nutr Health Aging. 2009;13(10):925-30. [Link] [DOI:10.1007/s12603-009-0253-0]
15. Calsyn RJ, Roades LA, Calsyn DS. Acquiescence in needs assessment studies of the elderly. Gerontologist. 1992;32(2):246-52. [Link] [DOI:10.1093/geront/32.2.246]
16. Chuemchit M, Deeleartyuenyong N, Promluan P, Khiewkhum J, Taneepanichskul S. Health promotion behavior and needs assessment: What do Thai elderly want and need. Int J Soc Sci Hum. 2012;2(5):396-9. [Link] [DOI:10.7763/IJSSH.2012.V2.133]
17. Darboe K, Ahmed LS. Elderly African immigrants in Minnesota: A case study of needs assessment in eight cities. Educ Gerontol. 2007;33(10):855-66. [Link] [DOI:10.1080/03601270701569101]
18. Dowrick C. Self‐assessment by elderly people‐a means of identifying unmet need in primary care. Health Soc Care Commun. 1993;1(5):289-96. [Link] [DOI:10.1111/j.1365-2524.1993.tb00230.x]
19. Liu LF, Yao HP. Examining the need assessment process by identifying the need profiles of elderly care recipients in the Ten-Year Long-Term Care Project (TLTCP) of Taiwan. J Am Med Dir Assoc. 2014;15(12):946-54. [Link] [DOI:10.1016/j.jamda.2014.07.007]
20. Sarabi RE. Assessment of educational needs of elderly people in Sirjan about healthy lifestyle, 2018-2019. J Gerontol. 2020;5(1):68-78. [Persian] [Link]
21. Tien DN, Zhang GL. Quality of life among the elderly in suburban Hanoi, Vietnam: Needs assessment and socio-economic factors affecting the elderly care. In: Jiang W, Ga X, editors. Proceedings of the 2017 International Conference on Innovations in Economic Management and Social Science. AEBMR-Advances in Economics Business and Management Research. 2017. p. 745-51. [Link] [DOI:10.2991/iemss-17.2017.146]
22. Gholizadeh S, Estaji Z, Akrami R, Ghanbari Moghaddam A. Health related needs of the elderly in Sabzevar city of Iran , 2019. J Gerontol. 2020;4(4):68-75. [Persian] [Link] [DOI:10.29252/joge.4.3.68]
23. Sousa R, Scazufca M, Rossi Menezes P, Luiz Crepaldi A, James Prince M. Feasibility and reliability of the elderly version of the Camberwell Assessment of Needs (CANE): results from the São Paulo Ageing & Health Study. Bras J Psychiatry. 2009;31(1):34-8. [Link] [DOI:10.1590/S1516-44462009000100009]
24. Stein J, Pabst A, Weyerer S, Werle J, Maier w, Heilmann K, et al. The assessment of met and unmet care needs in the oldest old with and without depression using the Camberwell Assessment of Need for the Elderly (CANE): Results of the Age MooDe study. J Affect Disord. 2016;193:309-17. [Link] [DOI:10.1016/j.jad.2015.12.044]
25. Tiativiriyaku P, Xenos P. Assessment of need for elderly in community in Hang Dong district, Chang Mai province, Thailand using camberwell assessment of need for the elderly questionnaire (CANE). J Health Res. 2017;31(2):43-54. [Link]
26. Tobis S, Wieczorowska-Tobis K, Talarska D, Pawlaczyk M, Suwalska A. Needs of older adults living in long-term care institutions: an observational study using Camberwell assessment of need for the elderly. Clin Interv Aging. 2018;13:2389-95. [Link] [DOI:10.2147/CIA.S145937]
27. Wieczorowska-Tobis K, Talarska D, Kropinska S, Jaracz K, Tobis S, Suwalska A, et al. The Camberwell Assessment of Need for the Elderly questionnaire as a tool for the assessment of needs in elderly individuals living in long-term care institutions. Arch Gerontol Geriatr. 2016;62:163-8. [Link] [DOI:10.1016/j.archger.2015.10.005]
28. Walters K, Liffe S, See Tai S, Orrell M. Assessing needs from patient, career and professional perspective: Camberwell assessment of needs for the elderly in primary care. Age Ageing. 2000;29(6):505-10. [Link] [DOI:10.1093/ageing/29.6.505]
29. Hojjati H, Hojjati H, Sharfnia SH, Salmasi E, Hosseinzadeh E, Farhadi S. Comparison of loneliness, belonging and life satisfaction in the elderlies living at home with the nursing home residents. J Health Care. 2012;14(3):9-15. [Persian] [Link]
30. Hein A, Steen EE, Thiel A, Hulsken-Giesler M, Wist T, Helmer A, et al. Working with a domestic assessment system to estimate the need of support and care of elderly and disabled persons: results from field studies. Inform Health Soc Care. 2014;39(3-4):210-31. [Link] [DOI:10.3109/17538157.2014.931857]
31. van der Ploeg ES, Bax D, Boorsma M, Nijpels G, van Hout HPJ. A cross-sectional study to compare care needs of individuals with and without dementia in residential homes in the Netherlands. BMC Geriatr. 2013;13:51. [Link] [DOI:10.1186/1471-2318-13-51]
32. Janipour B, Arasteh S, Taheri MR, Hossein SF. Environmental needs assessment of the elderly in Karaj urban parks. J Architect Environ Res. 2019;1(2):49-60. [Persian] [Link] [DOI:10.1016/j.vlsi.2017.09.010]
