Volume 10, Issue 4 (2022)
Health Educ Health Promot 2022, 10(4): 735-745 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Javanmard Z, Ameri F, Norouzi Shadmehri N, Karim Nia F, Mohamadyan M, Rajabi E. Types of Electronic Health Records Designed in Iran: A Systematic Review. Health Educ Health Promot 2022; 10 (4) :735-745
URL: http://hehp.modares.ac.ir/article-5-62665-en.html
URL: http://hehp.modares.ac.ir/article-5-62665-en.html
1- Department of Health Information Management, School of Allied Medical Sciences, Tehran University of Medical Sciences, Tehran, Iran
2- “Student Research Committee” and “School of Paramedical Sciences”, Mashhad University of Medical Sciences, Mashhad, Iran
3- Department of Health Information Technology, Ferdows School of Allied Medicine and Public Health, Birjand University of Medical Sciences, Birjand, Iran
4- Department of Surgical Technology, Ferdows School of Allied Medicine and Public Health, Birjand University of Medical Sciences, Birjand, Iran
2- “Student Research Committee” and “School of Paramedical Sciences”, Mashhad University of Medical Sciences, Mashhad, Iran
3- Department of Health Information Technology, Ferdows School of Allied Medicine and Public Health, Birjand University of Medical Sciences, Birjand, Iran
4- Department of Surgical Technology, Ferdows School of Allied Medicine and Public Health, Birjand University of Medical Sciences, Birjand, Iran
Keywords: Electronic Health Records [MeSH], Electronic Medical Records [MeSH], Personal Health Records [MeSH], Iran [MeSH]
Full-Text [PDF 1341 kb]
(757 Downloads)
| Abstract (HTML) (922 Views)
Full-Text: (352 Views)
Introduction
Medical information contained in medical records is very significant so that their appropriate management can lead to the growth of medical knowledge and the development of healthcare in a country and allow managers of different levels to provide accurate, comprehensive, and timely information for decisions and policies and minimize wrong decisions [1, 2].
Patients' medical records can be stored in various forms, e.g., paper, electronic, microfilm, or a combination of several formats, depending on the policies of the healthcare institution. Due to their inherent limitations, paper records cannot properly link healthcare providers and process data into actionable information, and their timely access is physically limited to one location, one user, and one time. Furthermore, organizing data and determining their temporal precedence is sometimes difficult and time-consuming [3]. On the other hand, information technology evolution has led to the move to computer information systems since the mid-1970s. Information technology improves the quality of healthcare and leads to the development of clinical systems [4, 5]. Moreover, Byrd noted that new health information systems can improve the quality of health information because of their better design, the use of structured data elements, drop-down menus, and instantaneous and point-of-care records of patient information by service providers [6].
The ultimate objective of these systems was to digitize health records and access Electronic Health Records (EHRs).
The EHR is an extensively accessible, understandable, and lifelong tool that collects personal health information electronically and is recorded, verified, and shared by healthcare providers [7-9]. The EHR includes critical medical information for diagnosis and treatment in healthcare on health status, physician visits, hospitalization, laboratory results, radiological findings, nursing documentation, and prescription medicines. It also potentially reduces drug interactions and side effects, as well as makes the tasks easier and saves patients' time [1]. Other functions of these EHRs include the ability to process, store, preserve, and transfer information by computer and, if necessary, make the information available to authorized people [10]. The EHRs have improved the quality of service delivery, reduced errors, and allowed integrated access and display of all patient data as the primary objective of the EHR [11].
The use of EHRs is significantly widespread nowadays. According to a study, only 12.2% of US hospitals had this basic system in 2009, and this percentage increased to 75.5% by 2015 [12]. This increase in the application could be due to the impact of EHRs on improving patient care.
According to Wigeman [13], five infrastructures are required to design and implement EHR system, including (i) Automatic Medical Records, (ii) Computer Medical Records, (iii) Electronic Medical Records (EMRs), (iv) Electronic Patient Records (EPRs), and (v) Electronic Health Records (EHR). In today's healthcare settings, healthcare organizations are striving to achieve a legal Electronic Medical Record system for their physicians and staff and have provided some of the infrastructures in their organizations. The EMRs are computer information systems that collect, store, and display patient information and typically replace paper-based medical records [14]. The EMR system was implemented in November 2017 in a breast cancer service in Western Sydney, Australia. Convenient and timely access to all patient information, ensuring the accuracy of record information, and reducing bias due to the timely entry of information into the records are among the advantages of implementing an EMR system in this center. Moreover, EMR was especially appreciated by the center's staff due to its easy documentation, time savings, complete record accuracy, clinical consultations, and highlighting of cases that should be recorded [15].
Another type of EHRs that has attracted much attention is the Personal Health Record (PHR), which is a self-managed tool [16]. Promoting patient engagement in health care delivery and people's interest in accessing their EHRs make PHRs interesting. This type of record system through self-care has a significant role in improving the health and awareness of individuals and controlling symptoms [17]. The experience of the UK National Health Service in implementing a PHR system called "Health space" for diabetes management showed that this system has excellent potential to improve safety and care efficiency, and patients can check the accuracy of their summary care record and access detailed information about their health [18].
Such projects on the development of EHR and other types of electronic record systems have been implemented in many countries. Several studies have also been conducted in Iran, and record systems have been designed for different groups of patients. Some of these record systems have been designed to the level of determining the data elements of system, and some have reached the stage of creation and implementation. According to the literature, there is no comprehensive research on the types of EHR systems designed in Iran. This study aimed to review the types of these systems in Iran systematically.
Information and Methods
This study was done in 2022. We followed PRISMA guidelines to review the types of EHRs designed in Iran.
Medical information contained in medical records is very significant so that their appropriate management can lead to the growth of medical knowledge and the development of healthcare in a country and allow managers of different levels to provide accurate, comprehensive, and timely information for decisions and policies and minimize wrong decisions [1, 2].
Patients' medical records can be stored in various forms, e.g., paper, electronic, microfilm, or a combination of several formats, depending on the policies of the healthcare institution. Due to their inherent limitations, paper records cannot properly link healthcare providers and process data into actionable information, and their timely access is physically limited to one location, one user, and one time. Furthermore, organizing data and determining their temporal precedence is sometimes difficult and time-consuming [3]. On the other hand, information technology evolution has led to the move to computer information systems since the mid-1970s. Information technology improves the quality of healthcare and leads to the development of clinical systems [4, 5]. Moreover, Byrd noted that new health information systems can improve the quality of health information because of their better design, the use of structured data elements, drop-down menus, and instantaneous and point-of-care records of patient information by service providers [6].
The ultimate objective of these systems was to digitize health records and access Electronic Health Records (EHRs).
The EHR is an extensively accessible, understandable, and lifelong tool that collects personal health information electronically and is recorded, verified, and shared by healthcare providers [7-9]. The EHR includes critical medical information for diagnosis and treatment in healthcare on health status, physician visits, hospitalization, laboratory results, radiological findings, nursing documentation, and prescription medicines. It also potentially reduces drug interactions and side effects, as well as makes the tasks easier and saves patients' time [1]. Other functions of these EHRs include the ability to process, store, preserve, and transfer information by computer and, if necessary, make the information available to authorized people [10]. The EHRs have improved the quality of service delivery, reduced errors, and allowed integrated access and display of all patient data as the primary objective of the EHR [11].
The use of EHRs is significantly widespread nowadays. According to a study, only 12.2% of US hospitals had this basic system in 2009, and this percentage increased to 75.5% by 2015 [12]. This increase in the application could be due to the impact of EHRs on improving patient care.
According to Wigeman [13], five infrastructures are required to design and implement EHR system, including (i) Automatic Medical Records, (ii) Computer Medical Records, (iii) Electronic Medical Records (EMRs), (iv) Electronic Patient Records (EPRs), and (v) Electronic Health Records (EHR). In today's healthcare settings, healthcare organizations are striving to achieve a legal Electronic Medical Record system for their physicians and staff and have provided some of the infrastructures in their organizations. The EMRs are computer information systems that collect, store, and display patient information and typically replace paper-based medical records [14]. The EMR system was implemented in November 2017 in a breast cancer service in Western Sydney, Australia. Convenient and timely access to all patient information, ensuring the accuracy of record information, and reducing bias due to the timely entry of information into the records are among the advantages of implementing an EMR system in this center. Moreover, EMR was especially appreciated by the center's staff due to its easy documentation, time savings, complete record accuracy, clinical consultations, and highlighting of cases that should be recorded [15].
Another type of EHRs that has attracted much attention is the Personal Health Record (PHR), which is a self-managed tool [16]. Promoting patient engagement in health care delivery and people's interest in accessing their EHRs make PHRs interesting. This type of record system through self-care has a significant role in improving the health and awareness of individuals and controlling symptoms [17]. The experience of the UK National Health Service in implementing a PHR system called "Health space" for diabetes management showed that this system has excellent potential to improve safety and care efficiency, and patients can check the accuracy of their summary care record and access detailed information about their health [18].
Such projects on the development of EHR and other types of electronic record systems have been implemented in many countries. Several studies have also been conducted in Iran, and record systems have been designed for different groups of patients. Some of these record systems have been designed to the level of determining the data elements of system, and some have reached the stage of creation and implementation. According to the literature, there is no comprehensive research on the types of EHR systems designed in Iran. This study aimed to review the types of these systems in Iran systematically.
Information and Methods
This study was done in 2022. We followed PRISMA guidelines to review the types of EHRs designed in Iran.
Eligibility criteria
Original articles about the design or development of a type of EHR system in Iran were included in the study. All brief reports, letters to the editor, conference abstracts, observational studies, review articles, and articles with no available full text were excluded from the study process.
Information sources and search strategy
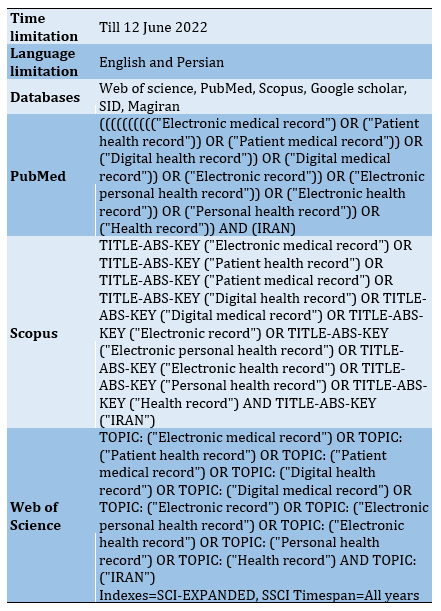
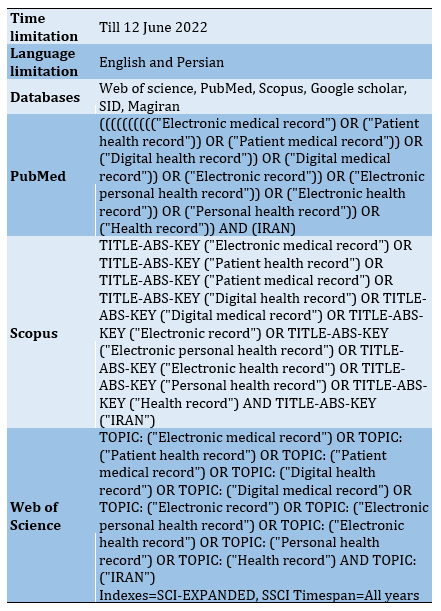
Web of Science, PubMed, and Scopus databases and Google Scholar search engine were used for retrieving English papers, as well as SID and Magiran databases were applied for retrieving Persian papers in this regard. Searching in databases was done on 12th June 2022 with no time limitation. The search strategy consisted of two concepts namely “Electronic health record” and “Iran" (Table 1), which were designed by two authors (Z.J. & F.A.). Moreover, the results were limited to English-language and Persian-language journal papers.
Study selection
The acquired articles based on the search strategy were inserted into the EndNote reference management software. At first, duplicate records were identified and removed through the software. Then the title and abstract of all studies were reviewed in terms of the eligibility criteria and if needed the full-texts were screened in detail.
The selection process was performed independently by two researchers, and if there was any contradiction discrepancy, it was referred to the third researcher.
Data extraction
Following the study selection according to the study inclusion and exclusion criteria, data were collected using a data extraction form based on the study objectives, which included the first author's name and study date, study location, study design, the aim of the study, type of electronic record, target disease or condition, Minimum Data Set (MDS), record user, and record implementation platform.
Table 1) Resource search strategy in scientific databases
Findings
A total of 715 papers were retrieved through the initial review of five databases and the Google Scholar search engine. After removing duplicate and irrelevant papers based on the evaluation of the title, abstract, and full text, finally, 28 papers were selected that were published to introduce or review the EHR system designed in Iran. A summary of the search and selection process is shown in the PRISMA diagram (Figure 1).
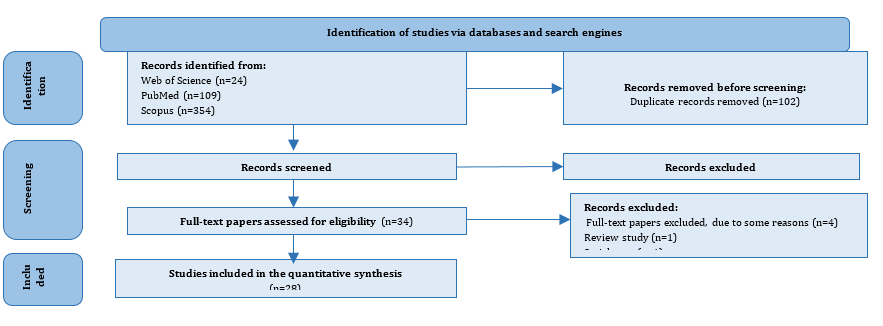
Figure 1) PRISMA flow diagram
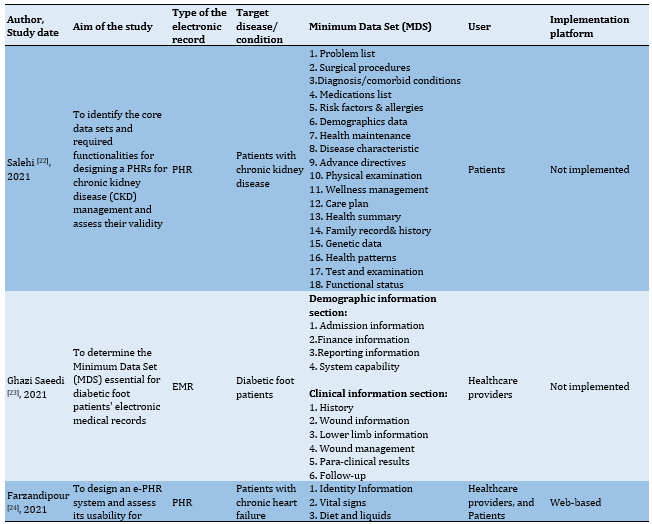
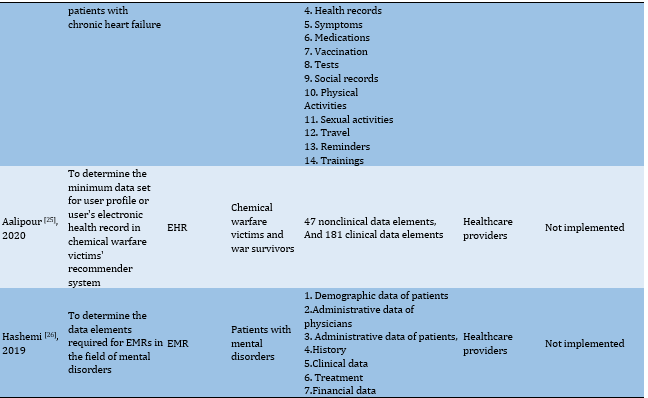
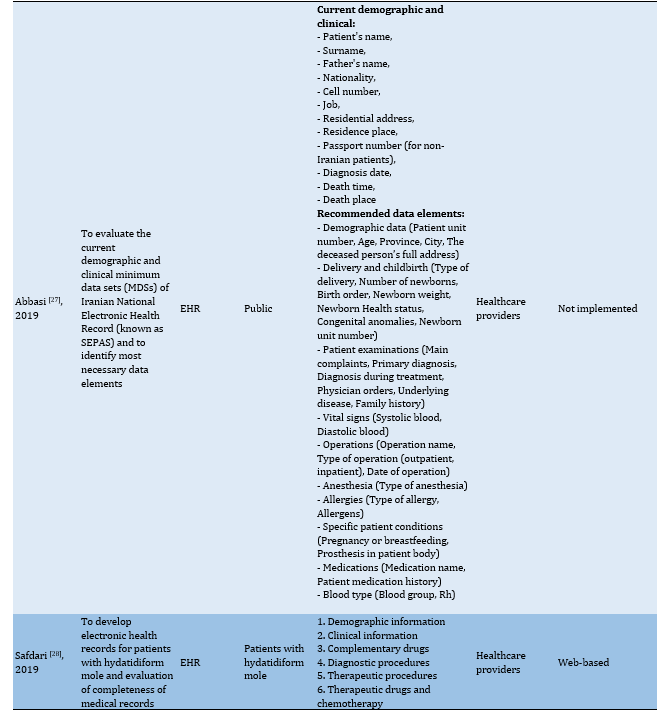
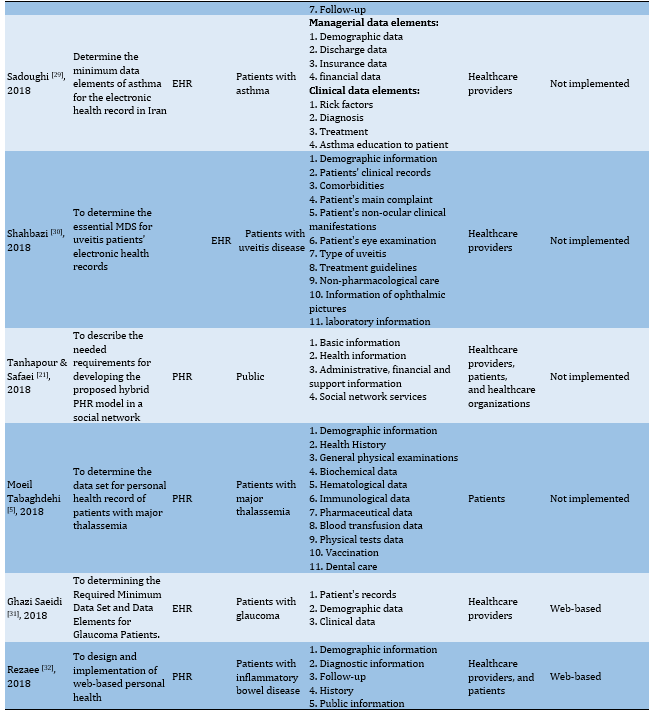
Characteristics of the studies
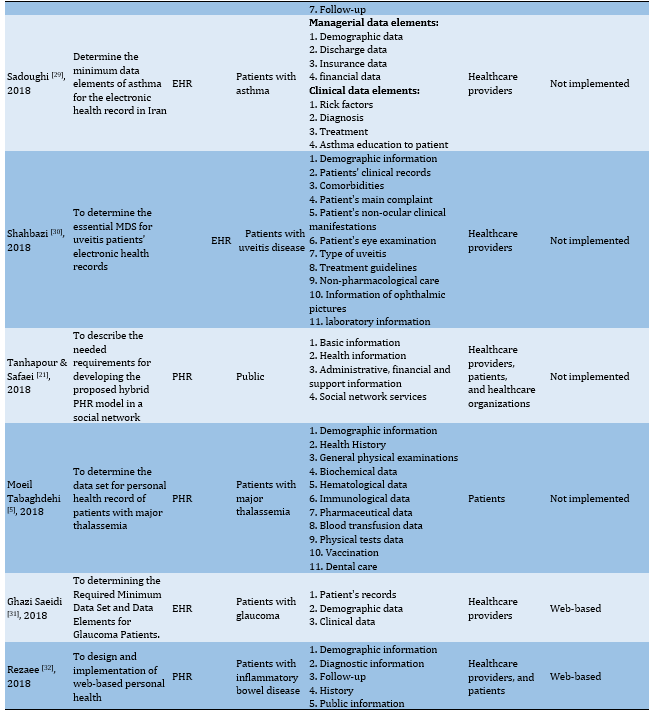
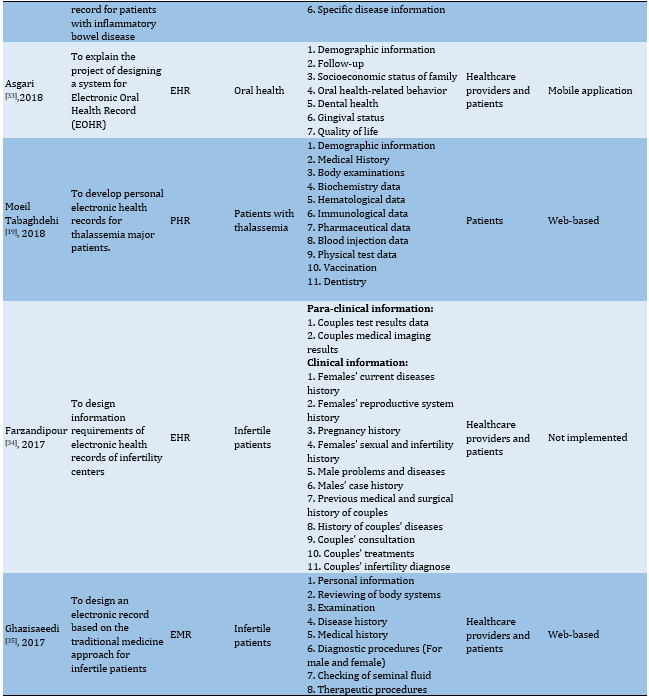
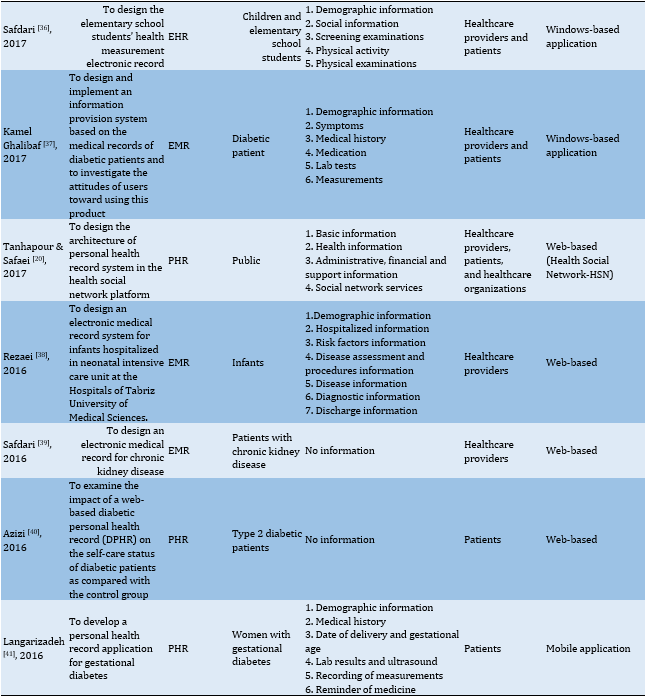
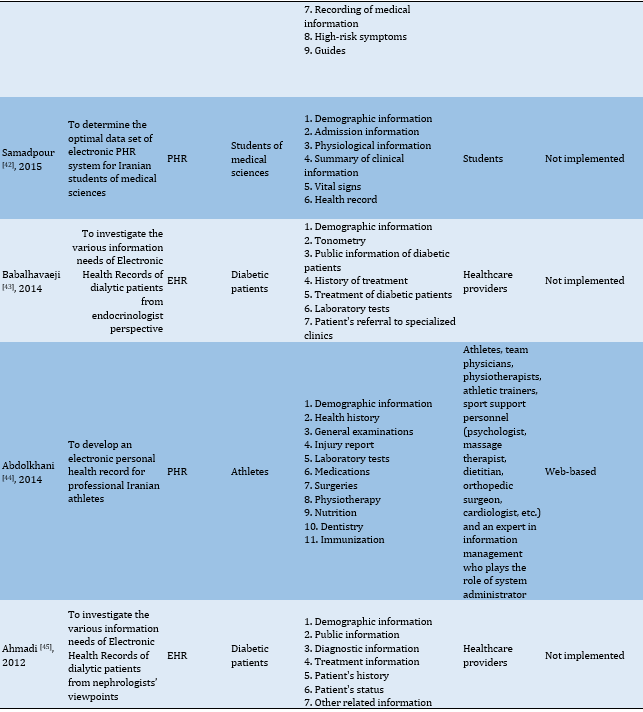
The results of 28 studies revealed that most projects on designing electronic records had been published in descriptive, descriptive-analytical, descriptive cross-sectional, and applied developmental in Iran. Approximately 46% of the studies (13 out of 28) only designed electronic record systems but did not implement them. However, some studies had implemented the designed record system after publishing their previous paper on determining the record MDS in their subsequent study. As observed in the studies conducted by Moeil Tabaghdehi et al. [5, 19], researchers published data on determining MDS of personal EHRs for patients with thalassemia major in an article in 2018. Then in the subsequent study, they developed this record system and presented the steps of its development and implementation. Similarly, in Tanhapour and Safaei's projects for designing and modeling a social health media as a PHR system, two original papers [20, 21] were published, which provided information on determining the MDS and the steps of developing and implementing electronic personal health records, respectively.
Types of electronic records
Out of 15 record systems, 4, 4, and 7 were implemented in EHR, EMR, and PHR formats, respectively. The EHR systems were implemented for infertility, uveitis, asthma, hydatidiform mole, diabetes, glaucoma, as well as school students' health information, chemical victims' health information, and national health record. In addition, EMRs were performed for mental illness, infertility, diabetes, diabetic foot ulcers data, and neonatal health information. PHRs were designed for major thalassemia, gestational diabetes, chronic kidney disease, chronic heart failure, type 2 diabetes mellitus, inflammatory bowel disease, athlete health status, student health information, and a general personal health record.
Implementation platforms
Out of 15 records, a total of 11 records (major thalassemia, hydatidiform mole, infertility, chronic kidney disease, type 2 diabetes, glaucoma, chronic heart failure, inflammatory bowel disease, athlete health status, neonatal health, and general personal health records) were developed as "web-based", two records (gestational diabetes and oral health records) were designed as "mobile application", and two records (elementary students' health records and diabetes) were performed as "windows-based application". It is noteworthy that the personal health record system designed in the study of Tanhapour and Safaei [20] was based on Web 2.0 and was developed in the social media.
Users of electronic records
The users of PHRs related to major thalassemia, gestational diabetes, type 2 diabetes, and chronic kidney disease were the "patients" with those diseases, and the users of PHRs related to students were from the "student" community. "Health care providers" were the users of records of uveitis disease, mental disorders, hydatidiform mole, infertility, diabetes, asthma, diabetic foot ulcer, chronic kidney disease, glaucoma, electronic records of infants, elementary students, chemical victims, and electronic national health records. In addition, users of diabetes, chronic heart failure, inflammatory bowel disease, athletes' health status, and oral health were "patients and health care providers"; while users of public personal health records were "patients, health care providers, and health care organizations".
Minimum data sets
Most of the data items that were considered in MDS of designed records were related to demographic data (85.71%), medical history (60.71%), therapeutic procedures (32.14%), diagnostic procedures (32.14%), and laboratory tests (32.14%), in respective order.
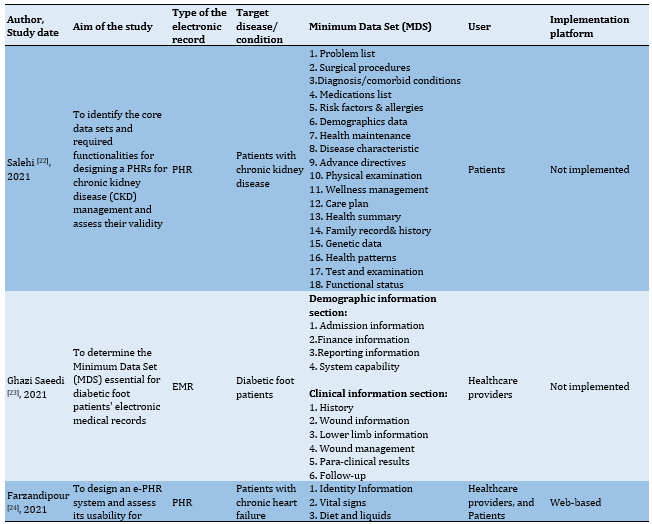
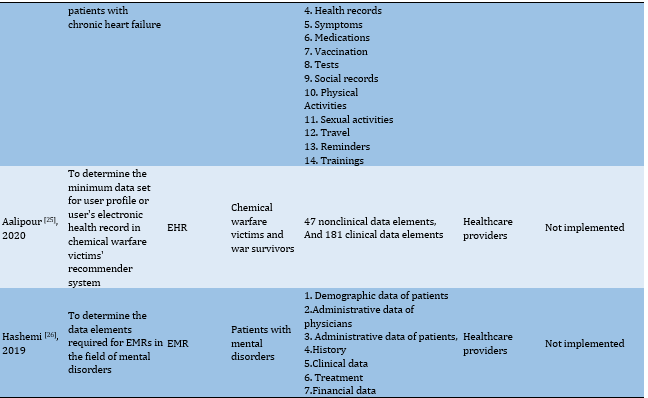
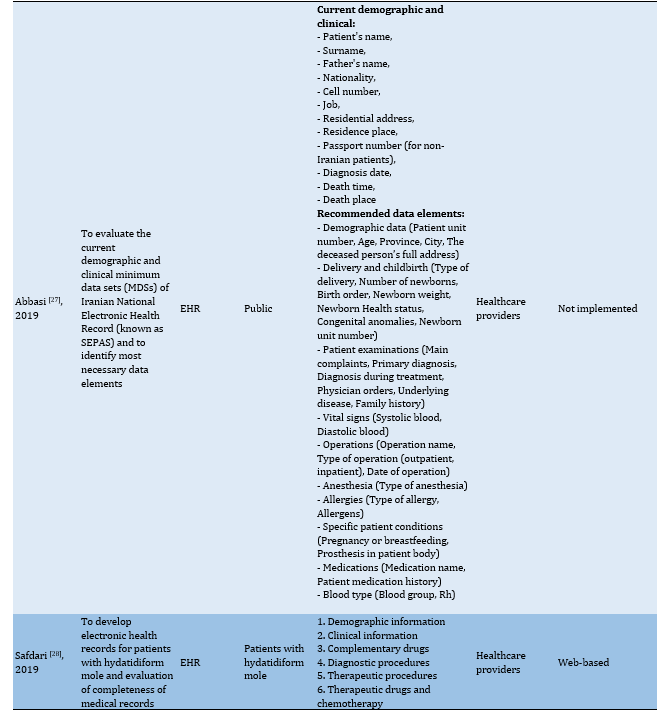
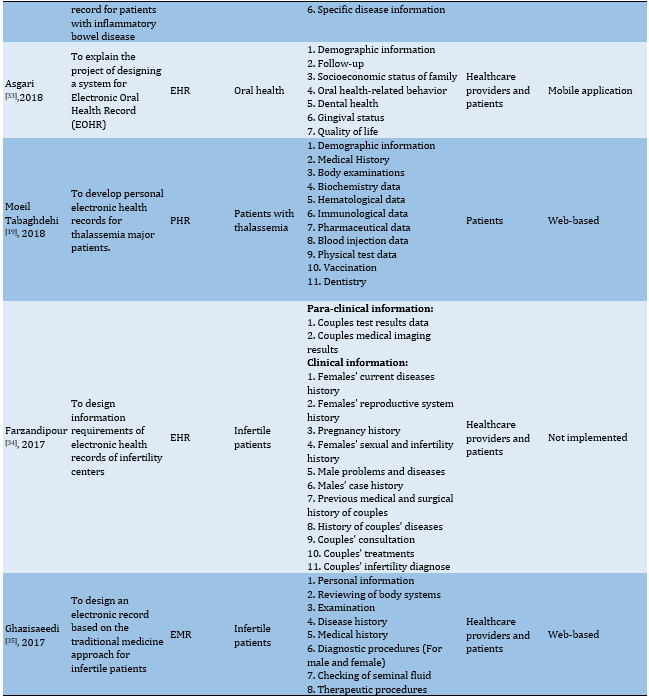
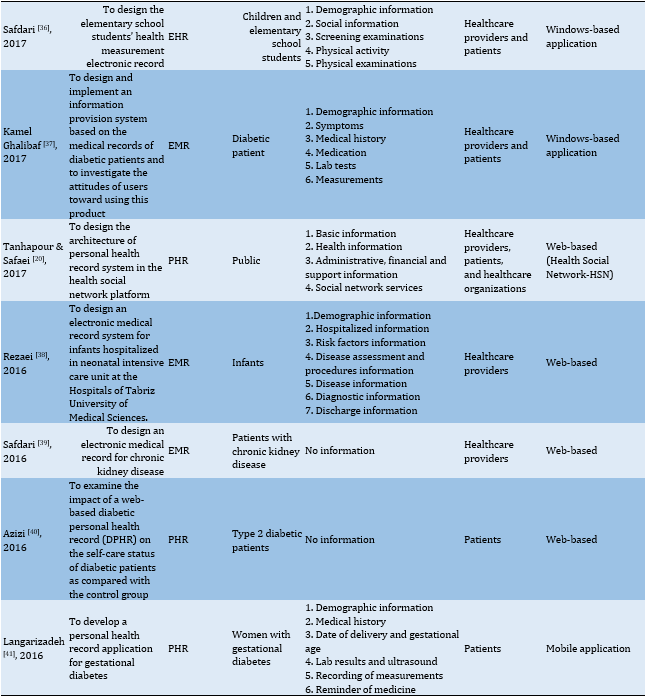
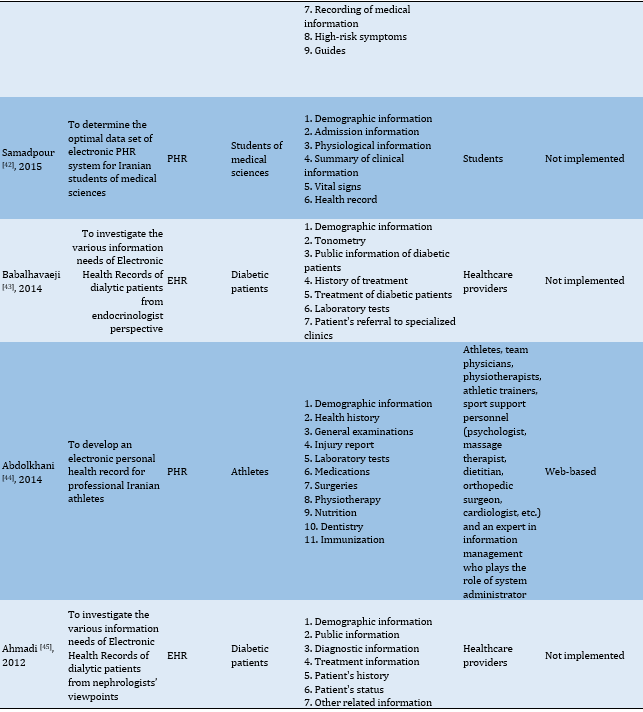
More detailed information on the types of EHRs designed in Iran is provided in Table 2.
Original articles about the design or development of a type of EHR system in Iran were included in the study. All brief reports, letters to the editor, conference abstracts, observational studies, review articles, and articles with no available full text were excluded from the study process.
Information sources and search strategy
Web of Science, PubMed, and Scopus databases and Google Scholar search engine were used for retrieving English papers, as well as SID and Magiran databases were applied for retrieving Persian papers in this regard. Searching in databases was done on 12th June 2022 with no time limitation. The search strategy consisted of two concepts namely “Electronic health record” and “Iran" (Table 1), which were designed by two authors (Z.J. & F.A.). Moreover, the results were limited to English-language and Persian-language journal papers.
Study selection
The acquired articles based on the search strategy were inserted into the EndNote reference management software. At first, duplicate records were identified and removed through the software. Then the title and abstract of all studies were reviewed in terms of the eligibility criteria and if needed the full-texts were screened in detail.
The selection process was performed independently by two researchers, and if there was any contradiction discrepancy, it was referred to the third researcher.
Data extraction
Following the study selection according to the study inclusion and exclusion criteria, data were collected using a data extraction form based on the study objectives, which included the first author's name and study date, study location, study design, the aim of the study, type of electronic record, target disease or condition, Minimum Data Set (MDS), record user, and record implementation platform.
Table 1) Resource search strategy in scientific databases
Findings
A total of 715 papers were retrieved through the initial review of five databases and the Google Scholar search engine. After removing duplicate and irrelevant papers based on the evaluation of the title, abstract, and full text, finally, 28 papers were selected that were published to introduce or review the EHR system designed in Iran. A summary of the search and selection process is shown in the PRISMA diagram (Figure 1).
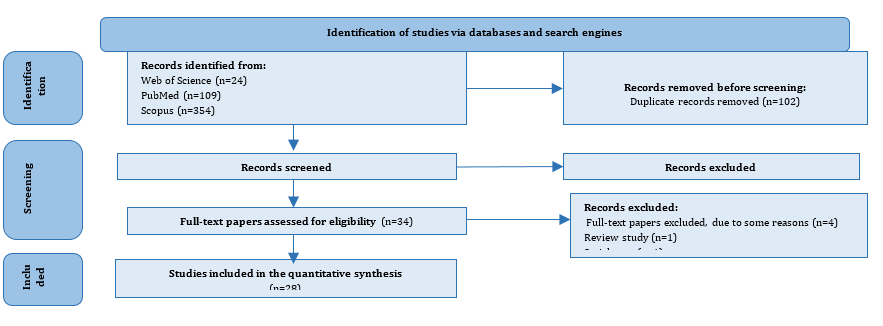
Figure 1) PRISMA flow diagram
Characteristics of the studies
The results of 28 studies revealed that most projects on designing electronic records had been published in descriptive, descriptive-analytical, descriptive cross-sectional, and applied developmental in Iran. Approximately 46% of the studies (13 out of 28) only designed electronic record systems but did not implement them. However, some studies had implemented the designed record system after publishing their previous paper on determining the record MDS in their subsequent study. As observed in the studies conducted by Moeil Tabaghdehi et al. [5, 19], researchers published data on determining MDS of personal EHRs for patients with thalassemia major in an article in 2018. Then in the subsequent study, they developed this record system and presented the steps of its development and implementation. Similarly, in Tanhapour and Safaei's projects for designing and modeling a social health media as a PHR system, two original papers [20, 21] were published, which provided information on determining the MDS and the steps of developing and implementing electronic personal health records, respectively.
Types of electronic records
Out of 15 record systems, 4, 4, and 7 were implemented in EHR, EMR, and PHR formats, respectively. The EHR systems were implemented for infertility, uveitis, asthma, hydatidiform mole, diabetes, glaucoma, as well as school students' health information, chemical victims' health information, and national health record. In addition, EMRs were performed for mental illness, infertility, diabetes, diabetic foot ulcers data, and neonatal health information. PHRs were designed for major thalassemia, gestational diabetes, chronic kidney disease, chronic heart failure, type 2 diabetes mellitus, inflammatory bowel disease, athlete health status, student health information, and a general personal health record.
Implementation platforms
Out of 15 records, a total of 11 records (major thalassemia, hydatidiform mole, infertility, chronic kidney disease, type 2 diabetes, glaucoma, chronic heart failure, inflammatory bowel disease, athlete health status, neonatal health, and general personal health records) were developed as "web-based", two records (gestational diabetes and oral health records) were designed as "mobile application", and two records (elementary students' health records and diabetes) were performed as "windows-based application". It is noteworthy that the personal health record system designed in the study of Tanhapour and Safaei [20] was based on Web 2.0 and was developed in the social media.
Users of electronic records
The users of PHRs related to major thalassemia, gestational diabetes, type 2 diabetes, and chronic kidney disease were the "patients" with those diseases, and the users of PHRs related to students were from the "student" community. "Health care providers" were the users of records of uveitis disease, mental disorders, hydatidiform mole, infertility, diabetes, asthma, diabetic foot ulcer, chronic kidney disease, glaucoma, electronic records of infants, elementary students, chemical victims, and electronic national health records. In addition, users of diabetes, chronic heart failure, inflammatory bowel disease, athletes' health status, and oral health were "patients and health care providers"; while users of public personal health records were "patients, health care providers, and health care organizations".
Minimum data sets
Most of the data items that were considered in MDS of designed records were related to demographic data (85.71%), medical history (60.71%), therapeutic procedures (32.14%), diagnostic procedures (32.14%), and laboratory tests (32.14%), in respective order.
More detailed information on the types of EHRs designed in Iran is provided in Table 2.
Table 2) Characteristics of the included studies
Discussion
This study aimed to investigate electronic record systems designed in Iran, and the papers related to designed electronic record systems were reviewed systematically. Some of the designed record systems have only reached the stage of determining the information elements of the record systems and design of the overall structure of the record systems, while others have reached the stage of their implementation. According to the literature results, the designed electronic records were in multiple levels of PHR, EMR, and EHR. In Afrizal et al.'s study [46] on the barriers to preparing EHRs in primary healthcare, these three types of records were referred to as electronic records used in primary care. Each of these record systems has its structure and application, so it is justifiable that in several studies, a specific type is developed for any purpose of electronic record design. In studies whose main purpose is to design a record that the patients can record and manage their health information, such as the investigations conducted by Moeil Tabaghdehi et al. [19] and Langarizadeh et al. [41], the record is of the type "PHR".
According to the literature, approximately 39% of studies (11 out of 28) only designed electronic record systems and did not implement them, which can be due to the lack of required infrastructure to implement these projects in Iran. Jahanbakhsh et al. [47] investigated the challenges of implementing EHR in Iran. They addressed infrastructure challenges (e.g., implementation costs, non-acceptance of EHR by many users, and lack of expertise for system maintenance) and structural challenges (e.g., the lack of an appropriate format for data entry, the shortage of data retrieval and editing services, and not enough attention to data integrity from birth to death), all of which can be true for designed records in studies.
It is noteworthy that among references in the present study, 7 out of 15 implemented records are in PHR format, and their users are patients and community members, which shows that the PHR system is more straightforward to implement than other types of electronic record systems. Moreover, it has a higher level of acceptance among its specific users. According to a study conducted by Mansour [48] in 2018 to evaluate patients' perspectives on the application of the PHR system in Egypt, PHR users showed a great desire to apply it and reported its usefulness and usability as the most important factors influencing their willingness to use this type of health record system. On the other hand, the growth of the importance of patient engagement in their care process is another reason for the widespread attention to the development of personal electronic records [49].
Another important issue related to the designed and implemented records in this study is the record implementation platform. Among 15 implemented records, 11, 2, and 2 were Web-based, in the form of mobile applications and Windows-based applications, respectively, which can be a big challenge when integrating electronic records. Heart et al. [50] also mentioned this in their study and considered the implementation of electronic records on different platforms as an important technological challenge in the integration and interoperability between records. According to the researchers, the content of the records may differ for data models, schemas, contracts, and the detail levels used to display similar data, which can make it challenging to integrate the types of records [50]. Therefore, these challenges must be considered by managers and developers to develop a comprehensive and integrated EHR.
The study of the Minimum Data Set (MDS) of designed electronic records is the next important issue addressed in this research. According to Sadoughi et al. [51], determinng the MDS is one of the most important steps in developing electronic health systems. The EHRs are no exception to this issue, and the determination of the MDS for the record systems in the types of EHRs of the studies was considered one of the important design steps. The study of these elements indicated that most of the data items considered in the types of designed records were related to demographic data, medical history, therapeutic procedures, diagnostic procedures, and laboratory tests. This result is consistent with the results of important information elements confirmed in the studies of Mahmoudvand et al. [52], Weintraub et al. [53], and Abbasi et al. [54]. The generality of these elements and their high importance are the reasons for the presence of these elements in any type of medical record. However, specific information elements of health status are also considered in every electronic record, depending on the type of disease or situation in which the electronic record was designed or developed.
Inaccessibility to the full text of some papers was one of the limitations of this study. In addition, in line with the study objective, only electronic records designed in Iran were reviewed; therefore, it is recommended that studies be conducted on the records designed and developed in other countries to achieve more accurate results on the electronic health records.
Conclusion
Designing EHRs for various diseases and clinical conditions can be an effective step towards developing a national EHR. For this purpose, determining the stakeholders' information requirements is of great importance. The results of this study can be considered as a comprehensive basis for developing a national EHR in Iran. A basis can be provided to develop a complete record taking into account the most important health factors related to the health of people in the community by considering the fundamental information elements of the types of records designed (e.g., demographic data, medical history, therapeutic procedures, diagnostic procedures, and laboratory tests), and the specific information elements of records. Furthermore, the results of this study can assist system administrators and developers in selecting an appropriate and integrated platform for developing national EHRs. Researchers can also use the results of the present study as a guideline and roadmap to compare data elements and features of EHRs designed or developed in Iran and think of solutions to solve the weaknesses of record systems with information deficiencies.
Acknowledgements: Nothing to report.
Ethical Permission: Nothing to report.
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Javanmard Z. (First author), Methodologist/ Original researcher/ Discussion author (30%); Ameri F (Second author), Methodologist/ Statistical analyst (25%); Norouzi Shadmehri N. (Third author), Introduction author/ Assistant (15%); Karim Nia F. (Fourth author), Methodologist/ Assistant (10%); Mohamadyan M. (Fifth author), Methodologist/ Assistant (10%); Erfan Rajabi E. (Sixth author), Methodologist/ Assistant (10%)
Funding: Nothing to report.
Discussion
This study aimed to investigate electronic record systems designed in Iran, and the papers related to designed electronic record systems were reviewed systematically. Some of the designed record systems have only reached the stage of determining the information elements of the record systems and design of the overall structure of the record systems, while others have reached the stage of their implementation. According to the literature results, the designed electronic records were in multiple levels of PHR, EMR, and EHR. In Afrizal et al.'s study [46] on the barriers to preparing EHRs in primary healthcare, these three types of records were referred to as electronic records used in primary care. Each of these record systems has its structure and application, so it is justifiable that in several studies, a specific type is developed for any purpose of electronic record design. In studies whose main purpose is to design a record that the patients can record and manage their health information, such as the investigations conducted by Moeil Tabaghdehi et al. [19] and Langarizadeh et al. [41], the record is of the type "PHR".
According to the literature, approximately 39% of studies (11 out of 28) only designed electronic record systems and did not implement them, which can be due to the lack of required infrastructure to implement these projects in Iran. Jahanbakhsh et al. [47] investigated the challenges of implementing EHR in Iran. They addressed infrastructure challenges (e.g., implementation costs, non-acceptance of EHR by many users, and lack of expertise for system maintenance) and structural challenges (e.g., the lack of an appropriate format for data entry, the shortage of data retrieval and editing services, and not enough attention to data integrity from birth to death), all of which can be true for designed records in studies.
