Volume 10, Issue 4 (2022)
Health Educ Health Promot 2022, 10(4): 779-789 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Dahmardeh H, Sadooghiasl A, Mohammadi E, Kazemnejad A. Design and Evaluation of Self-Compassion Scale in Iranian Patients with Multiple Sclerosis. Health Educ Health Promot 2022; 10 (4) :779-789
URL: http://hehp.modares.ac.ir/article-5-64172-en.html
URL: http://hehp.modares.ac.ir/article-5-64172-en.html
1- Department of Nursing, Faculty of Medical Sciences, Zahedan University of Medical Sciences, Zahedan, Iran
2- Department of Nursing, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
3- Department of Biostatistics, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
2- Department of Nursing, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
3- Department of Biostatistics, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
Keywords: elf-Compassion [MeSH], Multiple Sclerosis [MeSH], Psychometrics [MeSH], Instrumentation [MeSH], Factor Analysis [MeSH]
Full-Text [PDF 1969 kb]
(316 Downloads)
| Abstract (HTML) (501 Views)
Full-Text: (81 Views)
Introduction
Multiple Sclerosis (MS) is a chronic, inflammatory, progressive and common autoimmune disease of the nervous system [1-3]. Most people suffer from it at a young age, around their 20s to 40s. With many debilitating symptoms and complications [2], it is the most common cause of neurological disability in adults [4].
The MS Atlas, compiled by the Multiple Sclerosis International Federation (MSIF), is an open-source global compendium of data regarding the epidemiology of MS and the availability of resources for people with MS reported at country, regional and global levels. The first edition was produced in 2008 in collaboration with the World Health Organization (WHO) and was updated in 2013 [5]. Based on that, a total of 2.8 million people are estimated to live with MS worldwide (35.9 per 100,000 population). MS prevalence has increased in every world region since 2013, but gaps in prevalence estimates persist. The pooled incidence rate across 75 reporting countries is 2.1 per 100,000 persons/year, and the mean age of diagnosis is 32 years. Females are twice as likely to live with MS as males [6].
People with MS learn most of their family and social responsibilities during their 20s to 40s; however, for MS patients, the disease does not allow them to become contributing individuals in their societies, as they may encounter difficulties in carrying out their tasks [1]. Patients’ early symptoms and complications, such as visual impairments, pain, urinary incontinence, and weakness can threaten their independence and ability to effectively participate in society and their families, which in turn affects all aspects of their everyday lives [2].
Considering the features of this disease, and as the number of individuals suffering from MS is increasing [2], concerns have been raised regarding the quality of life and healthcare expenses of these patients. The impact and effectiveness of self-care have been observed before in patients’ medical and personal outcomes [7]. Self-care can reduce patients’ expenses, improve their quality of life, and it should be noted that its significance has been evident in patients’ medical and person-centered results [8].
The concept of self-compassion has a key role in self-care [9], and it can especially be observed in patient’s self-caring behavior in chronic diseases [10]. The significance of self-compassion is elaborated further by Mills et al., who found that self-compassion and self-care behaviors are directly correlated [11]. Additionally, Nery-Hurwit et al. strongly emphasized that MS patients require measures like self-compassion to perform better self-care [12]. The direct correlation between these two concepts requires further attention [11]. As it has been confirmed in other studies that have investigated other patients, self-compassion increases MS patients’ ability and mental attitude, which also ensures better outcomes [12].
Self-compassion is an adaptive way to communicate with oneself when aware of inadequacies and cope with difficult living conditions such as life-threatening condition and chronic illnesses [13]. Self-compassion as a psychological construct has a significant effect on the care and treatment of chronic patients [14-16]. The ability of self-compassion when feeling inadequacy, such as physical disability, enhances a person's ability to accept their situation better. Therefore, if self-compassion is reinforced in MS patients who are living with a chronic illness, they might change their mental attitude towards the situation [12].
A prerequisite for any action to promote self-compassion is to measure it using specific tools appropriate to the target group [14-16]. For the first time in the United States, Neff explained the concept of self-compassion, and based on designed and validated the only tool available for measuring it. The questions in this scale measure six components, including self-kindness, feeling isolated, self-judgment, mindfulness, common humanity, and over-identification [17]. This tool is not specific to a specific group and is used in all communities and groups.
After Neff, qualitative studies were conducted to examine the meaning of self-compassion in different communities and groups [18, 19]. The results of these studies showed that although Neff has defined six components, self-compassion has other components as well. For example, the results of a study by Freeman added the component of seeking support to the dimensions introduced by Neff [20]. These results indicate that the concept of self-compassion can have different definitions in varied situations and populations and therefore have different components than what Neff introduced. In addition, various investigations have been conducted to assess the psychometry of Neff tool in different groups and countries [21-27]. The results of these studies showed that the six dimensions introduced in the Neff tool are not repeated in these studies, i.e., people had different perceptions of self-compassion according to factors such as life experiences, cultural conditions, and values [28]. Hence, it can be said that these factors affect the self-compassion of individuals in different societies.
Experts believe that the content of a tool should be extracted directly from people who would use it. However, it should be coordinated to the culture of communities and countries in which the tool is to be used [29]. Therefore, planning to promote self-compassion in MS patients requires measuring it using appropriate and accurate tools. Consequently, the present study aimed to design and evaluate self-compassion assessment tools in MS patients to obtain more accurate information about their culture and values for planning to maintain and improve their mental and psychological status.
Instrument and Methods
This instrumentation study was conducted as a sequential-exploratory combined design. In the first stage, qualitative data were collected and analyzed, and in the quantitative stage, the scale was designed and its psychometric properties were tested. The present study consisted of three phases, including construct definition, item generation, and testing psychometric characteristics of the instrument performed from December 2019 to July 2020.
Sample and setting
The samples should be representative of the target community [30]. Therefore, for sampling, patients from different ethnic groups in Iran were selected from the MS associations of Zahedan, Ahvaz, Kerman, East Azerbaijan, Ardabil, Yazd, Fasa, Astara, Amol, Sabzevar and North Khorasan.
Participants were purposefully selected from among MS patients who had been diagnosed for at least six months and had received treatment for at least six months. The setting of the study was hospitals and communities of Zahedan and Tehran Province, Iran.
The first phase: Construct definition
In the first phase, a qualitative study was performed using a guided content analysis according to self-compassion theory of Neff. Individual semi-structural interviews were performed to collect data. The duration of the interview was 15 to 55 minutes, with an average of 28 minutes. The place and time of the interview were determined according to participants’ preference. At the beginning of the interview, the purpose of the study was explained for the participants, and after receiving demographic information, they answered the main questions of the interview. The questions were redesigned based on the components of Neff's self-compassion theory. According to the participants' answers, exploratory questions were used to extract more data from their experiences. All interviews were recorded and transcribed. Then it was analyzed using the Directed Content Analysis method. This method was proposed in 2005 by Hsieh and Shannon [31].
The second phase: Item generation
In this phase, a theoretical and operational definition was determined for each of the main classes formed in the qualitative stage. The extraction of items depended on the definition of each of the dimensions and structures of the concept under study. The questionnaire questions were designed to include the dimensions of self-compassion mentioned by the participants in their interviews. At the end of this stage, an initial draft of the scale was prepared.
The third phase: Testing psychometric characteristics of the instrument
At this stage, the face and content validity of the structure and the reliability of the instrument were evaluated. To determine the face validity, two qualitative and quantitative methods were used. To determine the qualitative face validity, 10 potential users of the questionnaire (MS patients) were interviewed face to face regarding the difficulty level (recognizing items, phrases or words that are difficult for them to understand), the degree of appropriateness (appropriateness and proper relationship of the phrases with the dimensions of the questionnaire) and ambiguity (the possibility of misunderstandings or the existence of inadequacies in the meanings of the words). Then their opinions were reviewed and applied.
To evaluate the quantitative face validity, the impact score method was used. In this way, 10 patients were asked to rate the importance of each item on a 5-point Likert scale (quite important = 5, somewhat important = 4, moderately important = 3, slightly important = 2, it does not matter at all = 1). These patients were suffering from MS and were selected purposefully. The completed questionnaires at this stage were assessed with the formula as follows:
Impact score = frequency (%) × importance
A score of 1.5 and above indicated the appropriateness of the item.
To evaluate the validity of qualitative content, the opinion of experts (n=14) who had rich knowledge and experience in instrumentation, ethics, self-compassion, psychology, psychiatric nursing, and MS was obtained. The items were evaluated in terms of the level of difficulty, ambiguity, Persian grammar, use of appropriate words, and placement of words in their proper place.
To evaluate the validity of quantitative content, two methods of content validity ratio (CVR) and content validity index (CVI) were used. In the CVR index, the necessity of an item was evaluated from the perspective of experts (n=14). To calculate the CVR, each expert was asked to review each item based on a three-part spectrum: 1) necessary, 2) useful but not necessary, and 3) not necessary, then the answers were used to calculate the CVR. In this study, the minimum value of CVR index was considered as 0.51, regarding that each item was reviewed by 14 panel members [32].
For the content validity index, the relevance of items to the construct was measured from the perspective of experts. In this method, at the item level, Waltz and Basel's (1983) proposed formula was used to calculate the CVI: thus, the number of specialists who gave each question a score of 3 and 4 was divided by the total number of rankers (I-CVI). Besides, it was considered at the instrument level (S-CVI) [32].
After calculating the CVI based on the aggregation of the number of agreeing on points for each item (ranking 3 and 4 in the 4-point scale), relevance of an item was checked based on a score greater than 0.79 at the item level, and a score greater than 0.90 at the tool level [33].
In this way, from the 78 primary extracted items, after calculating the item impact score index with values higher than 1.5, content validity ratio higher than 0.51, and content validity index higher than 0.79, 73 items were selected and entered the factor analysis stage.
To evaluate the construct validity, Confirmatory Factor Analysis (CFA) and Exploratory Factor Analysis (EFA) methods were used. Since this study was designed based on Neff theory [34], CFA method was used first for items related to the constructs of Neff theory and Freeman's study because CFA is a confirmatory and theory-based method [35]. Then, for four structures added in this study to the classes introduced by Neff, EFA exploratory factor analysis was used [33, 36].
In the confirmatory factor analysis stage, the questionnaire was completed by 341 patients with MS (approximately 5 times the number of items) by purposive sampling. In investigations based on factor analysis, samples must represent the target population to achieve valid factors [30]. Therefore, for sampling, patients were selected from all over the country from MS associations in different cities.
Goodness of fit indices were used to assess the fit of confirmatory factor analysis, and items with a factor load above 0.3 were retained and approved [37].
Exploratory factor analysis was then performed for four new components, including concealment, spiritual resilience, concern for cohabitation, and being a role model for others. The Kaiser-Meyer-Olkin index test was used to determine the appropriateness of the sample size. Bartlett’s test of Sphericity was also used to evaluate the appropriateness of exploratory factor analysis. To determine the number of factors, the Eigenvalues (the sum of squared component loadings for each component) greater than one, the diagram of Scree Kettel (elbow point) and the percentage of variance greater than 5% were considered.
To determine the reliability of the questionnaire, two methods were used. First, the reliability of stability was performed using the test-retest method, which was measured 14 days later. Second, the information obtained from completing the self-compassion questionnaire by 51 patients with MS was used. Internal consistency was evaluated by Cronbach's alpha coefficient method performed by information extracted from 113 patients with MS after completion of the self-compassion questionnaire, and values equal to or greater than 0.7 were accepted. Statistical analysis was performed using SPSS 21 software.
Findings
Construct definition phase
In the qualitative phase, 11 categories were considered, including self-kindness, self-judgment, common humanity, isolation, mindfulness and over-identification (6 dimensions of Neff study), seeking support (Freeman), concealment, spiritual resilience, concern for living together, and role-playing for others. In the present study, in addition to replicating the 6 dimensions of the Neff study [34] and the Freeman “seeking support” dimension [20], 4 new dimensions were added to self-compassion.
Self-compassion in the MS patient means that when patients face such unpleasant conditions, they express “self-kindness” for self-compassion, in addition, “adhere to their treatment” and feel confident and valued, instead of “blaming themselves for the disease”. They consider the disease as a "human experience" that can happen to anyone, rather than finding themselves alone in the situation. They also respond in a "balanced way" to the discomfort they experience, rather than "magnifying" it in their minds and thinking of paralysis and disabilities. On the other hand, with the help and establishment of a "communication with a transcendental force", they create the capacity for relaxation and “seek support" from the family and their treatment team. Sometimes, due to the circumstances of the disease, they "hide" from others in order to avoid experiencing pity. They are also "concerned about their cohabitation." They inspire and guide their peers by trying to "be an example" for their peers. They experience a sense of self-compassion by connecting with others and making time for them.
A comparison of the above definition with the Neff's definition of self-compassion shows that the themes of "spiritual resilience", "worrying about the future of cohabitation", "hiding", and "being a role model for others" are new features added to Neff's definition of self-compassion.
Item generation phase
In this phase, items were extracted for each of the classes obtained from the qualitative stage. The items were examined by the members of the research team to ensure the accuracy and to find any overlapping and duplicate items. Duplicate items were removed, and some items were merged. Finally, the initial draft of the questionnaire was designed with 78 items.
Quantitative phase
Validity
To determine the qualitative face validity, 10 participants examined the tool. For example: "Item No. 44 - When the sensory symptoms of the disease occur, I try to alleviate it with a method such as using cold water to cool myself", which was difficult for most participants to understand, but remained without change to retain quantitative face validity and obtained an impact factor of 1.86, which was acceptable and was retained for the content validity stage, but was eventually removed from the questionnaire due to not obtaining a sufficient score in the next stages.
In the evaluation of quantitative face validity, 4 items obtained an impact factor score of less than 1.5 and were considered unacceptable. However, these items were retained for content validity review, and in the end, two of the 4 items remained due to good content validity.
In the quantitative content validity stage, 7 items of self-kindness (2 items), self-judgment (1 item), common humanity (1 item), mindfulness (2 items), and self-modeling (1 item) were removed due to not receiving sufficient CVR and CVI scores, leaving 71 items. On the other hand, 2 new items were added to the category of" being a role model for others" according to the results of qualitative validity content based on the research team's opinion. At the end of this stage, 73 items remained in the content validity stage due to obtaining sufficient CVR and CVI scores as well as an acceptable impact score in the face validity stage and were finalized.
The S-CVI score at the instrument level considered to be more than 0.90, which in this study, after removing the items that did not obtain a sufficient CVR and CVI scores, the S-CV was calculated as 0.93.
Construct validity
In total, 341 participants filled in the questionnaires in the quantitative phase. There were 266 females (78%) and 75 males (22%), 237 married (69.5%), and 104 single (30.5%). The mean age of participants was 34.69 years. The mean duration of the disease was 76.1 months (Table 1).
Table1) Frequency distribution of characteristics of the study participants (n=341)

The results of confirmatory factor analysis for structures based on Neff's theory and Freeman's study (self-kindness, self-judgment, common humanity, isolation, mindfulness, over-identification, and search for support) are shown in Table 2. The four indices were fit in the acceptable intervals; hence the model was confirmed according to the confirmatory factor analysis.
Table 2) Confirmatory factor analysis results
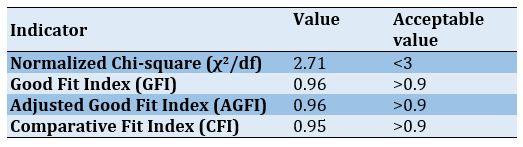
To examine the confirmatory factor analysis, the factors were defined by the symbol F (abbreviation for Factor) as follows: Factors F1 to F7, respectively, indicate self-kindness, self-judgment, common humanity, isolation, mindfulness, over-identification and seeking support (Figures 1-7).
Exploratory factor analysis
At the beginning of factor analysis, to determine the possibility of factorization, the appropriate adequacy measurement index test in the samples, Kaiser-Meyer-Olkin (KMO), and Bartlett's test of sphericity were used (Table 3).

Figure 1) Factor loads of self-kindness
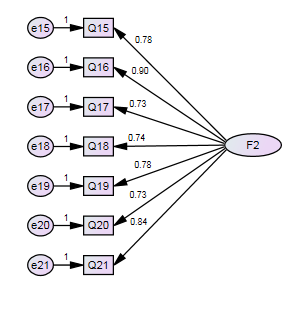
Figure 2) Factor loads of self-judgement
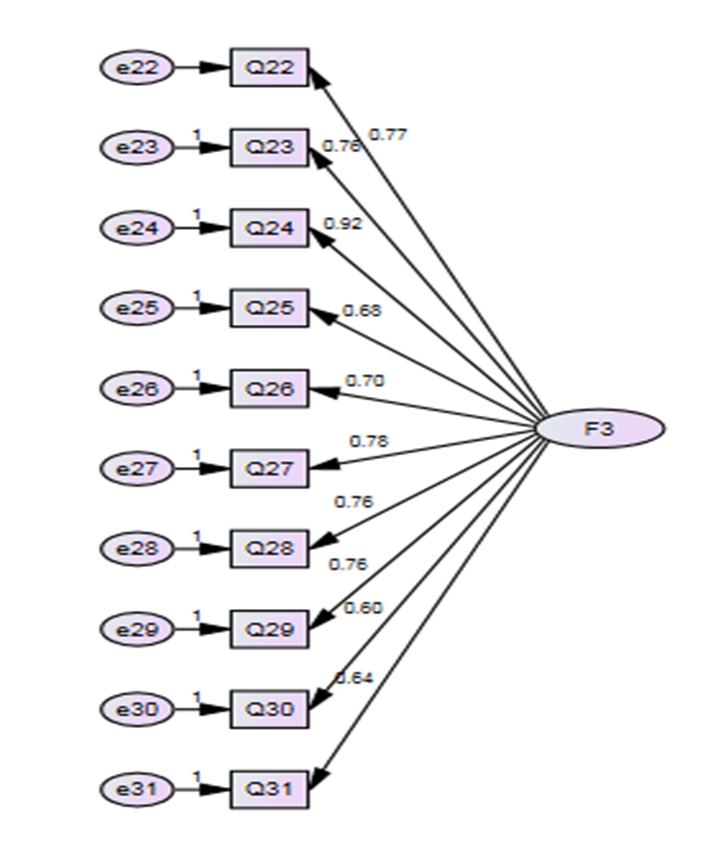
Figure 3) Factor loads of common humanity
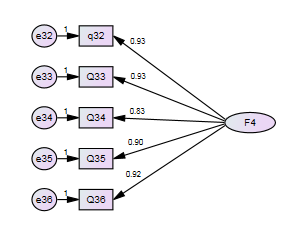
Figure 4) Factor loads of isolation
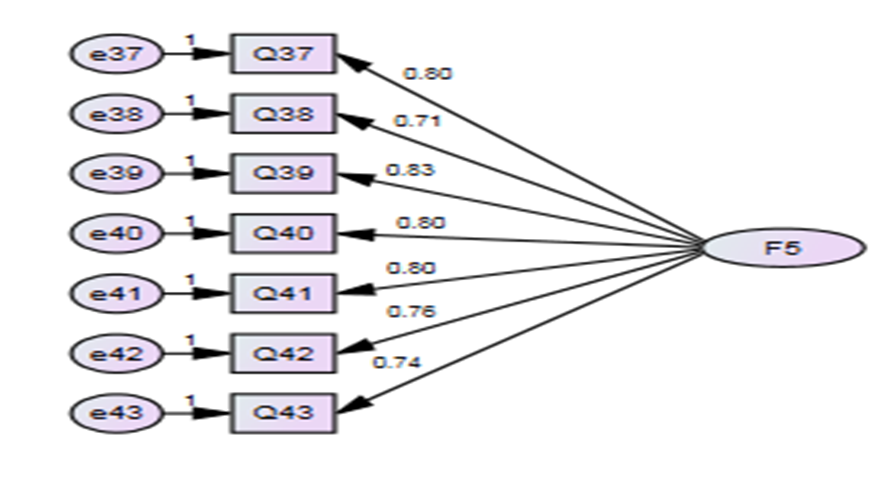
Figure 5) Factor loads of self-identification
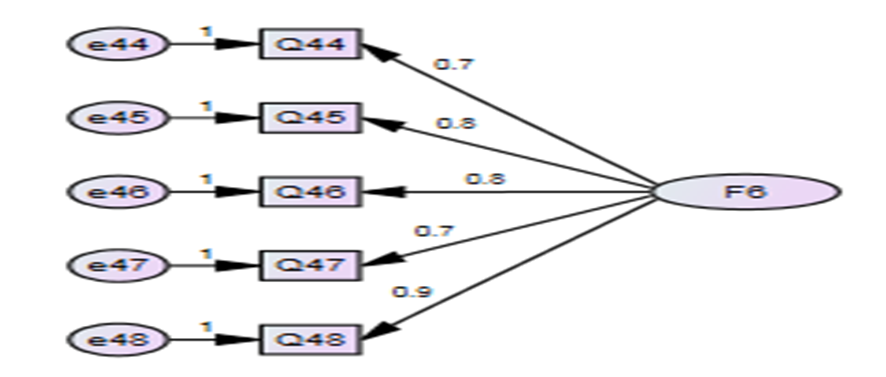
Figure 6) Factor loads of over-identification
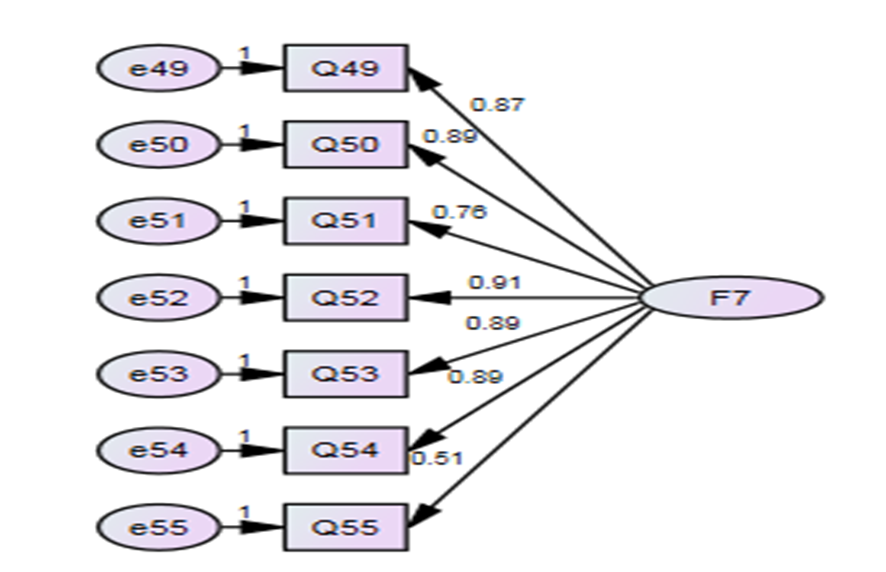
Figure 7) Factor loads of seeking support
Table 3 shows the Kaiser Meyer-Olkin sampling index equal to 0.803, based on which a good sampling of variables has been done based on the pairwise correlation of the reagents and their partial correlation. Also, the null hypothesis of the sphericity test in data was rejected (p<0.000), and the KMO test was confirmed. Therefore, it can be concluded that the implementation of exploratory factor analysis provided a suitable model for the present data and factor detection was possible, and the items were sufficient enough to predict the factors.
Table 3) Results of KMO and Bartlett tests

The results of explained variance values for the extraction of 4 new factors showed that with a specific eigenvalue above 2.441, they were able to predict 63.254 of total changes in self-compassion in patients with MS, which is a desirable value [38]. In this study, a factor load of 0.4 was determined as the minimum degree of acceptable correlation between each item and the extracted factors.
Eighteen items with a factor load of more than 0.4 in 4 factors included spiritual resilience (6 items), being a role model for others (3 items), worrying about cohabitation (5 items), and concealment (4 items). Three items from the category of “concerned with cohabitation” were transferred to the class of spiritual resilience because they were conceptually and semantically more similar. At this point, all questions were saved, and no item was deleted. At the end of this stage, a questionnaire with 73 items was prepared to check reliability.
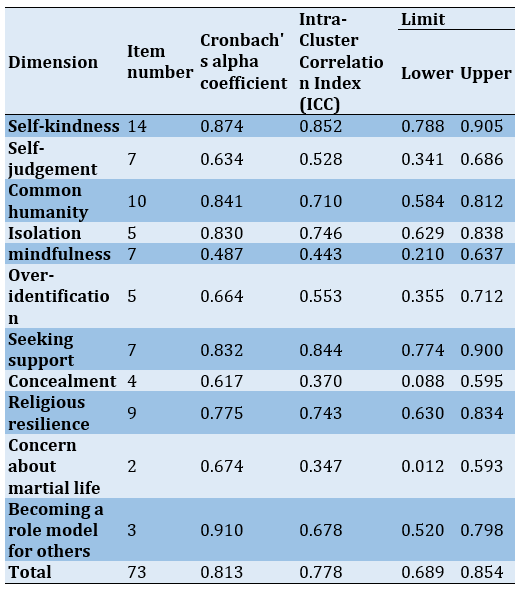
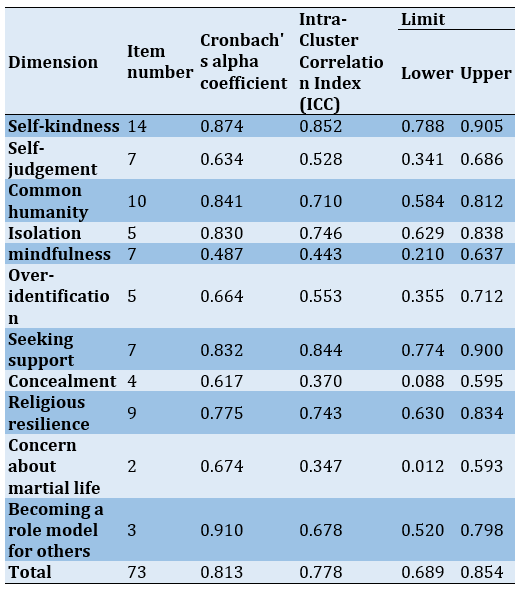
Reliability
To determine the internal consistency of the questionnaire, Cronbach's alpha coefficient was calculated to be 0.813, which showed that the questionnaire had an acceptable internal consistency. Also, to determine the stability of the questionnaire, retest test and calculation of intra-cluster correlation were used. The questionnaire was completed by 51 people in two stages, and the results were equal to 0.778 with a confidence interval of 0.854-0.689 and showed a good stability (Table 4).
Scoring
For the final questionnaire, a 5-point Likert scale was considered. In scoring the items, all had a positive meaning as the score of 5 indicates always, 4 more often, 3 occasionally, 2 rarely, and 1 never. Based on the above scoring and the number of items in the questionnaire, the minimum total score of the questionnaire was 73, and the maximum was 365.
Table 4) The results of determining the reliability of the self-compassion measurement tool in patients with MS
Discussion
The aim of this study was to design a self-compassion assessment tool in patients with MS disease. The tool items were based on 6 constructs of self-kindness, self-judgment, common humanity, isolation, mindfulness and over-identification of Neff theory and Freeman support search construct and 4 newly developed constructs of spiritual resilience, concealment, concern for cohabitation and role modeling designed based on the results of a qualitative study in MS patients with special life conditions. Psychometric findings indicated the validity and reliability of the designed questionnaire.
The first dimension of the present study tool was "self-kindness", which had 14 items. In the Neff study, which examined healthy individuals, the development of kindness and self-awareness were replaced instead of misjudgment in times of distress [34]. However, in the present study, new features of diet and medication adherence, feeling self-confidence and self-worth, and more attention to self were added to the construct. Sirois and Hirsch showed that self-compassion had been effective in adhering to treatment in patients with fibromyalgia, chronic fatigue syndrome, and cancer patients, which were probably due to the effect of self-compassion on reducing stress [39]. In the present study, MS patients, like those with cancer or chronic fatigue syndrome, perceived and experienced adherence to treatment and care along with a sense of self-confidence and self-worth as three other indicators of self-compassion.
The next dimension was "self-judgment", including 7 items, which was defined in Neff study as self-judging and blame in failure or pain and unhappiness [34]. While in the present study, new features of feeling insignificant to others and mental conflict about why they suffer from the disease were also added to the construct. The reason these features were added to the self-judgment structure is related to MS itself, which changes the body and affects how people treat them or vice versa. The results of a study by Jones et al. showed that patients with MS feel rejected and worthless because of the disease, and this leads to their isolation and reduced social relationships [40].
Many questions, negative ideas, and thoughts about the cause of the disease arise in the minds of patients with MS. Güner et al. stated that these negative automatic thoughts and dysfunctional attitudes are risk factors for developing depression and anxiety in individuals who have recently been diagnosed with the disease [41]. However, people with higher self-compassion have a lower risk of depression and anxiety than those without it [42]. Therefore, in this tool, these items were highlighted and considered.
Another dimension of the present study tool was common humanity, including 10 items. The items related to the positive mood reinforcement class in this dimension were somewhat consistent with the items of Neff tool. But in the present study, a new feature of “trying to play their role as before the disease” was added to this structure.
The next dimension was isolation, including 5 items. The items related to having negative self-image and isolation were consistent with the items of Neff tool; however, a tendency for isolation and social distancing was another new item different from Neff theory. The experience of loneliness is characteristic of MS [43]. These people often withdraw from participating in social activities [44]. In line with the results of the present study, Beal and Stuifbergen showed that women with MS may be exposed to loneliness due to social network changes that occur during chronic illness [45], so it is important to pay attention to loneliness and evaluate it in self-compassion.
Another dimension of the present study was mindfulness, including 7 items. Items related to categories of “trying to forget and not thinking about the illness and its negative aspects”, “accepting and coping with illness”, and “not blaming oneself for the illness” were consistent with the statements of the Neff tool. However, the present study added “adapting and accepting difficult treatment regimen with self-improvement”, “turning bad feelings into good ones about the disease”, and “changing attitudes to the illness” to the characteristics of Neff's mindfulness item. Patients with MS try to adapt to new changes and limitations in their life due to unpleasant and unpredictable symptoms, difficult treatment regimens, and uncertainty about the future of the disease [46]. In the present study, adaptation and acceptance of difficult treatment was achieved with self-improvement and self-compassion, so five items were designed to measure these items in patients with MS.
The sixth dimension of the present study tool was over-identification, including 5 items. In this respect, the items were conceptually consistent with the items of Neff theory. However, according to the findings of this study, there were more characteristics, including perception and worry about the progression of the disease by seeing patients with advanced condition, fear of paralysis and severe disability and thinking about it, and unwillingness to accept the disease and disabilities. Patients with chronic diseases are always afraid of the progression of the disease with all its consequences [47]. In the present study, due to the chronic nature of the disease, patients with MS were always afraid of the progression of the disease and their condition worsening and eventually paralysis, and thought about it a lot. Therefore, to measure these cases, 3 items were designed to fit the target group.
As mentioned, Neff self-compassion tool had 6 dimensions, and new dimensions were added by the present study for patients with MS. The first new dimension was "spiritual resilience", including 9 dimensions. For many patients with chronic illness, spirituality/religiosity is an important source of coping [48]. In the Iranian and Islamic society of the present study, many behaviors in individual and social life are influenced by religious beliefs [49], and many people tolerate stressful conditions better by praying, reading spiritual books or attending religious ceremonies [50]. Patients with MS tried to be patient and tolerated it by relying on God and having religious beliefs, thus showing self-compassion. In line with the present results, the results of a qualitative study by Ebrahimi et al. described one of the characteristics perceived by MS patients following the illness as "the use of spirituality" [51].
Searching for support was another new dimension with 7 items. MS patients perceived and expressed it as having a positive view of the attention and support of others and encouragement to their possessions and support of the family and their physician. In line with the results of the present study, Ghafari et al. expressed "support seeking" as one of the characteristics perceived by MS patients in the process of adapting to this disease [46].
Another new dimension was concealment with 4 items. MS patients expressed it as hiding the disease from others to avoid their pity and the following discomfort, thinking of themselves, and not expecting from others. In the present study, this dimension was compared with the dimension of seeking support, and some patients preferred to hide their illness instead of seeking support for a self-compassion to avoid pitiful treatment of others. The results of Earnshaw et al. study showed that MS patients, like other chronic patients, tolerate stigma [52]. Stigma is a threat that is related to cultural characteristics. In European cultures, they strongly emphasize individualistic norms and independent self-concept, while Asian cultures emphasize on collective norms and mutual self-concept. Likewise, In Iran, due to a culture of collectivism, patients are concerned about the way others look at them [53]. Thus, they try to hide their illness from others to avoid increased support from sympathetic people and prefer isolation [54].
Another new dimension found in this study was "concern about cohabitation" with two items shown by factor analysis. The onset of symptoms in MS is usually around the third or fourth decade of life, which is the age of childbearing, family growth, and the establishment and strengthening of social and marital relationships. In these patients, the challenge of coping with the disease, relationship problems, and sexual dysfunction are among the factors that threaten the emotional relationship between couples. As a result of the disease, the needs of spouses are often ignored and might harm the marital relationship leading to a possible loss of a sexual partner [55].
Another important issue is that in each country, the formation of a family has its own definition according to the accepted customs and laws. In the Iranian legal system, which is derived from the Islamic intellectual system, marriage is necessary to form a family, so gathering a group of people without a “sharia marriage” is not considered a family [56]. For this reason, the issue of maintaining cohabitation or marriage and family formation is important for MS patients according to the social and religious status of the present society, and it affects their self-compassion and requires measurement.
Being a role model for others was another new dimension. Factor analysis showed that it had three items. This means trying to convey positive experiences to others and support other patients, which was expressed as an indicator and a special feature of self-compassion. Some patients who were successful in adapting to the disease stated that they were trying to transfer their experiences to other patients. This also helped themselves to express self-compassion. As Louisa Ng indicates that peer support in chronic diseases is an effective source and tool for coping with stressful life experiences and gaining information and support from those who share a common experience [57].
Limitations of the study
One of the limitations of the present study is that this study was conducted on MS patients in the Iranian community, which may hamper the generalization of the results to populations of chronic patients in other societies. Therefore, it is suggested that in future research, this issue should be taken into consideration and investigated in another group with psychometrics.
This tool was designed for a specific group of Iranian patients; however, because it was designed based on the theory of Neff, including a healthy group in non-Iranian societies, our tool can be used for healthy people and even MS patients in other regions. It can be used even for other groups of chronic patients after psychometry. This tool can provide information to service providers to better identify self-compassion and self-care needs of MS patients to develop appropriate planning. Further research using this tool is recommended in other communities. This study was performed on MS patients. It is suggested to use this tool in communities and other groups of chronic patients after psychometric assessment.
Conclusion
The Self-Compassion Assessment Tool, developed and validated for patients with MS, has 73 items with 11 dimensions. The tool has good validity and reliability and is easy to use and score in the target group. In this tool, in addition to the dimensions of self-compassion based on the theory of Neff, there are 4 new dimensions. Self-compassion has other dimensions in patients with MS.
Acknowledgements: The authors would like to express their gratitude to all patients who participated in this study.
Ethical Permission: This study was approved by the Ethics Committee of Tarbiat Modares University (IR.MODARES.REC.1398.139). Autonomy, independence, confidentiality, and privacy of the participants were considered. Participants were informed about the study. Written and oral informed consent was obtained for taking notes or audio recordings. Participants were free to withdraw from the study at any time.
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Dahmardeh H (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (40%); Sadooghiasl A (Second Author), Introduction Writer/Methodologist/ Main Researcher/Discussion Writer (25%); Mohammadi E (Third Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (25%); Kazemnejad A (Fourth Author), Methodologist/Statistical Analyst (10%)
Funding: This study was one part of the Ph.D. dissertation by the first author (HD) that was supported financially by the research deputy of Tarbiat Modares University.
Multiple Sclerosis (MS) is a chronic, inflammatory, progressive and common autoimmune disease of the nervous system [1-3]. Most people suffer from it at a young age, around their 20s to 40s. With many debilitating symptoms and complications [2], it is the most common cause of neurological disability in adults [4].
The MS Atlas, compiled by the Multiple Sclerosis International Federation (MSIF), is an open-source global compendium of data regarding the epidemiology of MS and the availability of resources for people with MS reported at country, regional and global levels. The first edition was produced in 2008 in collaboration with the World Health Organization (WHO) and was updated in 2013 [5]. Based on that, a total of 2.8 million people are estimated to live with MS worldwide (35.9 per 100,000 population). MS prevalence has increased in every world region since 2013, but gaps in prevalence estimates persist. The pooled incidence rate across 75 reporting countries is 2.1 per 100,000 persons/year, and the mean age of diagnosis is 32 years. Females are twice as likely to live with MS as males [6].
People with MS learn most of their family and social responsibilities during their 20s to 40s; however, for MS patients, the disease does not allow them to become contributing individuals in their societies, as they may encounter difficulties in carrying out their tasks [1]. Patients’ early symptoms and complications, such as visual impairments, pain, urinary incontinence, and weakness can threaten their independence and ability to effectively participate in society and their families, which in turn affects all aspects of their everyday lives [2].
Considering the features of this disease, and as the number of individuals suffering from MS is increasing [2], concerns have been raised regarding the quality of life and healthcare expenses of these patients. The impact and effectiveness of self-care have been observed before in patients’ medical and personal outcomes [7]. Self-care can reduce patients’ expenses, improve their quality of life, and it should be noted that its significance has been evident in patients’ medical and person-centered results [8].
The concept of self-compassion has a key role in self-care [9], and it can especially be observed in patient’s self-caring behavior in chronic diseases [10]. The significance of self-compassion is elaborated further by Mills et al., who found that self-compassion and self-care behaviors are directly correlated [11]. Additionally, Nery-Hurwit et al. strongly emphasized that MS patients require measures like self-compassion to perform better self-care [12]. The direct correlation between these two concepts requires further attention [11]. As it has been confirmed in other studies that have investigated other patients, self-compassion increases MS patients’ ability and mental attitude, which also ensures better outcomes [12].
Self-compassion is an adaptive way to communicate with oneself when aware of inadequacies and cope with difficult living conditions such as life-threatening condition and chronic illnesses [13]. Self-compassion as a psychological construct has a significant effect on the care and treatment of chronic patients [14-16]. The ability of self-compassion when feeling inadequacy, such as physical disability, enhances a person's ability to accept their situation better. Therefore, if self-compassion is reinforced in MS patients who are living with a chronic illness, they might change their mental attitude towards the situation [12].
A prerequisite for any action to promote self-compassion is to measure it using specific tools appropriate to the target group [14-16]. For the first time in the United States, Neff explained the concept of self-compassion, and based on designed and validated the only tool available for measuring it. The questions in this scale measure six components, including self-kindness, feeling isolated, self-judgment, mindfulness, common humanity, and over-identification [17]. This tool is not specific to a specific group and is used in all communities and groups.
After Neff, qualitative studies were conducted to examine the meaning of self-compassion in different communities and groups [18, 19]. The results of these studies showed that although Neff has defined six components, self-compassion has other components as well. For example, the results of a study by Freeman added the component of seeking support to the dimensions introduced by Neff [20]. These results indicate that the concept of self-compassion can have different definitions in varied situations and populations and therefore have different components than what Neff introduced. In addition, various investigations have been conducted to assess the psychometry of Neff tool in different groups and countries [21-27]. The results of these studies showed that the six dimensions introduced in the Neff tool are not repeated in these studies, i.e., people had different perceptions of self-compassion according to factors such as life experiences, cultural conditions, and values [28]. Hence, it can be said that these factors affect the self-compassion of individuals in different societies.
Experts believe that the content of a tool should be extracted directly from people who would use it. However, it should be coordinated to the culture of communities and countries in which the tool is to be used [29]. Therefore, planning to promote self-compassion in MS patients requires measuring it using appropriate and accurate tools. Consequently, the present study aimed to design and evaluate self-compassion assessment tools in MS patients to obtain more accurate information about their culture and values for planning to maintain and improve their mental and psychological status.
Instrument and Methods
This instrumentation study was conducted as a sequential-exploratory combined design. In the first stage, qualitative data were collected and analyzed, and in the quantitative stage, the scale was designed and its psychometric properties were tested. The present study consisted of three phases, including construct definition, item generation, and testing psychometric characteristics of the instrument performed from December 2019 to July 2020.
Sample and setting
The samples should be representative of the target community [30]. Therefore, for sampling, patients from different ethnic groups in Iran were selected from the MS associations of Zahedan, Ahvaz, Kerman, East Azerbaijan, Ardabil, Yazd, Fasa, Astara, Amol, Sabzevar and North Khorasan.
Participants were purposefully selected from among MS patients who had been diagnosed for at least six months and had received treatment for at least six months. The setting of the study was hospitals and communities of Zahedan and Tehran Province, Iran.
The first phase: Construct definition
In the first phase, a qualitative study was performed using a guided content analysis according to self-compassion theory of Neff. Individual semi-structural interviews were performed to collect data. The duration of the interview was 15 to 55 minutes, with an average of 28 minutes. The place and time of the interview were determined according to participants’ preference. At the beginning of the interview, the purpose of the study was explained for the participants, and after receiving demographic information, they answered the main questions of the interview. The questions were redesigned based on the components of Neff's self-compassion theory. According to the participants' answers, exploratory questions were used to extract more data from their experiences. All interviews were recorded and transcribed. Then it was analyzed using the Directed Content Analysis method. This method was proposed in 2005 by Hsieh and Shannon [31].
The second phase: Item generation
In this phase, a theoretical and operational definition was determined for each of the main classes formed in the qualitative stage. The extraction of items depended on the definition of each of the dimensions and structures of the concept under study. The questionnaire questions were designed to include the dimensions of self-compassion mentioned by the participants in their interviews. At the end of this stage, an initial draft of the scale was prepared.
The third phase: Testing psychometric characteristics of the instrument
At this stage, the face and content validity of the structure and the reliability of the instrument were evaluated. To determine the face validity, two qualitative and quantitative methods were used. To determine the qualitative face validity, 10 potential users of the questionnaire (MS patients) were interviewed face to face regarding the difficulty level (recognizing items, phrases or words that are difficult for them to understand), the degree of appropriateness (appropriateness and proper relationship of the phrases with the dimensions of the questionnaire) and ambiguity (the possibility of misunderstandings or the existence of inadequacies in the meanings of the words). Then their opinions were reviewed and applied.
To evaluate the quantitative face validity, the impact score method was used. In this way, 10 patients were asked to rate the importance of each item on a 5-point Likert scale (quite important = 5, somewhat important = 4, moderately important = 3, slightly important = 2, it does not matter at all = 1). These patients were suffering from MS and were selected purposefully. The completed questionnaires at this stage were assessed with the formula as follows:
Impact score = frequency (%) × importance
A score of 1.5 and above indicated the appropriateness of the item.
To evaluate the validity of qualitative content, the opinion of experts (n=14) who had rich knowledge and experience in instrumentation, ethics, self-compassion, psychology, psychiatric nursing, and MS was obtained. The items were evaluated in terms of the level of difficulty, ambiguity, Persian grammar, use of appropriate words, and placement of words in their proper place.
To evaluate the validity of quantitative content, two methods of content validity ratio (CVR) and content validity index (CVI) were used. In the CVR index, the necessity of an item was evaluated from the perspective of experts (n=14). To calculate the CVR, each expert was asked to review each item based on a three-part spectrum: 1) necessary, 2) useful but not necessary, and 3) not necessary, then the answers were used to calculate the CVR. In this study, the minimum value of CVR index was considered as 0.51, regarding that each item was reviewed by 14 panel members [32].
For the content validity index, the relevance of items to the construct was measured from the perspective of experts. In this method, at the item level, Waltz and Basel's (1983) proposed formula was used to calculate the CVI: thus, the number of specialists who gave each question a score of 3 and 4 was divided by the total number of rankers (I-CVI). Besides, it was considered at the instrument level (S-CVI) [32].
After calculating the CVI based on the aggregation of the number of agreeing on points for each item (ranking 3 and 4 in the 4-point scale), relevance of an item was checked based on a score greater than 0.79 at the item level, and a score greater than 0.90 at the tool level [33].
In this way, from the 78 primary extracted items, after calculating the item impact score index with values higher than 1.5, content validity ratio higher than 0.51, and content validity index higher than 0.79, 73 items were selected and entered the factor analysis stage.
To evaluate the construct validity, Confirmatory Factor Analysis (CFA) and Exploratory Factor Analysis (EFA) methods were used. Since this study was designed based on Neff theory [34], CFA method was used first for items related to the constructs of Neff theory and Freeman's study because CFA is a confirmatory and theory-based method [35]. Then, for four structures added in this study to the classes introduced by Neff, EFA exploratory factor analysis was used [33, 36].
In the confirmatory factor analysis stage, the questionnaire was completed by 341 patients with MS (approximately 5 times the number of items) by purposive sampling. In investigations based on factor analysis, samples must represent the target population to achieve valid factors [30]. Therefore, for sampling, patients were selected from all over the country from MS associations in different cities.
Goodness of fit indices were used to assess the fit of confirmatory factor analysis, and items with a factor load above 0.3 were retained and approved [37].
Exploratory factor analysis was then performed for four new components, including concealment, spiritual resilience, concern for cohabitation, and being a role model for others. The Kaiser-Meyer-Olkin index test was used to determine the appropriateness of the sample size. Bartlett’s test of Sphericity was also used to evaluate the appropriateness of exploratory factor analysis. To determine the number of factors, the Eigenvalues (the sum of squared component loadings for each component) greater than one, the diagram of Scree Kettel (elbow point) and the percentage of variance greater than 5% were considered.
To determine the reliability of the questionnaire, two methods were used. First, the reliability of stability was performed using the test-retest method, which was measured 14 days later. Second, the information obtained from completing the self-compassion questionnaire by 51 patients with MS was used. Internal consistency was evaluated by Cronbach's alpha coefficient method performed by information extracted from 113 patients with MS after completion of the self-compassion questionnaire, and values equal to or greater than 0.7 were accepted. Statistical analysis was performed using SPSS 21 software.
Findings
Construct definition phase
In the qualitative phase, 11 categories were considered, including self-kindness, self-judgment, common humanity, isolation, mindfulness and over-identification (6 dimensions of Neff study), seeking support (Freeman), concealment, spiritual resilience, concern for living together, and role-playing for others. In the present study, in addition to replicating the 6 dimensions of the Neff study [34] and the Freeman “seeking support” dimension [20], 4 new dimensions were added to self-compassion.
Self-compassion in the MS patient means that when patients face such unpleasant conditions, they express “self-kindness” for self-compassion, in addition, “adhere to their treatment” and feel confident and valued, instead of “blaming themselves for the disease”. They consider the disease as a "human experience" that can happen to anyone, rather than finding themselves alone in the situation. They also respond in a "balanced way" to the discomfort they experience, rather than "magnifying" it in their minds and thinking of paralysis and disabilities. On the other hand, with the help and establishment of a "communication with a transcendental force", they create the capacity for relaxation and “seek support" from the family and their treatment team. Sometimes, due to the circumstances of the disease, they "hide" from others in order to avoid experiencing pity. They are also "concerned about their cohabitation." They inspire and guide their peers by trying to "be an example" for their peers. They experience a sense of self-compassion by connecting with others and making time for them.
A comparison of the above definition with the Neff's definition of self-compassion shows that the themes of "spiritual resilience", "worrying about the future of cohabitation", "hiding", and "being a role model for others" are new features added to Neff's definition of self-compassion.
Item generation phase
In this phase, items were extracted for each of the classes obtained from the qualitative stage. The items were examined by the members of the research team to ensure the accuracy and to find any overlapping and duplicate items. Duplicate items were removed, and some items were merged. Finally, the initial draft of the questionnaire was designed with 78 items.
Quantitative phase
Validity
To determine the qualitative face validity, 10 participants examined the tool. For example: "Item No. 44 - When the sensory symptoms of the disease occur, I try to alleviate it with a method such as using cold water to cool myself", which was difficult for most participants to understand, but remained without change to retain quantitative face validity and obtained an impact factor of 1.86, which was acceptable and was retained for the content validity stage, but was eventually removed from the questionnaire due to not obtaining a sufficient score in the next stages.
In the evaluation of quantitative face validity, 4 items obtained an impact factor score of less than 1.5 and were considered unacceptable. However, these items were retained for content validity review, and in the end, two of the 4 items remained due to good content validity.
In the quantitative content validity stage, 7 items of self-kindness (2 items), self-judgment (1 item), common humanity (1 item), mindfulness (2 items), and self-modeling (1 item) were removed due to not receiving sufficient CVR and CVI scores, leaving 71 items. On the other hand, 2 new items were added to the category of" being a role model for others" according to the results of qualitative validity content based on the research team's opinion. At the end of this stage, 73 items remained in the content validity stage due to obtaining sufficient CVR and CVI scores as well as an acceptable impact score in the face validity stage and were finalized.
The S-CVI score at the instrument level considered to be more than 0.90, which in this study, after removing the items that did not obtain a sufficient CVR and CVI scores, the S-CV was calculated as 0.93.
Construct validity
In total, 341 participants filled in the questionnaires in the quantitative phase. There were 266 females (78%) and 75 males (22%), 237 married (69.5%), and 104 single (30.5%). The mean age of participants was 34.69 years. The mean duration of the disease was 76.1 months (Table 1).
Table1) Frequency distribution of characteristics of the study participants (n=341)

The results of confirmatory factor analysis for structures based on Neff's theory and Freeman's study (self-kindness, self-judgment, common humanity, isolation, mindfulness, over-identification, and search for support) are shown in Table 2. The four indices were fit in the acceptable intervals; hence the model was confirmed according to the confirmatory factor analysis.
Table 2) Confirmatory factor analysis results
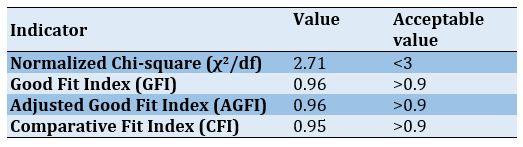
To examine the confirmatory factor analysis, the factors were defined by the symbol F (abbreviation for Factor) as follows: Factors F1 to F7, respectively, indicate self-kindness, self-judgment, common humanity, isolation, mindfulness, over-identification and seeking support (Figures 1-7).
Exploratory factor analysis
At the beginning of factor analysis, to determine the possibility of factorization, the appropriate adequacy measurement index test in the samples, Kaiser-Meyer-Olkin (KMO), and Bartlett's test of sphericity were used (Table 3).

Figure 1) Factor loads of self-kindness
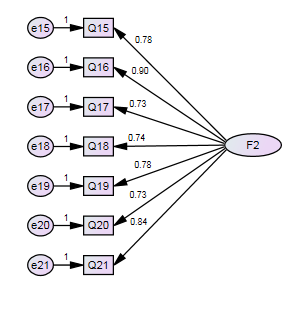
Figure 2) Factor loads of self-judgement
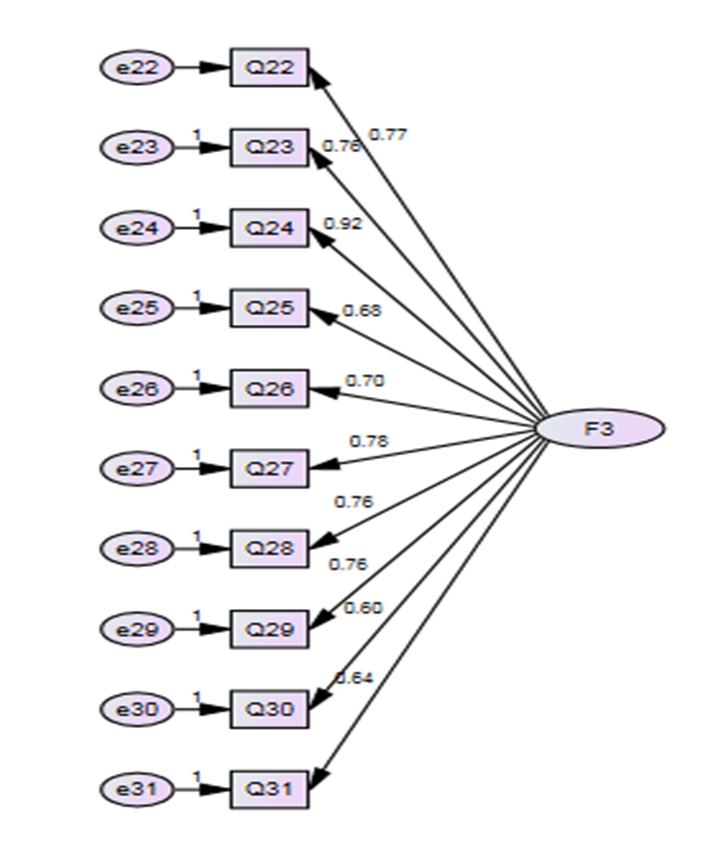
Figure 3) Factor loads of common humanity
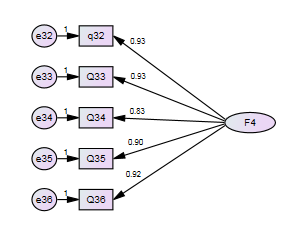
Figure 4) Factor loads of isolation
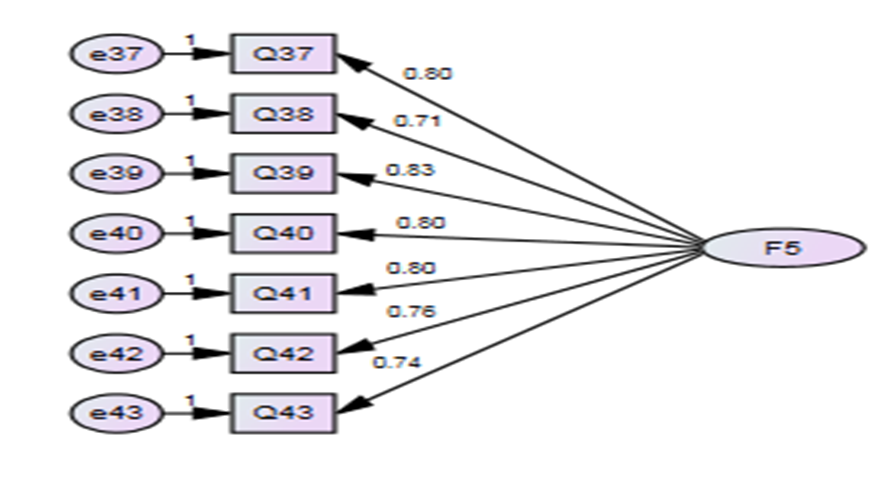
Figure 5) Factor loads of self-identification
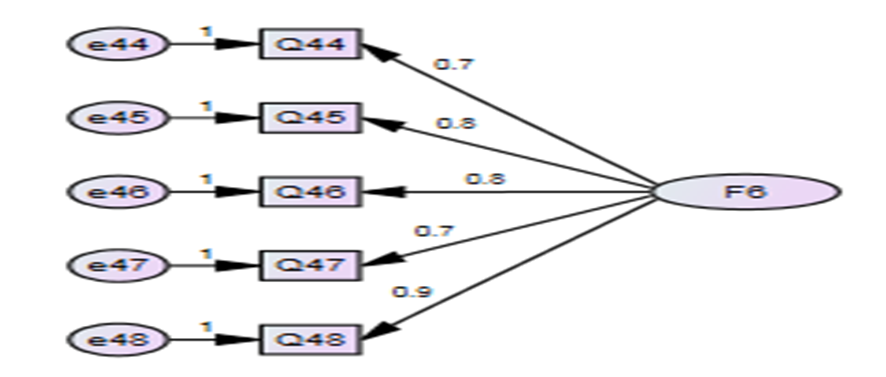
Figure 6) Factor loads of over-identification
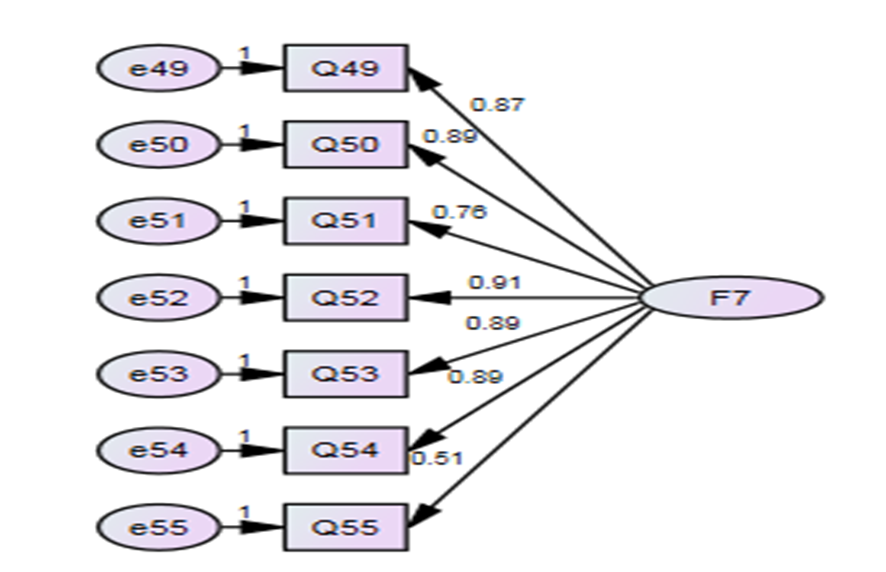
Figure 7) Factor loads of seeking support
Table 3 shows the Kaiser Meyer-Olkin sampling index equal to 0.803, based on which a good sampling of variables has been done based on the pairwise correlation of the reagents and their partial correlation. Also, the null hypothesis of the sphericity test in data was rejected (p<0.000), and the KMO test was confirmed. Therefore, it can be concluded that the implementation of exploratory factor analysis provided a suitable model for the present data and factor detection was possible, and the items were sufficient enough to predict the factors.
Table 3) Results of KMO and Bartlett tests

The results of explained variance values for the extraction of 4 new factors showed that with a specific eigenvalue above 2.441, they were able to predict 63.254 of total changes in self-compassion in patients with MS, which is a desirable value [38]. In this study, a factor load of 0.4 was determined as the minimum degree of acceptable correlation between each item and the extracted factors.
Eighteen items with a factor load of more than 0.4 in 4 factors included spiritual resilience (6 items), being a role model for others (3 items), worrying about cohabitation (5 items), and concealment (4 items). Three items from the category of “concerned with cohabitation” were transferred to the class of spiritual resilience because they were conceptually and semantically more similar. At this point, all questions were saved, and no item was deleted. At the end of this stage, a questionnaire with 73 items was prepared to check reliability.
Reliability
To determine the internal consistency of the questionnaire, Cronbach's alpha coefficient was calculated to be 0.813, which showed that the questionnaire had an acceptable internal consistency. Also, to determine the stability of the questionnaire, retest test and calculation of intra-cluster correlation were used. The questionnaire was completed by 51 people in two stages, and the results were equal to 0.778 with a confidence interval of 0.854-0.689 and showed a good stability (Table 4).
Scoring
For the final questionnaire, a 5-point Likert scale was considered. In scoring the items, all had a positive meaning as the score of 5 indicates always, 4 more often, 3 occasionally, 2 rarely, and 1 never. Based on the above scoring and the number of items in the questionnaire, the minimum total score of the questionnaire was 73, and the maximum was 365.
Table 4) The results of determining the reliability of the self-compassion measurement tool in patients with MS
Discussion
The aim of this study was to design a self-compassion assessment tool in patients with MS disease. The tool items were based on 6 constructs of self-kindness, self-judgment, common humanity, isolation, mindfulness and over-identification of Neff theory and Freeman support search construct and 4 newly developed constructs of spiritual resilience, concealment, concern for cohabitation and role modeling designed based on the results of a qualitative study in MS patients with special life conditions. Psychometric findings indicated the validity and reliability of the designed questionnaire.
The first dimension of the present study tool was "self-kindness", which had 14 items. In the Neff study, which examined healthy individuals, the development of kindness and self-awareness were replaced instead of misjudgment in times of distress [34]. However, in the present study, new features of diet and medication adherence, feeling self-confidence and self-worth, and more attention to self were added to the construct. Sirois and Hirsch showed that self-compassion had been effective in adhering to treatment in patients with fibromyalgia, chronic fatigue syndrome, and cancer patients, which were probably due to the effect of self-compassion on reducing stress [39]. In the present study, MS patients, like those with cancer or chronic fatigue syndrome, perceived and experienced adherence to treatment and care along with a sense of self-confidence and self-worth as three other indicators of self-compassion.
The next dimension was "self-judgment", including 7 items, which was defined in Neff study as self-judging and blame in failure or pain and unhappiness [34]. While in the present study, new features of feeling insignificant to others and mental conflict about why they suffer from the disease were also added to the construct. The reason these features were added to the self-judgment structure is related to MS itself, which changes the body and affects how people treat them or vice versa. The results of a study by Jones et al. showed that patients with MS feel rejected and worthless because of the disease, and this leads to their isolation and reduced social relationships [40].
Many questions, negative ideas, and thoughts about the cause of the disease arise in the minds of patients with MS. Güner et al. stated that these negative automatic thoughts and dysfunctional attitudes are risk factors for developing depression and anxiety in individuals who have recently been diagnosed with the disease [41]. However, people with higher self-compassion have a lower risk of depression and anxiety than those without it [42]. Therefore, in this tool, these items were highlighted and considered.
Another dimension of the present study tool was common humanity, including 10 items. The items related to the positive mood reinforcement class in this dimension were somewhat consistent with the items of Neff tool. But in the present study, a new feature of “trying to play their role as before the disease” was added to this structure.
The next dimension was isolation, including 5 items. The items related to having negative self-image and isolation were consistent with the items of Neff tool; however, a tendency for isolation and social distancing was another new item different from Neff theory. The experience of loneliness is characteristic of MS [43]. These people often withdraw from participating in social activities [44]. In line with the results of the present study, Beal and Stuifbergen showed that women with MS may be exposed to loneliness due to social network changes that occur during chronic illness [45], so it is important to pay attention to loneliness and evaluate it in self-compassion.
Another dimension of the present study was mindfulness, including 7 items. Items related to categories of “trying to forget and not thinking about the illness and its negative aspects”, “accepting and coping with illness”, and “not blaming oneself for the illness” were consistent with the statements of the Neff tool. However, the present study added “adapting and accepting difficult treatment regimen with self-improvement”, “turning bad feelings into good ones about the disease”, and “changing attitudes to the illness” to the characteristics of Neff's mindfulness item. Patients with MS try to adapt to new changes and limitations in their life due to unpleasant and unpredictable symptoms, difficult treatment regimens, and uncertainty about the future of the disease [46]. In the present study, adaptation and acceptance of difficult treatment was achieved with self-improvement and self-compassion, so five items were designed to measure these items in patients with MS.
The sixth dimension of the present study tool was over-identification, including 5 items. In this respect, the items were conceptually consistent with the items of Neff theory. However, according to the findings of this study, there were more characteristics, including perception and worry about the progression of the disease by seeing patients with advanced condition, fear of paralysis and severe disability and thinking about it, and unwillingness to accept the disease and disabilities. Patients with chronic diseases are always afraid of the progression of the disease with all its consequences [47]. In the present study, due to the chronic nature of the disease, patients with MS were always afraid of the progression of the disease and their condition worsening and eventually paralysis, and thought about it a lot. Therefore, to measure these cases, 3 items were designed to fit the target group.
As mentioned, Neff self-compassion tool had 6 dimensions, and new dimensions were added by the present study for patients with MS. The first new dimension was "spiritual resilience", including 9 dimensions. For many patients with chronic illness, spirituality/religiosity is an important source of coping [48]. In the Iranian and Islamic society of the present study, many behaviors in individual and social life are influenced by religious beliefs [49], and many people tolerate stressful conditions better by praying, reading spiritual books or attending religious ceremonies [50]. Patients with MS tried to be patient and tolerated it by relying on God and having religious beliefs, thus showing self-compassion. In line with the present results, the results of a qualitative study by Ebrahimi et al. described one of the characteristics perceived by MS patients following the illness as "the use of spirituality" [51].
Searching for support was another new dimension with 7 items. MS patients perceived and expressed it as having a positive view of the attention and support of others and encouragement to their possessions and support of the family and their physician. In line with the results of the present study, Ghafari et al. expressed "support seeking" as one of the characteristics perceived by MS patients in the process of adapting to this disease [46].
Another new dimension was concealment with 4 items. MS patients expressed it as hiding the disease from others to avoid their pity and the following discomfort, thinking of themselves, and not expecting from others. In the present study, this dimension was compared with the dimension of seeking support, and some patients preferred to hide their illness instead of seeking support for a self-compassion to avoid pitiful treatment of others. The results of Earnshaw et al. study showed that MS patients, like other chronic patients, tolerate stigma [52]. Stigma is a threat that is related to cultural characteristics. In European cultures, they strongly emphasize individualistic norms and independent self-concept, while Asian cultures emphasize on collective norms and mutual self-concept. Likewise, In Iran, due to a culture of collectivism, patients are concerned about the way others look at them [53]. Thus, they try to hide their illness from others to avoid increased support from sympathetic people and prefer isolation [54].
Another new dimension found in this study was "concern about cohabitation" with two items shown by factor analysis. The onset of symptoms in MS is usually around the third or fourth decade of life, which is the age of childbearing, family growth, and the establishment and strengthening of social and marital relationships. In these patients, the challenge of coping with the disease, relationship problems, and sexual dysfunction are among the factors that threaten the emotional relationship between couples. As a result of the disease, the needs of spouses are often ignored and might harm the marital relationship leading to a possible loss of a sexual partner [55].
Another important issue is that in each country, the formation of a family has its own definition according to the accepted customs and laws. In the Iranian legal system, which is derived from the Islamic intellectual system, marriage is necessary to form a family, so gathering a group of people without a “sharia marriage” is not considered a family [56]. For this reason, the issue of maintaining cohabitation or marriage and family formation is important for MS patients according to the social and religious status of the present society, and it affects their self-compassion and requires measurement.
Being a role model for others was another new dimension. Factor analysis showed that it had three items. This means trying to convey positive experiences to others and support other patients, which was expressed as an indicator and a special feature of self-compassion. Some patients who were successful in adapting to the disease stated that they were trying to transfer their experiences to other patients. This also helped themselves to express self-compassion. As Louisa Ng indicates that peer support in chronic diseases is an effective source and tool for coping with stressful life experiences and gaining information and support from those who share a common experience [57].
Limitations of the study
One of the limitations of the present study is that this study was conducted on MS patients in the Iranian community, which may hamper the generalization of the results to populations of chronic patients in other societies. Therefore, it is suggested that in future research, this issue should be taken into consideration and investigated in another group with psychometrics.
This tool was designed for a specific group of Iranian patients; however, because it was designed based on the theory of Neff, including a healthy group in non-Iranian societies, our tool can be used for healthy people and even MS patients in other regions. It can be used even for other groups of chronic patients after psychometry. This tool can provide information to service providers to better identify self-compassion and self-care needs of MS patients to develop appropriate planning. Further research using this tool is recommended in other communities. This study was performed on MS patients. It is suggested to use this tool in communities and other groups of chronic patients after psychometric assessment.
Conclusion
The Self-Compassion Assessment Tool, developed and validated for patients with MS, has 73 items with 11 dimensions. The tool has good validity and reliability and is easy to use and score in the target group. In this tool, in addition to the dimensions of self-compassion based on the theory of Neff, there are 4 new dimensions. Self-compassion has other dimensions in patients with MS.
Acknowledgements: The authors would like to express their gratitude to all patients who participated in this study.
Ethical Permission: This study was approved by the Ethics Committee of Tarbiat Modares University (IR.MODARES.REC.1398.139). Autonomy, independence, confidentiality, and privacy of the participants were considered. Participants were informed about the study. Written and oral informed consent was obtained for taking notes or audio recordings. Participants were free to withdraw from the study at any time.
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Dahmardeh H (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (40%); Sadooghiasl A (Second Author), Introduction Writer/Methodologist/ Main Researcher/Discussion Writer (25%); Mohammadi E (Third Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (25%); Kazemnejad A (Fourth Author), Methodologist/Statistical Analyst (10%)
Funding: This study was one part of the Ph.D. dissertation by the first author (HD) that was supported financially by the research deputy of Tarbiat Modares University.
Article Type: Descriptive & Survey |
Subject:
Spiritual Health
Received: 2022/09/13 | Accepted: 2022/11/13 | Published: 2022/12/20
Received: 2022/09/13 | Accepted: 2022/11/13 | Published: 2022/12/20
References
1. Abedini E, Ghanbari Hashem-Abadi BA, Talebian-Sharif J. Effectiveness of group therapy based on hope approach on hope and depression in women with multiple sclerosis. J Clin Psychol. 2016;8(2):1-11. [Persian] [Link]
2. Dahmardeh H, Vagharseyyedin SA, Amiri Fard H, Sharif-zadeh GR, Rakhshani-Zabol F. Effect of self-care educational program based on Orem's theory on hope in patients with multiple sclerosis. Medical - Surgical Nursing Journal. 2015;4(2):57-63. [Persian] [Link]
3. Correale J, Gaita'n MI, Ysrraelit MC, Fiol MP. Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain. 2017;140(30):527-46. [Link]
4. Karussis D. The diagnosis of multiple sclerosis and the various related demyelinating syndromes: A critical review. J Autoimmun. 2014;48-49:134-42. [Link] [DOI:10.1016/j.jaut.2014.01.022]
5. Browne P, Chandraratna D, Angood C, Tremlett H, Baker C, Taylor BV, et al. Atlas of multiple sclerosis 2013: A growing global problem with widespread inequity. Neurology 2014;83(11):1022-4. [Link] [DOI:10.1212/WNL.0000000000000768]
6. Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie R, et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Mult Scler. 2020;26(14):1816-21. [Link] [DOI:10.1177/1352458520970841]
7. Jaarsma T, Cameron J, Riegel B, Stromberg A. Factors related to self-care in heart failure patients according to the middle-range theory of self-care of chronic illness: a literature update. Curr Heart Fail Rep. 2017;14(2):71-7. [Link] [DOI:10.1007/s11897-017-0324-1]
8. Wilkinson A, Whitehead L. Evolution of the concept of self-care and implications for nurses: A literature review. Int J Nurs Stud. 2009;46(8):1143-7. [Link] [DOI:10.1016/j.ijnurstu.2008.12.011]
9. Sinclair S, Kondejewski J, Raffin-Bouchal S, King-Shier KM, Singh P. Can self-compassion promote healthcare provider well-being and compassionate care to others? Results of a systematic review. Appl Psychol Health Well Being. 2017:9(2):168-206. [Link] [DOI:10.1111/aphw.12086]
10. Ferrari M, Dal Cin M, Steele M. Educational and psychological aspects Self-compassion is associated with optimum self-care behaviour, medical outcomes and psychological well-being in a cross-sectional sample of adults with diabetes. Diabet Med. 2017;34(11):1546-53. [Link] [DOI:10.1111/dme.13451]
11. Mills J, Wand T, Fraser JA. Examining self-care, self-compassion and compassion for others: a cross-sectional survey of palliative care nurses and doctors. Int J Palliat Nurs. 2018;24(1):4-11. [Link] [DOI:10.12968/ijpn.2018.24.1.4]
12. Nery-Hurwit M, Yun J, Ebbeck V. Examining the roles of self-compassion and resilience on health-related quality of life for individuals with multiple sclerosis. Disabil Health J. 2018;11(2):256-61. [Link] [DOI:10.1016/j.dhjo.2017.10.010]
13. Moszadeh S. Effectiveness of self-directed group training on reducing the stress of parenting and increasing parental self-efficacy and resilience of mothers of children with autism spectrum disorder [Dissertation]. Mashhad: Mashhad Ferdowsi University; 2017. [Link]
14. Pinto-Gouveia J, Duarte C, Matos M, Fráguas S. The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clin Psychol Psychother. 2014; 21(4):311-23. [Link] [DOI:10.1002/cpp.1838]
15. Neff KD. The development and validation of a scale to measure self-compassion. Self Ident. 2003;2(3):223-50. [Link] [DOI:10.1080/15298860309027]
16. Wren AA, Somers TJ, Wright MA, Goetz MC, Leary MR, Fras AM, et al. Self-compassion in patients with persistent musculoskeletal pain: Relationship of self-compassion to adjustment to persistent pain. J Pain Symptom Manag. 2012;43(4):759-70. [Link] [DOI:10.1016/j.jpainsymman.2011.04.014]
17. Kachooei M, Hasani J, Moradi A, Fathi-Ashtiani A. Comparison of dispositional mindfulness and self-compassion among women with normal and high body-mass-index. Community Health. 2018;5(2):103-12. [Persian] [Link]
18. Rickers S. The lived experience of self-compassion in social workers [Dissertation]. Minneapolis: The University of Minnesota; 2012. [Link]
19. Klingle KE, Van Vliet KJ. Self-compassion from the adolescent perspective: A qualitative study. J Adolesc Res. 2017:34(3):1-24. [Link] [DOI:10.1177/0743558417722768]
20. Freeman S. Emotions in teaching: Self-compassion [Dissertation]. Provo, Utah, United States: Brigham Young University; 2016. [Link]
21. López A, Sanderman R, Smink A, Zhang Y, van Sonderen E, Ranchor A, et al. A reconsideration of the self-compassion scale's total score: Self-compassion versus self-criticism. PLoS One. 2015;10(7):e0132940. [Link] [DOI:10.1371/journal.pone.0132940]
22. Costa J, Marôco J, Pinto-Gouveia J, Ferreira C, Castilho P. Validation of the Psychometric Properties of the Self-Compassion Scale. Testing the factorial validity and factorial invariance of the measure among borderline personality disorder, anxiety disorder, eating disorder and general populations. Clin Psychol Psychother. 2016;23(5):460-8. [Link] [DOI:10.1002/cpp.1974]
23. Hupfeld J, Ruffieux N. Validierung einer deutschen version der self-compassion scale (SCS-D). Zeitschrift für Klinische Psychol und Psychother. 2011;40(2):115-23. [German] [Link] [DOI:10.1026/1616-3443/a000088]
24. Halamová J, Kanovský M, Pacúchová M. Self-compassion scale: IRT psychometric analysis, validation, and factor structure - Slovak translation. Psychol Belg. 2018;57(4):190-209. [Link] [DOI:10.5334/pb.398]
25. Eirini K, Christos P, Michael G, Anastasios S. Validity, reliability and factorial structure of the self-compassion scale in the Greek population. J Psychol Psychother. 2017;7(4):1-6. [Link] [DOI:10.4172/2161-0487.1000313]
26. Tanenbaum ML, Adams RN, Gonzalez JS, Hanes SJ, Hood KK. Adapting and validating a measure of diabetes-specific self-compassion. J Diabetes Complications. 2018;32(2):196-202. [Link] [DOI:10.1016/j.jdiacomp.2017.10.009]
27. Elices M, Carmona C, Pascual JC, Feliu-Soler A, Martin-Blanco A, Soler J. Compassion and self-compassion: Construct and measurement. Mindful Compass. 2017;2(1):34-40. [Link] [DOI:10.1016/j.mincom.2016.11.003]
28. McGehee P, Germer C, Neff K. Core values in mindful self-compassion. In Monteiro LM, Compson JF, Musten F, editors. Practitioner's guide to ethics and mindfulness-based interventions. Springer; 2017. p. 279-93. [Link] [DOI:10.1007/978-3-319-64924-5_11]
29. Shahhosseini ZSM, Ramezankhani A, Majd HA. Designing and psychometric properties of a questionnaire for assessing female adolescents' health needs. J Sch Public Health. 2011;9(1):11-22. [Persian] [Link]
30. Kline P. An easy guide to factor analysis. London: Routledge; 2014. [Link] [DOI:10.4324/9781315788135]
31. Hsieh HF, Shannon SE. Three approach to qualitative content analysis. Qual Health Res. 2005;15(9):1277-88. [Link] [DOI:10.1177/1049732305276687]
32. Ebadi A, Zarshenas L, Rakhshan M, Zareiyan A, Sharifinia H, Mjahedi M. Priniciples of scale development in health science. 1st Edition. Tehran: Jameenegar; 2017. [Persian] [Link]
33. Waltz CF. Nursing research: design statistics and computer analysis. Philadelphia: Davis FA; 1981. [Link]
34. Neff K. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Ident. 2003;2(2):85-101. [Link] [DOI:10.1080/15298860309032]
35. Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J Educ Res. 2006;99(6):323-38. [Link] [DOI:10.3200/JOER.99.6.323-338]
36. Polit DF, Yang FM. Measurement and the measurement of change: A primer for the health professions. Wolters Kluwer, 2016. [Link]
37. Haynes CA, Miles J, Clements K. A confirmatory factor analysis of two models of sensation seeking. Person Indiv Differ. 2000;29(5):823-39. [Link] [DOI:10.1016/S0191-8869(99)00235-4]
38. Klein P. Easy guide to factor analysis. Sadrissadat J, Minaei A, translators. 1st Edition. Tehran: Samat; 2001. [Persian] [Link]
39. Sirois FM, Hirsch JK. Self-compassion and adherence in five medical samples: the role of stress. Mindfulness. 2019;10(1):46-54. [Link] [DOI:10.1007/s12671-018-0945-9]
40. Jones JB, Walsh S, Isaac C. The relational impact of multiple sclerosis: An integrative review of the literature using a cognitive analytic framework. J Clin Psychol Med Settings. 2017;34(3-4):316-40. [Link] [DOI:10.1007/s10880-017-9506-y]
41. Güner MC, Yazar MS, Meterelliyoz KS. Cognitive predictors of depression and anxiety in individuals with newly diagnosed multiple sclerosis. Eur J Psychiatry. 2020;34(4):202-10. [Link] [DOI:10.1016/j.ejpsy.2020.06.004]
42. Amanelahi A, Tardast K, Aslani K. Prediction of depression based on components of self- compassion in girl students with emotional breakdown experience in Ahvaz Universities. J Clin Psychol. 2016;8(2):77-87. [Persian] [Link]
43. Rokach A. Loneliness in cancer and multiple sclerosis patients. Psychol Rep. 2004;94(2):637-48. [Link] [DOI:10.2466/pr0.94.2.637-648]
44. Kalina JT, Hinojosa J. A protocol for improving loneliness in people with multiple sclerosis. Occup Ther Mental Health. 2016;32(2):130-45. [Link] [DOI:10.1080/0164212X.2015.1130106]
45. Beal CC, Stuifbergen A. Loneliness in women with multiple sclerosis. Rehabil Nurs. 2007;32(4):165-71. [Link] [DOI:10.1002/j.2048-7940.2007.tb00171.x]
46. Ghafari S, Fallahi-Khoshknab M, Nourozi K, Mohammadi E. Patients' experiences of adapting to multiple sclerosis: a qualitative study. Contemp Nurse. 2015;50(1):36-49. [Link] [DOI:10.1080/10376178.2015.1010252]
47. Nielsen J, Saliger J, Montag C, Markett S, Nöhring C, Karbe H. Facing the Unknown: Fear of progression could be a relevant psychological risk factor for depressive mood states among patients with multiple sclerosis. Psychother Psychosom. 2018;87(3):190-2. [] [DOI:10.1159/000487329]
48. Büssing A, Koenig HG. Spiritual needs of patients with chronic diseases. Religions. 2010;1(1):18-27. [Link] [DOI:10.3390/rel1010018]
49. Khaledian M, Arjmand Kermani R, Amini P. The effectiveness of spirituality education with emphasis on the teachings of Islam on resilience and social adjustment in drug addicts. Soc Health Addict. 2018;5(18):57-74. [Persian] [Link]
50. Baljani E, Khashabi J, Amanpour E, Azimi N. Relationship between spiritual well-being, religion, and hope among patients with cancer. Hayat. 2011;17(3):27-37. [Persian] [Link]
51. Ebrahimi H, Hasankhani H, Namdar H, Khodadadi E, Fooladi M. Dealing with chronic illness: Experiences of Iranian families of persons with multiple sclerosis- A qualitative study. Mult Scler Int. 2017;2017:9243161. [Link] [DOI:10.1155/2017/9243161]
52. Earnshaw VA, Quinn DM, Park CL. Anticipated stigma and quality of life among people living with chronic illnesses. Chronic Illn. 2012;8(2):79-88. [Link] [DOI:10.1177/1742395311429393]
53. Vaghee S, Salarhaji A. Stigma in family caregivers of patients with Schizophrenia Hospitalized in Ibn-Sina Psychiatric Hospital of Mashhad in 2014-2015. J Torbat Heydariyeh University Med Sci. 2015;3(3):23-30. [Persian] [Link]
54. Joachim G, Acorn S. Stigma of visible and invisible chronic conditions. J Adv Nurs. 2000;32(1):243-8. [Link] [DOI:10.1046/j.1365-2648.2000.01466.x]
55. Keykhaei A, Imani M, Faghihi H, Alikhah F. Marital quality in the spouses of men with multiple sclerosis: A descriptive comparative study. Int J Med Res Health Sci. 2016;5(11):415-23. [Link]
56. Azimpoor A, Papinejad F. Strategies to combat white marriage from the perspective of the Qur'an and narratives. J Women Strateg Stud. 2019;21(84):69-93. [Persian] [Link]
57. Ng L, Amatya B, Khan F. Outcomes of a peer support program in multiple sclerosis in an Australian community cohort: A prospective study. J Neurodegener Dis. 2013;2013:429171. [Link] [DOI:10.1155/2013/429171]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