33. Albina EM, Hernandez AA. Assessment of the elderly on perceived needs, benefits and barriers: Inputs for the design of intelligent assistive technology. 2018 16th International Conference on ICT and Knowledge Engineering. Bangkok, Thailand: 2018. p. 82-91. [Link] [DOI:10.1109/ICTKE.2018.8612447]
34. Javadian SR. Gerontological social work. Q J Soc Work. 2015;4(2):27-32. [Persian] [Link]
35. Maghsoudi A. The study of prevalence of chronic diseases and its association with quality of life in the elderly of Ewaz (South of Fars province), 2014. Navid No. 2016;18(61):35-42. [Persian] [Link]
36. Naemani F, Fayaz-Bakhsh A, Sohrabi Z, Zali ME. Service required for elderly receiving home care: a situational analysis. Payesh. 2019;18(6):513-25. [Persian] [Link]
37. Cheraghi P, Delbari A, Cheraghi Z, Karimi-Shahanjarini A, Zanjari A. Assessment of met and unmet care needs in older adults without mental disorders using the Camberwell assessment of need for the elderly: A systematic review and meta-analysis. J Res Health Sci. 2021;21(4):e00530. [Link] [DOI:10.34172/jrhs.2021.64]
38. Leesri T, Srisuphan W, Senaratana W, Vannarit T. CIPP model evaluation of a collaborative diabetic management in community setting. Glob J Medical Clin Case Rep. 2016;3(1):29-34. [Link] [DOI:10.17352/2455-5282.000030]
39. Nagalingam J. Understanding successful aging: a study of older Indian adults in Singapore. Care Manag J. 2007;8(1):18-25. [Link] [DOI:10.1891/152109807780494131]
40. Fry CL, Dickerson-Putman J, Draper P, Ikels C, Keith J, Glascock AP, et al. Culture and the meaning of a good old age. Cultur Aging Context. 1997;3:99-123. [Link]
41. Craciun C. Successful aging-utopia or the result of lifelong learning? Meaning and representations of ageing in romanian elderly. Ageing Int. 2012;37(4):373-85. [Link] [DOI:10.1007/s12126-011-9131-2]
42. Chang K-S, Tsai W-H, Tsai C-H, Yeh H-I, Chiu P-H, Chang Y-W, et al. Effects of health education programs for the elders in community care centers-Evaluated by health promotion behaviors. Int J Gerontol. 2017;11(2):109-13. [Link] [DOI:10.1016/j.ijge.2017.03.009]
43. de Vries NM, van Ravensberg CD, Hobbelen JSM, Rikkert MGMO, Staal JB, Nijhuis-van der Sanden MWG. Effects of physical exercise therapy on mobility, physical functioning, physical activity and quality of life in community-dwelling older adults with impaired mobility, physical disability and/or multi-morbidity: a meta-analysis. Ageing Res Rev. 2012;11(1):136-49. [Link] [DOI:10.1016/j.arr.2011.11.002]
44. Toto PE, Raina KD, Holm MB, Schlenk EA, Rubinstein EN, Rogers JC. Outcomes of a multicomponent physical activity program for sedentary, community-dwelling older adults. J Aging Phys Act. 2012;20(3):363-78. [Link] [DOI:10.1123/japa.20.3.363]
45. Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. 2010;15(S2):9-19. [Link] [DOI:10.1080/10810730.2010.499985]
46. Ferguson B. Health literacy and health disparities: The role they play in maternal and child health. Nurs Womens Health. 2008;12(4):286-98. [Link] [DOI:10.1111/j.1751-486X.2008.00343.x]
47. Salimi F, Garmaroudi G, Hosseini SM, Batebi AJJoe, health c. Effect of self-care educational program to improving quality of life among elderly referred to health centers in Zanjan. J Educ Community Health. 2015;2(2):28-37. [Persian] [Link]
48. Zanjari N, Bahrami G, Koochi MN, Arani ZA. Factors affecting the elderly's quality of life in the middle east: A systematic review. J Educ Community Health. 2021;8(2):143-58. [Persian] [Link] [DOI:10.52547/jech.8.2.143]
49. Alipour N, Dastoorpour M, Araban M. Effect of educational intervention on fear of falling in the elderly people: A randomized cluster trial. J Educ Community Health. 2020;7(3):145-51. [Persian] [Link] [DOI:10.29252/jech.7.3.145]
50. Coughlin JF. Understanding the Janus face of technology and ageing: Implications for older consumers, business innovation and society. Int J Emerg Technol Soc. 2010;8(2):62-7. [Link]
51. Demiris G, Rantz MJ, Aud MA, Marek KD, Tyrer HW, Skubic M, et al. Older adults' attitudes towards and perceptions of 'smart home'technologies: a pilot study. Med Inform Internet Med. 2004;29(2):87-94. [Link] [DOI:10.1080/14639230410001684387]
52. Magnusson L, Hanson E, Borg MJT, Disability. A literature review study of information and communication technology as a support for frail older people living at home and their family carers. Technol Disabil. 2004;16(4):223-35. [Link] [DOI:10.3233/TAD-2004-16404]
53. Yoshany N, Khameshi SSS, Rezaei M, Baghin N, Kakolaki ZK. Relationship between quality of life and using smart phones in the elderly. J Educ Community Health. 2019;6(4):247-55. [Persian] [Link] [DOI:10.29252/jech.6.4.247]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |