Volume 11, Issue 1 (2023)
Health Educ Health Promot 2023, 11(1): 79-87 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yasrebirad M, Mohammadkhan Kermanshahi S, Mohammadi E. A Grounded Theory of the Process of Improving the Quality of Life in Patients with Heart Disease. Health Educ Health Promot 2023; 11 (1) :79-87
URL: http://hehp.modares.ac.ir/article-5-62856-en.html
URL: http://hehp.modares.ac.ir/article-5-62856-en.html
1- Nursing Department, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
2- Nursing Department, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran, Tarbiat Modares University, Jalal e Al e Ahmad street Street, Tehran, Iran. Postal Code: 14115-111 (kerman_s@modares.ac.ir)
2- Nursing Department, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran, Tarbiat Modares University, Jalal e Al e Ahmad street Street, Tehran, Iran. Postal Code: 14115-111 (kerman_s@modares.ac.ir)
Full-Text [PDF 1570 kb]
(3305 Downloads)
| Abstract (HTML) (1977 Views)
Full-Text: (332 Views)
Introduction
Cardiovascular diseases are the leading cause of death in the world, with 17 million deaths per year [1, 2]. Studies in Iran have shown that cardiovascular diseases have the highest mortality rate compared to other diseases [3]. The first cause of death in Iran, with 39.3% of all deaths, is due to cardiovascular diseases, of which 19.5% are related to heart attack, 9.3% are due to stroke, 3.1% are related to hypertension and the rest related to other cardiovascular diseases [4]. Almost all heart diseases lead to some form of heart failure, which causes a variety of symptoms, such as shortness of breath, dizziness, angina, edema, and ascites [5, 6]. These symptoms lead to intolerance to activity [7, 8] and change the patient's lifestyle [9], which affects his satisfaction and quality of life [10-12].
Apart from poor prognosis and pain [10], these diseases cause limitations in physical activity, changes in physical condition [13], loss of job security, reduced recreational activity, fear and anxiety about the future, disruption of family roles, fear of death, and cessation of social interactions [14, 15]. Psychological distress (anxiety), decreased vitality, increased dependence, and early retirement impose a negative impact on quality of life [16-18]. Researchers have concluded that the symptoms of the disease are the most important predictors of quality of life, and with increasing severity of the disease, the quality of life decreases [15, 19, 20].
Abbasi et al. showed that the quality of life in patients with heart failure in physical, mental, psychological, social, and economic dimensions is in a better situation than most internal and external review studies, and only the average quality of life of the study sample in California was better than the present study, but the quality of life in these patients is still not in a good condition [21].
Quality of life is about people's perception of their position in life in terms of culture, value system in which they live, their goals, expectations, standards and priorities. So it is a completely subjective matter and not visible to others. And it is based on people's understanding of different aspects of life [16]. On the other hand, although professionals and service providers may be interested in changes in physical criteria to further improve their quality of life, patients are more likely to change their symptoms, physical function, and social roles [22].
Many nursing models have been designed, presented, and used over the past decades to provide targeted, coherent, and scientific nursing services, especially for chronic patients, which the quality of life in many of these theories, such as Roy, King, and Orem, indirectly are mentioned as the goal and consequence of care models. The main focus of these models is more on strategy and care interventions, but they have not said anything about improving the quality of life.
On the other hand, these theories are more adapted and inspired by concepts and knowledge of other disciplines such as sociology, psychology and management, and so on [23].
Therefore, for theorizing, instead of using the knowledge and theories of other fields or simply from the theorist's personal experiences, which is the dominant feature of nursing theories, the experiences of the main stakeholders, who are patients and their families, should be used. On the other hand, quality of life is an individual and mental phenomenon and is completely dependent on patients' perceptions and experiences, and people's efforts to improve quality of life are affected by individual, contextual, and cultural factors and conditions.
Therefore, since maximizing the quality of life is one of the main goals of treating heart patients, then in the first step, healthcare workers and researchers should obtain more information about the quality of life and the process of changing the different aspects of the quality of life of these patients and how to improve it; and in the second step, knowing the quality of life of patients with heart diseases and the factors affecting it by nurses can be a guide so that nursing diagnoses, measures, interventions, evaluation and adjustment of health education and health promotion programs during treatment and at the time of discharge, these variables should be considered.
This study aimed to explain the process of improving the quality of life of heart patients in Iran.
Participants and Methods
In this qualitative study, “the process of improving the quality of life in heart patients” was discovered using the method of grounded theory of the 2015 version of Strauss and Corbin. The participants in this study were patients with a variety of heart disorders who had a good understanding of the Persian language and were able to communicate verbally and tend to express their experiences. For creating maximum diversity of accurate knowledge of the factors involved in the process of improving the quality of life in these patients, participants were selected from different social classes, different stages of disease severity, and under different treatments for heart disease, including pacemaker, angioplasty, and open heart surgery. Sampling in the present study was first purposeful and then theoretical [24]. Sampling in qualitative research usually starts with purpose-based sampling, while with the emergence of conceptual classes during data analysis, participants are selected based on theoretical sampling to find the data in the direction of transparency and more accurate confirmation [25, 26].
The research environment was the heart and CCU wards of Shahid Rajaei Heart Hospital and Alborz Hospital (both in Karaj City), clinics, and homes. During the study, the researcher tried to determine the interview environment based on the ease of access of the participants and in a place where they were comfortable and willing to interview.
Data collection
Between October 25, 2020, and December 21, 2021, data collection was done by visiting the participants in the places mentioned. Individual interviews lasted for 25-60 min (30 min on average), and due to Coronavirus, the interviews were conducted via WhatsApp or phone call. The individual interviews were the main basis for data collection. In order to cover the most important areas of interest, the interviews began with broad-based, open questions with follow-up probes, with prompts such as, "How has this disease affected you and your life?" Continuing the interview was based on the answers to probing or exploratory questions, such as "What did you do to solve this problem?" The questions focused on how patients try to improve their quality of life and the issues, and problems and obstacles they face.
Data analysis
In the present study, Corbin and Strauss analysis method was used [27], which has steps, including open coding to identify concepts, development of concepts according to their characteristics and dimensions,
analyze data for context, process entry into analysis, and categories integration. The data was transcribed verbatim, and the analysis began after each interview. Throughout the whole process, data collection and coding were carried out simultaneously to explore, deepen, and refine questions, a process that contributed to the formation of new questions [28]. A constant comparative method was used to systematize and analyze data compare meanings and identify similarities and differences [27]. Texts were read line by line and labeled with codes based on phrases or names that were as close to the data as possible. Then, the codes were compared with each other based on similarities and differences. Once all the codes were identified and were starting to stand out, the next step of focused coding was followed to organize and group the data into temporary categories. Step by step, in line with the constant comparative method, the analyses were brought to a more abstract level that generated concepts confirmed by the properties of the data. During the whole process, memos were used to record reflections, questions, and ideas [29].
Study rigor
To increase the power and accuracy of the study, the researcher uses strategies such as maximum variation in sampling, long-term engagement with data, continuous comparative analysis, control by participants in the research, expert review, taking evidence-based note-taking, and using citations [30].
Findings
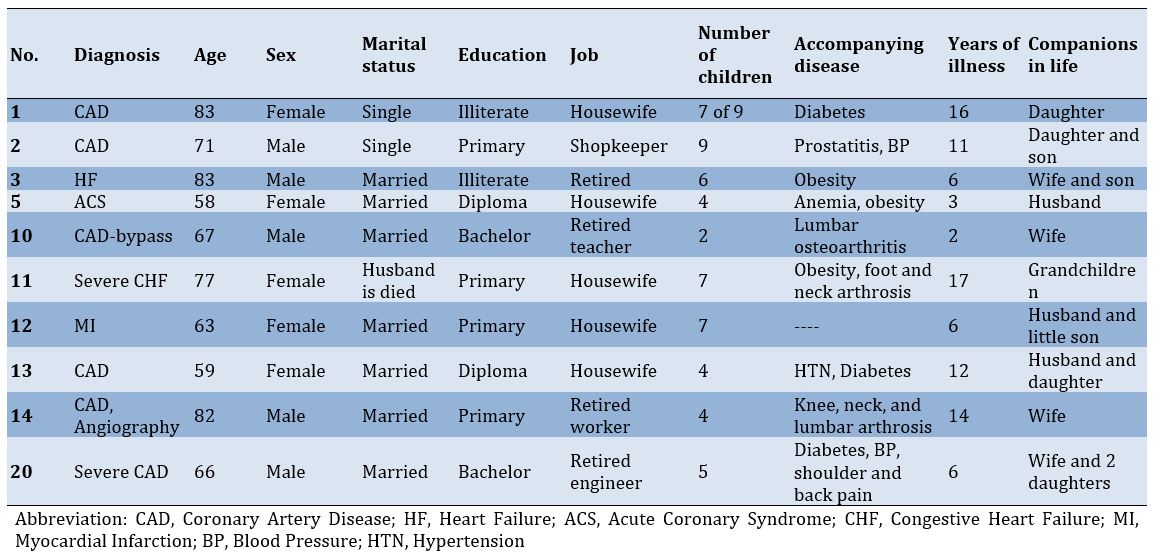
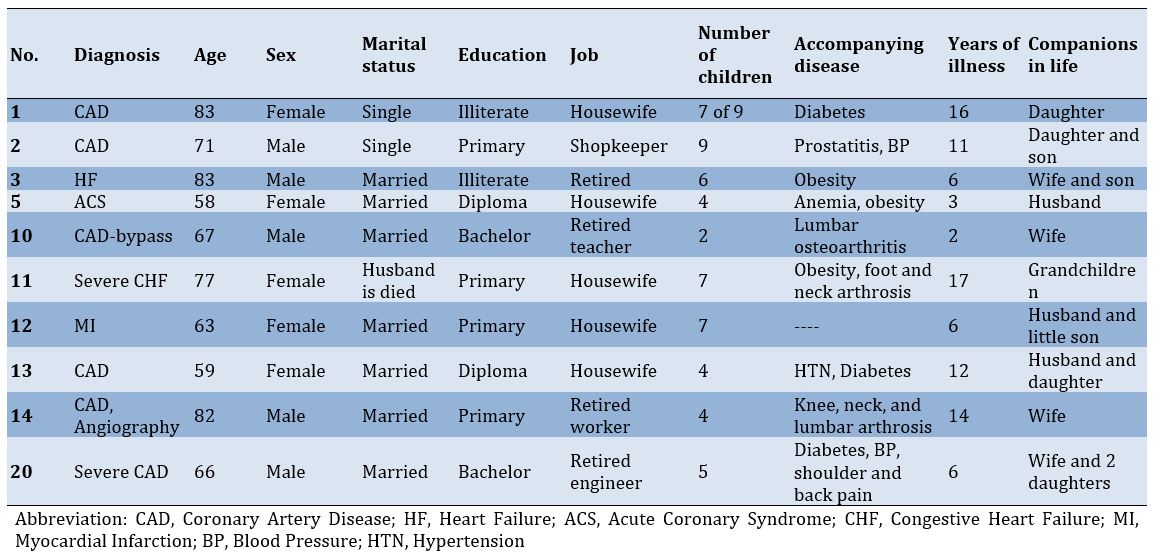
The characteristics of some participants are presented in Table 1.
Cardiovascular diseases are the leading cause of death in the world, with 17 million deaths per year [1, 2]. Studies in Iran have shown that cardiovascular diseases have the highest mortality rate compared to other diseases [3]. The first cause of death in Iran, with 39.3% of all deaths, is due to cardiovascular diseases, of which 19.5% are related to heart attack, 9.3% are due to stroke, 3.1% are related to hypertension and the rest related to other cardiovascular diseases [4]. Almost all heart diseases lead to some form of heart failure, which causes a variety of symptoms, such as shortness of breath, dizziness, angina, edema, and ascites [5, 6]. These symptoms lead to intolerance to activity [7, 8] and change the patient's lifestyle [9], which affects his satisfaction and quality of life [10-12].
Apart from poor prognosis and pain [10], these diseases cause limitations in physical activity, changes in physical condition [13], loss of job security, reduced recreational activity, fear and anxiety about the future, disruption of family roles, fear of death, and cessation of social interactions [14, 15]. Psychological distress (anxiety), decreased vitality, increased dependence, and early retirement impose a negative impact on quality of life [16-18]. Researchers have concluded that the symptoms of the disease are the most important predictors of quality of life, and with increasing severity of the disease, the quality of life decreases [15, 19, 20].
Abbasi et al. showed that the quality of life in patients with heart failure in physical, mental, psychological, social, and economic dimensions is in a better situation than most internal and external review studies, and only the average quality of life of the study sample in California was better than the present study, but the quality of life in these patients is still not in a good condition [21].
Quality of life is about people's perception of their position in life in terms of culture, value system in which they live, their goals, expectations, standards and priorities. So it is a completely subjective matter and not visible to others. And it is based on people's understanding of different aspects of life [16]. On the other hand, although professionals and service providers may be interested in changes in physical criteria to further improve their quality of life, patients are more likely to change their symptoms, physical function, and social roles [22].
Many nursing models have been designed, presented, and used over the past decades to provide targeted, coherent, and scientific nursing services, especially for chronic patients, which the quality of life in many of these theories, such as Roy, King, and Orem, indirectly are mentioned as the goal and consequence of care models. The main focus of these models is more on strategy and care interventions, but they have not said anything about improving the quality of life.
On the other hand, these theories are more adapted and inspired by concepts and knowledge of other disciplines such as sociology, psychology and management, and so on [23].
Therefore, for theorizing, instead of using the knowledge and theories of other fields or simply from the theorist's personal experiences, which is the dominant feature of nursing theories, the experiences of the main stakeholders, who are patients and their families, should be used. On the other hand, quality of life is an individual and mental phenomenon and is completely dependent on patients' perceptions and experiences, and people's efforts to improve quality of life are affected by individual, contextual, and cultural factors and conditions.
Therefore, since maximizing the quality of life is one of the main goals of treating heart patients, then in the first step, healthcare workers and researchers should obtain more information about the quality of life and the process of changing the different aspects of the quality of life of these patients and how to improve it; and in the second step, knowing the quality of life of patients with heart diseases and the factors affecting it by nurses can be a guide so that nursing diagnoses, measures, interventions, evaluation and adjustment of health education and health promotion programs during treatment and at the time of discharge, these variables should be considered.
This study aimed to explain the process of improving the quality of life of heart patients in Iran.
Participants and Methods
In this qualitative study, “the process of improving the quality of life in heart patients” was discovered using the method of grounded theory of the 2015 version of Strauss and Corbin. The participants in this study were patients with a variety of heart disorders who had a good understanding of the Persian language and were able to communicate verbally and tend to express their experiences. For creating maximum diversity of accurate knowledge of the factors involved in the process of improving the quality of life in these patients, participants were selected from different social classes, different stages of disease severity, and under different treatments for heart disease, including pacemaker, angioplasty, and open heart surgery. Sampling in the present study was first purposeful and then theoretical [24]. Sampling in qualitative research usually starts with purpose-based sampling, while with the emergence of conceptual classes during data analysis, participants are selected based on theoretical sampling to find the data in the direction of transparency and more accurate confirmation [25, 26].
The research environment was the heart and CCU wards of Shahid Rajaei Heart Hospital and Alborz Hospital (both in Karaj City), clinics, and homes. During the study, the researcher tried to determine the interview environment based on the ease of access of the participants and in a place where they were comfortable and willing to interview.
Data collection
Between October 25, 2020, and December 21, 2021, data collection was done by visiting the participants in the places mentioned. Individual interviews lasted for 25-60 min (30 min on average), and due to Coronavirus, the interviews were conducted via WhatsApp or phone call. The individual interviews were the main basis for data collection. In order to cover the most important areas of interest, the interviews began with broad-based, open questions with follow-up probes, with prompts such as, "How has this disease affected you and your life?" Continuing the interview was based on the answers to probing or exploratory questions, such as "What did you do to solve this problem?" The questions focused on how patients try to improve their quality of life and the issues, and problems and obstacles they face.
Data analysis
In the present study, Corbin and Strauss analysis method was used [27], which has steps, including open coding to identify concepts, development of concepts according to their characteristics and dimensions,
analyze data for context, process entry into analysis, and categories integration. The data was transcribed verbatim, and the analysis began after each interview. Throughout the whole process, data collection and coding were carried out simultaneously to explore, deepen, and refine questions, a process that contributed to the formation of new questions [28]. A constant comparative method was used to systematize and analyze data compare meanings and identify similarities and differences [27]. Texts were read line by line and labeled with codes based on phrases or names that were as close to the data as possible. Then, the codes were compared with each other based on similarities and differences. Once all the codes were identified and were starting to stand out, the next step of focused coding was followed to organize and group the data into temporary categories. Step by step, in line with the constant comparative method, the analyses were brought to a more abstract level that generated concepts confirmed by the properties of the data. During the whole process, memos were used to record reflections, questions, and ideas [29].
Study rigor
To increase the power and accuracy of the study, the researcher uses strategies such as maximum variation in sampling, long-term engagement with data, continuous comparative analysis, control by participants in the research, expert review, taking evidence-based note-taking, and using citations [30].
Findings
The characteristics of some participants are presented in Table 1.
Table 1) Characteristics of some participants
In the first and second stages of the analytic phase, open coding and development of concepts in terms of features and dimensions, analysis of research data led to the extraction of 4 concepts, which were presented under the headings of “inability to control daily life”, “striving for self-management”, “perceived support from spouse and children”, and “abandonment of the patient and family in the caring knowledge gap”.
Inability to control daily life
This concept implies that heart patients suffer from mental and physical limitations and disabilities following the onset of disease complications, which are accompanied by various stresses such as fear of imminent death, fear of disability, feeling of hopelessness for the future, and stress perceived by others, the feeling of physical disability, the frustration caused by lost physical strength, which is accompanied by the combination of limitations and disabilities with these stresses in patients creat a feeling of inability to control daily life. Knowing the cause of the patient's fears and anxieties and why they feel physically disabled, it is possible to eliminate the fears with timely interventions and to promote a sense of health instead of these unpleasant feelings by teaching health tips. This concept has three characteristics:
• Understanding of physical disability
The physical limitations caused by the disease have caused the patient to feel powerless and to see the disease constantly present and watching over them. One of the participants said:
“These same daily chores, in the middle of the housework, I’m short of breath, and my heart beats faster. This disease is always on me, madam, I used to get up at dawn, but now I sleep until noon. Because I cannot work.” (Participant 1)
• Inability to play role function
This concept actually shows that these patients have difficulty in performing many other tasks due to physical disability caused by the disease, in addition to personal duties, such as caring for children and spouses, as well as some of their favorite activities. One of the patients said so:
“I have been suffering from this disease for almost 3 years now. I have a headache when I eat a food because my fat is high. Suddenly I get short of breath and feel sick, I fall asleep. I always went after my wife, slept and brought her tea, peeled fruit, but now I have trouble breathing quickly because all the arteries of my heart are closed, so I go to sleep early. I'm afraid he will hate me for this work.” (Participant 5)
• Inability to meet financial needs in life
This concept includes problems that are imposed on the family following illness, which in some cases, however, cannot be compensated at all. On the other hand, we encounter families who normally do not have a problem with their low salary and live more or less, but with the outbreak of the disease, the costs of the disease are added to their expenses and create countless problems for them. One of the participants said so:
“Because I have heart disease, I could not have surgery on my prostate, and instead, I had to buy expensive drugs (ampoules of one million tomans) to solve the prostate problem, which imposed a lot of financial burden on me because I had to inject one ampule a day for a month.” (Participant 2)
Striving for self-management
This concept shows that the participants try to return their lives to normal by observing the relative food and medicine and also paying attention to some heart symptoms and preventive actions, and by their efforts, ignore the disease and the effect of the disease on physical and social life. There are four sub-concepts in this concept. These four sub-concepts include: “desire and effort to comply with medical advice”, “effort to maintain social interactions”, “individual effort to manage stress”, and “effort to gradually empower self-management”. As can be seen, the patients themselves try to improve their health with different methods, which will be much more effective if these spontaneous interventions are accompanied by specialized training from nurses and doctors.
• Desire and effort to comply with medical advice
This concept is related to how participants try to bring their lives closer to normal by following medical advice, whether in the field of food, medicine, and treatment or in terms of symptoms.
“I take my medicine really on time. I'm afraid of this disease, and I always take it on time. Even if I do not have money, I borrow and buy my medicine. Of course, my daughter is also really sensitive to my medicines. God bless her.” (Participant 5)
• Effort to maintain social interactions
To maintain social interactions, patients try to do their favorite social activities and maintain their family relationships, thus providing a normal life for themselves.
“My son-in-law is dead, and my daughter is left without a guardian with my two grandchildren. I try to be a good grandfather to my grandchildren and help them financially and spiritually. Sometimes I take sacks of rice for them. And sometimes I buy what they want for my grandchildren's birthday, like a bicycle, so that they know that I can still do something.” (Participant 20)
• Individual effort to manage stress
This concept expresses the methods that heart patients adopt to overcome and manage their stress.
“I just go for a walk. Nothing affects me as much as walking alone and talking to myself under my breath. I also try to stay away from those who make me angry because my heart is upset, and I am afraid something will happen to my heart.” (Participant 5)
• Effort to gradually empower self-management
This concept refers to the factors that cause self-care or disease control, which can either have arisen over time or the patient herself has been able to manage her disease by performing a series of activities.
“The first and second years after the illness were very difficult for me. I really needed the help of my children. But now I cook with a little salt, I walk, and it seems that I am not worried about my illness, and I know what to do."(Participant 31)
Perceived support from spouse and children
This concept indicates the types of support that the patient receives from the family and has five characteristics: “family assistance in home activities”, “psychological support”, “financial support”, “helping the patient to comply with treatment”, and “insufficient educational support”.
• Family assistance in home activities
The spouses and children of some of these participants try to manage him physically first so that by doing housework and other ancillary work instead of the patient, they actually want to calm the patient's body and rest the heart. This small organ is less stressed, and consequently, the patient experiences less pain in his chest, and to some extent, reduces the patient's feeling of helplessness.
“I cannot work. God bless my daughter. In the afternoon, when she no longer has anything to do in her house, she comes here and fills my freezer and buys everything for us. She cooks. She protects me in the face of my other children. Sometimes she gets into a fight with her brother because of me. She gives me money whenever I want. As a man, do not let me be ashamed of my wife. God bless her, very sympathetic, very conscientious. I did not know what to do if I did not have this daughter.” (Participant 10)
• Psychological support
Some members of the patient's family also try to talk to the patient to some extent affect the patient's psyche and encourage him/her to overcome the physical disabilities with his/her mental abilities. In this regard, one of the participants describes as follows:
“My daughter is very good. Whenever I'm mentally and physically weak in life, I talk to my daughter I feel light. My daughter constantly reminds me of my abilities and tells me not to think about diseases. You are better than a hundred like yourself, and I am sure you will answer this disease. You are strong.” (Participant 16)
• Financial support
Sometimes children, either from a close way or from a far way, support their parents financially or try to reduce the impact of financial disability on life and illness. One of them says so:
"Sometimes my son sends me Euros or Dollars from Germany so that I can pay for the medicine. I am away from him, my dear (sick laughter), but it would not be a joke. If he does not help, God should help me." (Participant 13)
• Helping the patient to comply with treatment
Of course, sometimes the participants' spouses and children try to reduce the physical symptoms to a great extent by preparing the medicines on time and giving them on time, as well as taking the parents to the doctor on time or cooking diet food for the patient.
“My wife is very precise. Sometimes she even fights with me to give my medicine on time. Sometimes I tell her, 'Oh, this idiot hurts my heart more than not taking medicine, but she doesn't listen to it (patient laughs).” (Participant 14)
• Insufficient educational support
It was also seen in many families that the family members did not give scientific and accurate education to their patients in any way. One of the participants was asked about the reason for this issue, and he answered as follows:
“Madam, by God, I do not know what to teach my father because I do not know anything myself. Every time I go to the hospital to see my father, they take me out of the room when the patients are examined. I am told not to disturb the doctor. And when the doctor comes out of the room, and I ask him about the disease and its treatment, he tells me to ask the nurses.” (Participant 15)
As it can be seen, the patient's companions themselves do not know anything about their parent's illness that they want to teach them. This issue creates a sense of confusion and stress in them and shows that their educational support for their sick parents is not enough.
Abandonment of the patient and family in the caring knowledge gap
This concept shows that a patient with heart disease, along with her family, is left in the community in terms of education and is not valued, and we are dealing with patients who do not know anything about their disease and are not given proper education and have been completely forgotten and abandoned in the health system in terms of education. This concept includes two sub-concepts called “patients' insufficient knowledge of the disease” and “neglect of education in the health system”.
• Patients' insufficient knowledge of the disease
This sub-concept means that patients are left alone in terms of education in the health structure of society.
Most patients said that the reason for their ignorance about their disease was the lack of proper guidance and lack of training from the doctor and medical staff.
One of the patients states the reason for the excessive visit to the doctor as follows:
“Why should I lie? I do not know much about my illness. For example, I do not know what this heart does. I just know that it is very important. That's why I just try to go to the doctor quickly. I should not go, but I say well, I have to go so what do I know (sighs). Someone who does not teach us, at least go to the doctor myself so as not to threaten me.” (Participant 11)
• Neglect of education in the health system
This characteristic indicates that the patient's family members are not taught, and the family members who play an important role in caring for their patients, especially during the recovery period, are in complete ignorance. This self-concept consists of two characteristics: "lack of knowledge about the disease" and "following the incorrect advice of others in self-care". This sub-concept indicates that patients have been abandoned in terms of education in the health structure of society.
One of the patients attributed her lack of knowledge to a lack of training by the medical staff.
“They do not value a person at all. They do not say what happened to my heart. What should I do? They have to tell people, explain about this disease, and tell the truth about our drugs. What should we do?” (Participant 3)
Discussion
This study aimed to answer the question, “What is the process of improving the quality of life of heart patients?” It should be noted that this is an interactive process in which, patients depending on the type of disability, in the context of "cardiac symptoms", face a physical disability caused by heart disease. In this process, patients with heart disease face the main concern of the "inability to control daily life". They use the strategy of "striving for self-management" to deal with it. Among them, "perceived support from spouse and children" as facilitators, "financial problems in life" and "leaving the patient and family in the care knowledge gap" as deterrents, and underlying diseases such as diabetes, osteoarthritis, and obesity, are known as interfering factors. Eventually, the actions and reactions performed lead to peace of mind and body, as well as the gradual acquisition of self-care abilities for heart patients (Figure 1).
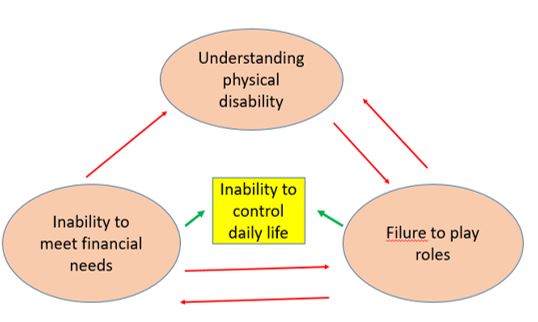
Figure1) Relationship between the three main concepts
This theory shows that the most important strategy that these patients use to respond to and resolve the stress caused by their inability to control their daily lives is to “strive for self-management”. However, factors related to the situation, background, and financial problems and the abandonment of the patient and family in the care knowledge gap act as obstacles in this direction and lead these patients to failure to play a role function, which of course strives for self-care, especially in Stress management, and obedience to medical advice have been able to bring them some peace of mind and body. To solve the problem of the inability to play a role, one should only seek appropriate treatments that are outside the scope of nursing, and financial problems are one of the problems of many patients, which is not a nursing problem. However, to provide patients with faster access to educational tips related to heart disease and to prevent the problems caused by patients' ignorance for 1 to 2 years, an educational guideline can be designed for patients, nurses, and hospitals to reduce the complications of patients' ignorance. Stress eliminates or reduces their quality of life.
A study by Malin et al. was conducted as a grounded theory in Sweden to discover discontinuities in life and the factors that contribute to the strength and continuity of heart patients in daily life [31]. One of the concepts that are almost consistent with the category of “Inability to control daily life” in our research is the concept of the experiences of discontinuity, which is completely consistent with the category of “the alienated body” and the category of “feeling of physical disability”. However, in Malin's research, time and the role of patients in time management have been mentioned, but in the present study, patients have not been mentioned in any way. In Malin's research, the subclass of “threatened self” is almost identical to the subclass of “fear of disability” and the subclass of “frustration with lost physical strength”. Malin's research does not mention the educational and financial problems of patients and their families, which may be due to socio-cultural differences or differences between the Swedish insurance system and Iran.
Another study by Fry et al. [32] was conducted in 2016 in the UK to explore the experiences of patients with heart failure. In this study, they identified 5 main themes that were of concern to patients. In the first theme, patients referred to common problems of heart failure, including physical disability and respiratory symptoms, which are in line with the understanding of the physical disability sub-category of the present study, but in Fry's study, there was no mention of frustration caused by physical disability. While in the present study, patients feel very frustrated due to the physical disability caused by the disease, which may be due to cultural differences and not having a happy life in the present study, which could be exacerbated by heart disease. The category “The role of family and friends in providing support” refers to patients 'concerns about becoming a burden for the family, and this is exactly the point that in the present study under the category of “fear of disability” and endangering patients' identities. This view is also consistent with two studies.
Two categories of "relationships with health professionals" and "access to health care" are mentioned in Fry's research, which patients did not mention at all in the present study. Perhaps one reason is that Fry has only worked on patients with heart failure, and these patients should be constantly monitored, but patients with other heart diseases in the present study do not need follow-up. Another reason may be the difference in the UK health care system, which makes access to specialists far more difficult than in Iran. In Iran, the patient can access the specialist directly and with short appointments with any symptom that she/he thinks is related to the heart, and finally, the fifth theme is the problem of "managing multiple illnesses", which has been highly emphasized by patients. In this theme, patients complain of disorders of other organs of the body along with heart problems, as well as management of drug interactions and multiple medical visits. However, in the present study, patients did not complain of comorbidities and did not consider them as important as heart disease. This difference may be due to cultural differences and patience and rapid adaptation of Iranian patients to their disease. Instead, the present study emphasizes financial and educational problems that have not been seen in Fry's research results. In Iran, contact with health professionals and caregivers is very easy, while they do not receive training from them, and in the UK, access to specialists is very difficult, but patients are educated in the same session [32].
Another qualitative study was conducted by Dhaliwal et al. in 2017 in Canada to explore the experiences of financial barriers in caring for heart patients. The study found that patients earning less than $40,000 a year did not have access to essential health care and could not afford many drugs, rehabilitation, and transportation costs and that many patients were reluctant to take their medications [33].
These results are all in line with the results of the financial dimension of the present study and may be because Canada is an immigrant country and it is not possible to allocate effective health insurance to all people.
In 2016, Malhotra et al. conducted a study in Singapore to learn about the experiences and preferences of care, communication, and decision-making among patients with heart failure. In this study, they identified six topics [34]. The theme of “physical and psychological symptoms” refers to disorders such as anxiety, depression, and withdrawal from many activities such as shopping, swimming, climbing stairs, meeting friends, or going on vacation. The class of “inability to control daily life” is one of the themes of the present study, and both are in one direction. In the “financial concerns” of Malhotra's research, patients complain about the high prices of medical care, stating that most of their medical insurance accounts have been emptied and that private insurance can only cover part of the cost of surgery, and so on. The patients continue to work even in the presence of illness and do not leave their work for treatment so that their insurance is not cut off. This theme is also in line with the subcategory of “inability to meet financial needs in life” in the present study. On the topic of “lack of knowledge about the disease” in Malhotra's research, patients also express their concern that doctors do not discuss the disease in detail with them and do not educate their families, which is exactly in line with the theme of “leaving the patient and family in the care knowledge gap” in the present study.
We showed that the process of improving the quality of life in cardiac patients is complex and is highly related to the level of literacy and education of the patients, so that the patients who had received health-related education from the hospital about their illness, performed better health care and had a better quality of life. Efforts to improve the quality of life should, in practice, consider this determining factor (health education to patients) to optimize clinical results in cardiac patients and address this important factor during the clinical interactions of nurses and doctors with patients. Health education help to improve the quality of life in these patients, and as a result, adherence to medication, diet, mobility, and exercise will improve them.
On the other hand, timely education on the tips related to the use of medicines when symptoms of the disease (chest pain and shortness of breath) can eliminate many stresses, confusion and complications caused by self-inflicted use of medicines.
Apart from the physical and mental problems, which are present in almost all the studies mentioned, it should be said that there were no signs of financial or educational problems in Sweden, but patients were still afraid of being overwhelmed and losing their identity. In the United Kingdom, Canada, and Singapore, access to a specialist was very difficult, but this problem was not seen in Iran. There are financial crises and educational abandonment of patients and families, especially in Iranian and Singaporean patients. Therefore, in the first step, a written educational program for patients and their families should be considered by specialists in order to ensure the quality and quantity of care. In the second step, financial facilities should be considered by the government to insure all sections of the population in connection with surgeries and the purchase of drugs, in order to eliminate to a large extent the predisposing and aggravating factors of physical and mental disability. When patients are aware of their illness and are comfortable with financial issues, the side stresses will go away and the main focus of patients and their families will be on the illness itself.
Strengths and weaknesses
Targeted sampling in different stages of the study ensured the diversity of the samples in terms of gender, literacy, health, and different social and economic levels and showed the factors related to improving the quality of life in these patients. The weak point is that all patients were selected from the city of Karaj, and if sampling was done from most cities in Iran, better access to different cultures would be found. It may be necessary to conduct more research on the impact of culture and geography on the process of improving the quality of life of these patients in the future.
Conclusion
Heart patients and their families in Iran are facing physical, psychological, financial and educational crises that have created other problems for them. Therefore, due to the negative interaction of heart disease and the process of care and treatment with perceived problems and experiences, this phenomenon can create a vicious cycle between the disease and the problems experienced and perceived in patients and families.
Acknowledgements: Nothing has been reported.
Ethical Permission: This study is part of a research project that was approved by the ethics board of Tarbiat Modares University of Tehran with the ethics code IR.MODARES.REC.1398.044. Permission was obtained from the hospital director and hospital staff, such as educational supervisors and nurses. Written informed consent was obtained from all of them, and they were assured that their names were protected and would not be published in any way and that they could leave the interview at any time. For illiterate’s participants informed consent was obtained from parents or guardians. All methods were carried out in accordance with relevant guidelines and regulations in the study.
Conflict of Interests: Nothing has been reported.
Authors’ Contribution: Yasarebirad M (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Mohammadkhan Kermanshahi S (Second Author), Methodologist/Assistant Researcher (30%); Mohammadi E (Third Author), Assistant Researcher/Discussion Writer (30%)
Funding: Not applicable.
In the first and second stages of the analytic phase, open coding and development of concepts in terms of features and dimensions, analysis of research data led to the extraction of 4 concepts, which were presented under the headings of “inability to control daily life”, “striving for self-management”, “perceived support from spouse and children”, and “abandonment of the patient and family in the caring knowledge gap”.
Inability to control daily life
This concept implies that heart patients suffer from mental and physical limitations and disabilities following the onset of disease complications, which are accompanied by various stresses such as fear of imminent death, fear of disability, feeling of hopelessness for the future, and stress perceived by others, the feeling of physical disability, the frustration caused by lost physical strength, which is accompanied by the combination of limitations and disabilities with these stresses in patients creat a feeling of inability to control daily life. Knowing the cause of the patient's fears and anxieties and why they feel physically disabled, it is possible to eliminate the fears with timely interventions and to promote a sense of health instead of these unpleasant feelings by teaching health tips. This concept has three characteristics:
• Understanding of physical disability
The physical limitations caused by the disease have caused the patient to feel powerless and to see the disease constantly present and watching over them. One of the participants said:
“These same daily chores, in the middle of the housework, I’m short of breath, and my heart beats faster. This disease is always on me, madam, I used to get up at dawn, but now I sleep until noon. Because I cannot work.” (Participant 1)
• Inability to play role function
This concept actually shows that these patients have difficulty in performing many other tasks due to physical disability caused by the disease, in addition to personal duties, such as caring for children and spouses, as well as some of their favorite activities. One of the patients said so:
“I have been suffering from this disease for almost 3 years now. I have a headache when I eat a food because my fat is high. Suddenly I get short of breath and feel sick, I fall asleep. I always went after my wife, slept and brought her tea, peeled fruit, but now I have trouble breathing quickly because all the arteries of my heart are closed, so I go to sleep early. I'm afraid he will hate me for this work.” (Participant 5)
• Inability to meet financial needs in life
This concept includes problems that are imposed on the family following illness, which in some cases, however, cannot be compensated at all. On the other hand, we encounter families who normally do not have a problem with their low salary and live more or less, but with the outbreak of the disease, the costs of the disease are added to their expenses and create countless problems for them. One of the participants said so:
“Because I have heart disease, I could not have surgery on my prostate, and instead, I had to buy expensive drugs (ampoules of one million tomans) to solve the prostate problem, which imposed a lot of financial burden on me because I had to inject one ampule a day for a month.” (Participant 2)
Striving for self-management
This concept shows that the participants try to return their lives to normal by observing the relative food and medicine and also paying attention to some heart symptoms and preventive actions, and by their efforts, ignore the disease and the effect of the disease on physical and social life. There are four sub-concepts in this concept. These four sub-concepts include: “desire and effort to comply with medical advice”, “effort to maintain social interactions”, “individual effort to manage stress”, and “effort to gradually empower self-management”. As can be seen, the patients themselves try to improve their health with different methods, which will be much more effective if these spontaneous interventions are accompanied by specialized training from nurses and doctors.
• Desire and effort to comply with medical advice
This concept is related to how participants try to bring their lives closer to normal by following medical advice, whether in the field of food, medicine, and treatment or in terms of symptoms.
“I take my medicine really on time. I'm afraid of this disease, and I always take it on time. Even if I do not have money, I borrow and buy my medicine. Of course, my daughter is also really sensitive to my medicines. God bless her.” (Participant 5)
• Effort to maintain social interactions
To maintain social interactions, patients try to do their favorite social activities and maintain their family relationships, thus providing a normal life for themselves.
“My son-in-law is dead, and my daughter is left without a guardian with my two grandchildren. I try to be a good grandfather to my grandchildren and help them financially and spiritually. Sometimes I take sacks of rice for them. And sometimes I buy what they want for my grandchildren's birthday, like a bicycle, so that they know that I can still do something.” (Participant 20)
• Individual effort to manage stress
This concept expresses the methods that heart patients adopt to overcome and manage their stress.
“I just go for a walk. Nothing affects me as much as walking alone and talking to myself under my breath. I also try to stay away from those who make me angry because my heart is upset, and I am afraid something will happen to my heart.” (Participant 5)
• Effort to gradually empower self-management
This concept refers to the factors that cause self-care or disease control, which can either have arisen over time or the patient herself has been able to manage her disease by performing a series of activities.
“The first and second years after the illness were very difficult for me. I really needed the help of my children. But now I cook with a little salt, I walk, and it seems that I am not worried about my illness, and I know what to do."(Participant 31)
Perceived support from spouse and children
This concept indicates the types of support that the patient receives from the family and has five characteristics: “family assistance in home activities”, “psychological support”, “financial support”, “helping the patient to comply with treatment”, and “insufficient educational support”.
• Family assistance in home activities
The spouses and children of some of these participants try to manage him physically first so that by doing housework and other ancillary work instead of the patient, they actually want to calm the patient's body and rest the heart. This small organ is less stressed, and consequently, the patient experiences less pain in his chest, and to some extent, reduces the patient's feeling of helplessness.
“I cannot work. God bless my daughter. In the afternoon, when she no longer has anything to do in her house, she comes here and fills my freezer and buys everything for us. She cooks. She protects me in the face of my other children. Sometimes she gets into a fight with her brother because of me. She gives me money whenever I want. As a man, do not let me be ashamed of my wife. God bless her, very sympathetic, very conscientious. I did not know what to do if I did not have this daughter.” (Participant 10)
• Psychological support
Some members of the patient's family also try to talk to the patient to some extent affect the patient's psyche and encourage him/her to overcome the physical disabilities with his/her mental abilities. In this regard, one of the participants describes as follows:
“My daughter is very good. Whenever I'm mentally and physically weak in life, I talk to my daughter I feel light. My daughter constantly reminds me of my abilities and tells me not to think about diseases. You are better than a hundred like yourself, and I am sure you will answer this disease. You are strong.” (Participant 16)
• Financial support
Sometimes children, either from a close way or from a far way, support their parents financially or try to reduce the impact of financial disability on life and illness. One of them says so:
"Sometimes my son sends me Euros or Dollars from Germany so that I can pay for the medicine. I am away from him, my dear (sick laughter), but it would not be a joke. If he does not help, God should help me." (Participant 13)
• Helping the patient to comply with treatment
Of course, sometimes the participants' spouses and children try to reduce the physical symptoms to a great extent by preparing the medicines on time and giving them on time, as well as taking the parents to the doctor on time or cooking diet food for the patient.
“My wife is very precise. Sometimes she even fights with me to give my medicine on time. Sometimes I tell her, 'Oh, this idiot hurts my heart more than not taking medicine, but she doesn't listen to it (patient laughs).” (Participant 14)
• Insufficient educational support
It was also seen in many families that the family members did not give scientific and accurate education to their patients in any way. One of the participants was asked about the reason for this issue, and he answered as follows:
“Madam, by God, I do not know what to teach my father because I do not know anything myself. Every time I go to the hospital to see my father, they take me out of the room when the patients are examined. I am told not to disturb the doctor. And when the doctor comes out of the room, and I ask him about the disease and its treatment, he tells me to ask the nurses.” (Participant 15)
As it can be seen, the patient's companions themselves do not know anything about their parent's illness that they want to teach them. This issue creates a sense of confusion and stress in them and shows that their educational support for their sick parents is not enough.
Abandonment of the patient and family in the caring knowledge gap
This concept shows that a patient with heart disease, along with her family, is left in the community in terms of education and is not valued, and we are dealing with patients who do not know anything about their disease and are not given proper education and have been completely forgotten and abandoned in the health system in terms of education. This concept includes two sub-concepts called “patients' insufficient knowledge of the disease” and “neglect of education in the health system”.
• Patients' insufficient knowledge of the disease
This sub-concept means that patients are left alone in terms of education in the health structure of society.
Most patients said that the reason for their ignorance about their disease was the lack of proper guidance and lack of training from the doctor and medical staff.
One of the patients states the reason for the excessive visit to the doctor as follows:
“Why should I lie? I do not know much about my illness. For example, I do not know what this heart does. I just know that it is very important. That's why I just try to go to the doctor quickly. I should not go, but I say well, I have to go so what do I know (sighs). Someone who does not teach us, at least go to the doctor myself so as not to threaten me.” (Participant 11)
• Neglect of education in the health system
This characteristic indicates that the patient's family members are not taught, and the family members who play an important role in caring for their patients, especially during the recovery period, are in complete ignorance. This self-concept consists of two characteristics: "lack of knowledge about the disease" and "following the incorrect advice of others in self-care". This sub-concept indicates that patients have been abandoned in terms of education in the health structure of society.
One of the patients attributed her lack of knowledge to a lack of training by the medical staff.
“They do not value a person at all. They do not say what happened to my heart. What should I do? They have to tell people, explain about this disease, and tell the truth about our drugs. What should we do?” (Participant 3)
Discussion
This study aimed to answer the question, “What is the process of improving the quality of life of heart patients?” It should be noted that this is an interactive process in which, patients depending on the type of disability, in the context of "cardiac symptoms", face a physical disability caused by heart disease. In this process, patients with heart disease face the main concern of the "inability to control daily life". They use the strategy of "striving for self-management" to deal with it. Among them, "perceived support from spouse and children" as facilitators, "financial problems in life" and "leaving the patient and family in the care knowledge gap" as deterrents, and underlying diseases such as diabetes, osteoarthritis, and obesity, are known as interfering factors. Eventually, the actions and reactions performed lead to peace of mind and body, as well as the gradual acquisition of self-care abilities for heart patients (Figure 1).
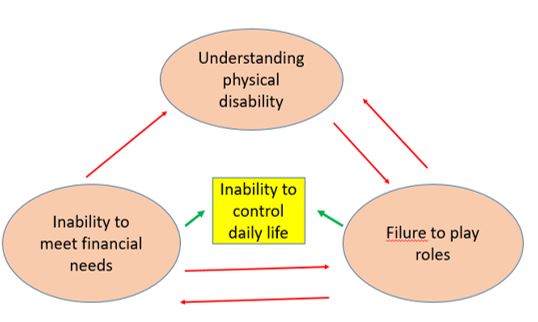
Figure1) Relationship between the three main concepts
This theory shows that the most important strategy that these patients use to respond to and resolve the stress caused by their inability to control their daily lives is to “strive for self-management”. However, factors related to the situation, background, and financial problems and the abandonment of the patient and family in the care knowledge gap act as obstacles in this direction and lead these patients to failure to play a role function, which of course strives for self-care, especially in Stress management, and obedience to medical advice have been able to bring them some peace of mind and body. To solve the problem of the inability to play a role, one should only seek appropriate treatments that are outside the scope of nursing, and financial problems are one of the problems of many patients, which is not a nursing problem. However, to provide patients with faster access to educational tips related to heart disease and to prevent the problems caused by patients' ignorance for 1 to 2 years, an educational guideline can be designed for patients, nurses, and hospitals to reduce the complications of patients' ignorance. Stress eliminates or reduces their quality of life.
A study by Malin et al. was conducted as a grounded theory in Sweden to discover discontinuities in life and the factors that contribute to the strength and continuity of heart patients in daily life [31]. One of the concepts that are almost consistent with the category of “Inability to control daily life” in our research is the concept of the experiences of discontinuity, which is completely consistent with the category of “the alienated body” and the category of “feeling of physical disability”. However, in Malin's research, time and the role of patients in time management have been mentioned, but in the present study, patients have not been mentioned in any way. In Malin's research, the subclass of “threatened self” is almost identical to the subclass of “fear of disability” and the subclass of “frustration with lost physical strength”. Malin's research does not mention the educational and financial problems of patients and their families, which may be due to socio-cultural differences or differences between the Swedish insurance system and Iran.
Another study by Fry et al. [32] was conducted in 2016 in the UK to explore the experiences of patients with heart failure. In this study, they identified 5 main themes that were of concern to patients. In the first theme, patients referred to common problems of heart failure, including physical disability and respiratory symptoms, which are in line with the understanding of the physical disability sub-category of the present study, but in Fry's study, there was no mention of frustration caused by physical disability. While in the present study, patients feel very frustrated due to the physical disability caused by the disease, which may be due to cultural differences and not having a happy life in the present study, which could be exacerbated by heart disease. The category “The role of family and friends in providing support” refers to patients 'concerns about becoming a burden for the family, and this is exactly the point that in the present study under the category of “fear of disability” and endangering patients' identities. This view is also consistent with two studies.
Two categories of "relationships with health professionals" and "access to health care" are mentioned in Fry's research, which patients did not mention at all in the present study. Perhaps one reason is that Fry has only worked on patients with heart failure, and these patients should be constantly monitored, but patients with other heart diseases in the present study do not need follow-up. Another reason may be the difference in the UK health care system, which makes access to specialists far more difficult than in Iran. In Iran, the patient can access the specialist directly and with short appointments with any symptom that she/he thinks is related to the heart, and finally, the fifth theme is the problem of "managing multiple illnesses", which has been highly emphasized by patients. In this theme, patients complain of disorders of other organs of the body along with heart problems, as well as management of drug interactions and multiple medical visits. However, in the present study, patients did not complain of comorbidities and did not consider them as important as heart disease. This difference may be due to cultural differences and patience and rapid adaptation of Iranian patients to their disease. Instead, the present study emphasizes financial and educational problems that have not been seen in Fry's research results. In Iran, contact with health professionals and caregivers is very easy, while they do not receive training from them, and in the UK, access to specialists is very difficult, but patients are educated in the same session [32].
Another qualitative study was conducted by Dhaliwal et al. in 2017 in Canada to explore the experiences of financial barriers in caring for heart patients. The study found that patients earning less than $40,000 a year did not have access to essential health care and could not afford many drugs, rehabilitation, and transportation costs and that many patients were reluctant to take their medications [33].
These results are all in line with the results of the financial dimension of the present study and may be because Canada is an immigrant country and it is not possible to allocate effective health insurance to all people.
In 2016, Malhotra et al. conducted a study in Singapore to learn about the experiences and preferences of care, communication, and decision-making among patients with heart failure. In this study, they identified six topics [34]. The theme of “physical and psychological symptoms” refers to disorders such as anxiety, depression, and withdrawal from many activities such as shopping, swimming, climbing stairs, meeting friends, or going on vacation. The class of “inability to control daily life” is one of the themes of the present study, and both are in one direction. In the “financial concerns” of Malhotra's research, patients complain about the high prices of medical care, stating that most of their medical insurance accounts have been emptied and that private insurance can only cover part of the cost of surgery, and so on. The patients continue to work even in the presence of illness and do not leave their work for treatment so that their insurance is not cut off. This theme is also in line with the subcategory of “inability to meet financial needs in life” in the present study. On the topic of “lack of knowledge about the disease” in Malhotra's research, patients also express their concern that doctors do not discuss the disease in detail with them and do not educate their families, which is exactly in line with the theme of “leaving the patient and family in the care knowledge gap” in the present study.
We showed that the process of improving the quality of life in cardiac patients is complex and is highly related to the level of literacy and education of the patients, so that the patients who had received health-related education from the hospital about their illness, performed better health care and had a better quality of life. Efforts to improve the quality of life should, in practice, consider this determining factor (health education to patients) to optimize clinical results in cardiac patients and address this important factor during the clinical interactions of nurses and doctors with patients. Health education help to improve the quality of life in these patients, and as a result, adherence to medication, diet, mobility, and exercise will improve them.
On the other hand, timely education on the tips related to the use of medicines when symptoms of the disease (chest pain and shortness of breath) can eliminate many stresses, confusion and complications caused by self-inflicted use of medicines.
Apart from the physical and mental problems, which are present in almost all the studies mentioned, it should be said that there were no signs of financial or educational problems in Sweden, but patients were still afraid of being overwhelmed and losing their identity. In the United Kingdom, Canada, and Singapore, access to a specialist was very difficult, but this problem was not seen in Iran. There are financial crises and educational abandonment of patients and families, especially in Iranian and Singaporean patients. Therefore, in the first step, a written educational program for patients and their families should be considered by specialists in order to ensure the quality and quantity of care. In the second step, financial facilities should be considered by the government to insure all sections of the population in connection with surgeries and the purchase of drugs, in order to eliminate to a large extent the predisposing and aggravating factors of physical and mental disability. When patients are aware of their illness and are comfortable with financial issues, the side stresses will go away and the main focus of patients and their families will be on the illness itself.
Strengths and weaknesses
Targeted sampling in different stages of the study ensured the diversity of the samples in terms of gender, literacy, health, and different social and economic levels and showed the factors related to improving the quality of life in these patients. The weak point is that all patients were selected from the city of Karaj, and if sampling was done from most cities in Iran, better access to different cultures would be found. It may be necessary to conduct more research on the impact of culture and geography on the process of improving the quality of life of these patients in the future.
Conclusion
Heart patients and their families in Iran are facing physical, psychological, financial and educational crises that have created other problems for them. Therefore, due to the negative interaction of heart disease and the process of care and treatment with perceived problems and experiences, this phenomenon can create a vicious cycle between the disease and the problems experienced and perceived in patients and families.
Acknowledgements: Nothing has been reported.
Ethical Permission: This study is part of a research project that was approved by the ethics board of Tarbiat Modares University of Tehran with the ethics code IR.MODARES.REC.1398.044. Permission was obtained from the hospital director and hospital staff, such as educational supervisors and nurses. Written informed consent was obtained from all of them, and they were assured that their names were protected and would not be published in any way and that they could leave the interview at any time. For illiterate’s participants informed consent was obtained from parents or guardians. All methods were carried out in accordance with relevant guidelines and regulations in the study.
Conflict of Interests: Nothing has been reported.
Authors’ Contribution: Yasarebirad M (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Mohammadkhan Kermanshahi S (Second Author), Methodologist/Assistant Researcher (30%); Mohammadi E (Third Author), Assistant Researcher/Discussion Writer (30%)
Funding: Not applicable.
Article Type: Original Research |
Subject:
Quality of Life
Received: 2022/07/12 | Accepted: 2023/02/13 | Published: 2023/02/19
Received: 2022/07/12 | Accepted: 2023/02/13 | Published: 2023/02/19
References
1. Emery CF, Frid DJ, Engebretson TO, Alonzo AA, Fish A, Ferketich AK, et al. Gender differences in quality of life among cardiac patients. Psychosom Med. 2004;66(2):190-7. [Link] [DOI:10.1097/01.psy.0000116775.98593.f4]
2. Al-Makki A, Dipette DJ, Whelton PK, Murad MH, Mustafa RA, Acharya S, et al. Hypertension pharmacological treatment in adults: a World Health Organization guideline executive summary. Hypertension. 2022;79(1):293-301. [Link] [DOI:10.1161/HYPERTENSIONAHA.121.18192]
3. Şahan E, Eroğlu MZ, Karataş MB, Mutluer B, Uğurpala,e C, Berkold TD. Death anxiety in patients with myocardial infarction or cancer. Egypt Heart J. 2018;70(3):143-7. [Link] [DOI:10.1016/j.ehj.2018.04.003]
4. Lakdizaji S, Hassankhni H, Mohajjel Agdam A, Khajegodary M, Salehi R. Effect of educational program on quality of life of patients with heart failure: a randomized clinical trial. J Caring Sci. 2013;2(1):11-8. [Link]
5. Dehghanzadeh S, Dehghan Nayeri N, Varaei S. "Doubtful accepting": A grounded theory study of living with cardiac resynchronization therapy. Nurs Health Sci. 2018;20(4):516-22. [Link] [DOI:10.1111/nhs.12547]
6. Alharbi M, Alharbi F, AlTuwayjiri A, Alharbi Y, Alhofair Y, Alanazi A, et al. Assessment of health-related quality of life in patients with heart failure: a cross-sectional study in Saudi Arabia. Health Qual Life Outcomes. 2022;20(1):128. [Link] [DOI:10.1186/s12955-022-02040-7]
7. Schjoedi I, Sommer I, Bjerrum MB. Experiences and management of fatigue in everyday life among adult patients living with heart failure: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep. 2016;14(3):68-115. [Link] [DOI:10.11124/JBISRIR-2016-2441]
8. Takabayashi K, Kitaguchi S, Iwatsu K, Morikami Y, Ichinohe T, Yamamoto T, et al. A decline in activities of daily living due to acute heart failure is an independent risk factor of hospitalization for heart failure and mortality. J Cardiol. 2019;73(6):522-9. [Link] [DOI:10.1016/j.jjcc.2018.12.014]
9. Tarekegn GE, Gezie LD, Birhan TY, Ewnetu F. Health-related quality of life among heart failure patients attending an outpatient clinic in the University of Gondar Comprehensive Specialized Hospital Northwest, Ethiopia, 2020: using structural equation modeling approach. Patient Relat Outcome Meas. 2021;12: 279-90. [Link] [DOI:10.2147/PROM.S322421]
10. Hekari D, Mohammadzadeh R. The assessment of adaptation rate of coronary artery disease female patients according to quadruple aspects of physiologic, self-perception, role playing and independence/dependence in Tabriz, 1386-87. Med Sci J. 2008;18 (3):187-93. [Persian] [Link]
11. Bahador R, Nouhi E, Jahani Y. Quality of life and its related factors in patients with CHF, referring to Jiroft Imam Khomeini Hospital. Iran J Nurs. 2017;30(105):23-33. [Persian] [Link] [DOI:10.29252/ijn.30.105.23]
12. Sun L-Y, Lee E-W, Zahra A, Park J-H. Risk factors of cardiovascular disease and their related socio-economical, environmental and health behavioral factors: Focused on low-middle income countries- a narrative review article. Iran J Public Health. 2015;44(4):435-44. [Link]
13. Komalasari R, Nurjanah, Yoche MM. Quality of life of people with cardiovascular disease: A descriptive study. Asian Pac IsI Nurse J. 2019;4(2):92-6. [Link] [DOI:10.31372/20190402.1045]
14. Moshki M, Khajavi A, Minaee S, Vakilian F, Hashemizadeh H. Perceived benefits of the disease: A qualitative study of patients' experiences of heart failure. Nurs Health Sci. 2020;22(2):464-71. [Link] [DOI:10.1111/nhs.12682]
15. Soleimani MA, Zarabadi-Pour S, Motalebi SA, Allen KA. Predictors of quality of life in patients with heart disease. J Relig Health. 2020;59(4):2135-48. [Link] [DOI:10.1007/s10943-019-00968-7]
16. Nejat S. Quality of life and its measurement. Iran J Epidemiol. 2008;4(2):57-62. [Persian] [Link]
17. Bahall M, Legall G, Khan K. Quality of life among patients with cardiac disease: the impact of comorbid depression. Health Qual Life Outcomes. 2020;18(1):189. [Link] [DOI:10.1186/s12955-020-01433-w]
18. Vlachakis C, Dragoumani K, Raftopoulou S, Mantaiou M, Papageorgiou L, Tsaniras SC, et al. In Vivo. 2018;32(4):859-70. [Link] [DOI:10.21873/invivo.11320]
19. Ferdiana A, Post MWM, King N, Bültmann U, van der Klink JJL. Meaning and components of quality of life among individuals with spinal cord injury in Yogyakarta Province, Indonesia. Disabil Rehabil. 2018;40(10):1183-91. [Link] [DOI:10.1080/09638288.2017.1294204]
20. Nwosu WO, Rajani R, McDonaugh T, Driscoll E, Hughes LD. Patients' and carers' perspective of the impact of heart failure on quality of life: a qualitative study. Psychol Health Med. 2022;27(6):1381-96. [Link] [DOI:10.1080/13548506.2021.1922719]
21. Abbasi K, Mohammadi E, Sadeghian H, Gholami Fesharaki M. Quality of life in patients with heart failure. Iran J Nurs Res. 2016;11(2):10-23. [Persian] [Link]
22. The Health Foundation. Quality improvement made simple. London: The Health Foundation; 2021. [Link]
23. Alligood MR, Tomy AM, editors. Nursing theorists and their work. 7th Edition. Maryland Heights, MO: Mosby Elsevier, 2010. [Link]
24. Noble H, Mitchell G. What is grounded theory? Evid Based Nurs. 2016;19(2):34-5. [Link] [DOI:10.1136/eb-2016-102306]
25. Haj Bagheri A, Parvizi S, Salsali M. Qualitative Reseach methods. Tehran: Boshra; 2013. [Persian] [Link]
26. Haj Bagheri A. Grounded theory: Research method. Tehran: Boshra; 2006. [Persian] [Link]
27. Juliet C, Anselm S. Basics of qualitative researches; Techniques and procedures for developing grounded theory. 4th Edition. Thousand Oaks, California: SAGE; 2015. [Link]
28. Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative content analysis: A focus on trustworthiness. SAGE J. 2014. [Link] [DOI:10.1177/2158244014522633]
29. Delve Ho L, Limpaecher A. The practical guide to grounded theory, practice guide to grounded theory research. 2021. [Link]
30. Tie YC, Birks M, Francis K. Grounded theory research: A design framework for novice researchers. SAGE Open Med. 2019;7:2050312118822927. [Link] [DOI:10.1177/2050312118822927]
31. Malin O, Ung EJ, Falk K. Continuity means "preserving a consistent whole"-A grounded theory study. Int J Qual Stud Health Wellbeing. 2015;10:29872. [Link] [DOI:10.3402/qhw.v10.29872]
32. Fry M, McLachlan S, Purdy S, Sanders T, Kadam UT, Chew-Graham CA. The implications of living with heart failure; the impact on everyday life, family support, co-morbidities and access to healthcare: a secondary qualitative analysis. BMC Fam Pract. 2016;17:139. [Link] [DOI:10.1186/s12875-016-0537-5]
33. Dhaliwal KK, King-Shier K, Manns BJ, Hemmelgarn BR, Stone JA, Campbell DJ. Exploring the impact of financial barriers on secondary prevention of heart disease. BMC Cardiovasc Disord. 2017;17(1):61. [Link] [DOI:10.1186/s12872-017-0495-4]
34. Malhotra C, Wong GCS, Tan BC, Ng CSH, Lee NC, Lau CSL, et al. Living with heart failure: Perspectives of patients from Singapore. Proceed Singapore Health Care. 2016;25(2):92-7. [Link] [DOI:10.1177/2010105815624121]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