It is noteworthy that among references in the present study, 7 out of 15 implemented records are in PHR format, and their users are patients and community members, which shows that the PHR system is more straightforward to implement than other types of electronic record systems. Moreover, it has a higher level of acceptance among its specific users. According to a study conducted by Mansour [48] in 2018 to evaluate patients' perspectives on the application of the PHR system in Egypt, PHR users showed a great desire to apply it and reported its usefulness and usability as the most important factors influencing their willingness to use this type of health record system. On the other hand, the growth of the importance of patient engagement in their care process is another reason for the widespread attention to the development of personal electronic records [49].
Another important issue related to the designed and implemented records in this study is the record implementation platform. Among 15 implemented records, 11, 2, and 2 were Web-based, in the form of mobile applications and Windows-based applications, respectively, which can be a big challenge when integrating electronic records. Heart et al. [50] also mentioned this in their study and considered the implementation of electronic records on different platforms as an important technological challenge in the integration and interoperability between records. According to the researchers, the content of the records may differ for data models, schemas, contracts, and the detail levels used to display similar data, which can make it challenging to integrate the types of records [50]. Therefore, these challenges must be considered by managers and developers to develop a comprehensive and integrated EHR.
The study of the Minimum Data Set (MDS) of designed electronic records is the next important issue addressed in this research. According to Sadoughi et al. [51], determinng the MDS is one of the most important steps in developing electronic health systems. The EHRs are no exception to this issue, and the determination of the MDS for the record systems in the types of EHRs of the studies was considered one of the important design steps. The study of these elements indicated that most of the data items considered in the types of designed records were related to demographic data, medical history, therapeutic procedures, diagnostic procedures, and laboratory tests. This result is consistent with the results of important information elements confirmed in the studies of Mahmoudvand et al. [52], Weintraub et al. [53], and Abbasi et al. [54]. The generality of these elements and their high importance are the reasons for the presence of these elements in any type of medical record. However, specific information elements of health status are also considered in every electronic record, depending on the type of disease or situation in which the electronic record was designed or developed.
Inaccessibility to the full text of some papers was one of the limitations of this study. In addition, in line with the study objective, only electronic records designed in Iran were reviewed; therefore, it is recommended that studies be conducted on the records designed and developed in other countries to achieve more accurate results on the electronic health records.
Conclusion
Designing EHRs for various diseases and clinical conditions can be an effective step towards developing a national EHR. For this purpose, determining the stakeholders' information requirements is of great importance. The results of this study can be considered as a comprehensive basis for developing a national EHR in Iran. A basis can be provided to develop a complete record taking into account the most important health factors related to the health of people in the community by considering the fundamental information elements of the types of records designed (e.g., demographic data, medical history, therapeutic procedures, diagnostic procedures, and laboratory tests), and the specific information elements of records. Furthermore, the results of this study can assist system administrators and developers in selecting an appropriate and integrated platform for developing national EHRs. Researchers can also use the results of the present study as a guideline and roadmap to compare data elements and features of EHRs designed or developed in Iran and think of solutions to solve the weaknesses of record systems with information deficiencies.
Acknowledgements: Nothing to report.
Ethical Permission: Nothing to report.
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Javanmard Z. (First author), Methodologist/ Original researcher/ Discussion author (30%); Ameri F (Second author), Methodologist/ Statistical analyst (25%); Norouzi Shadmehri N. (Third author), Introduction author/ Assistant (15%); Karim Nia F. (Fourth author), Methodologist/ Assistant (10%); Mohamadyan M. (Fifth author), Methodologist/ Assistant (10%); Erfan Rajabi E. (Sixth author), Methodologist/ Assistant (10%)
Funding: Nothing to report.
Article Type: Systematic Review |
Subject:
Health Communication
Received: 2022/07/20 | Accepted: 2022/10/20 | Published: 2022/11/22
Received: 2022/07/20 | Accepted: 2022/10/20 | Published: 2022/11/22
References
1. Ajami S, Ketabi S. Medical records departments and multi-criteria decision-making. Health Inf Manag. 2013;9(5):697-711. [Persian] [Link]
2. Ammenwerth E, Brender J, Nykänen P, Prokosch H-U, Rigby M, Talmon J. Visions and strategies to improve evaluation of health information systems: Reflections and lessons based on the HIS-EVAL workshop in Innsbruck. Int J Med Inform. 2004;73(6):479-91. [Link] [DOI:10.1016/j.ijmedinf.2004.04.004]
3. Mirani N, Ayatollahi H, Haghani H. A survey on barriers to the development and adoption of electronic health records in Iran. J Health Administration. 2013;15(50):65-75. [Persian] [Link]
4. Columbus ML. The evaluation and effectiveness of an interdisciplinary course in Electronic Health Record (EHR) technology for health and rehabilitation professionals [Dissertation]. Pittsburgh, Pennsylvania: University of Pittsburgh; 2006. [Link]
5. Moeil Tabaghdehi K, Ghazisaeedi M, Shahmoradi L, Karami H, Bashiri A. Designing a minimum data set for major thalassemia patients: Towards electronic personal health record. J Community Health Res. 2018;7(1):24-31. [Link]
6. Byrd JB, Vigen R, Plomondon ME, Rumsfeld JS, Box TL, Fihn SD, et al. Data quality of an electronic health record tool to support VA cardiac catheterization laboratory quality improvement: the VA Clinical Assessment, Reporting, and Tracking System for Cath Labs (CART) program. Am Heart J. 2013;165(3):434-40. [Link] [DOI:10.1016/j.ahj.2012.12.009]
7. Logue MD, Effken JA. An exploratory study of the personal health records adoption model in the older adult with chronic illness. J Innov Health Inform. 2013;20(3):151-69. [Link] [DOI:10.14236/jhi.v20i3.21]
8. Ahmadi M, Samadbeik M, Sadoughi F. Modeling of outpatient prescribing process in iran: a gateway toward electronic prescribing system. Iran J Pharm Res. 2014;13(2):725-38. [Link]
9. Rezaeibagha F, Win KT, Susilo W. A systematic literature review on security and privacy of electronic health record systems: Technical perspectives. Health Inf Manag J. 2015;44(3):23-38. [Link] [DOI:10.1177/183335831504400304]
10. Langarizadeh M, Gholinezhad KM. Designing a conceptual model of laboratory reporting system for data exchanging with Iranian electronic health record system abstract. J Health Admin. 2017;20(68):10-22. [Persian] [Link]
11. Liu Z, Han B, Jiang R, Huang Y, Ma C, Wen J, et al. Mental health status of doctors and nurses during COVID-19 epidemic in china. Lancet. 2020;4(3):1-25. [Link] [DOI:10.2139/ssrn.3551329]
12. Nguyen CT. Examination of cloud privacy & security regulations of electronic health records [Dissertation]. Utica, New York: Utica College; 2021. [Link]
13. Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: A review. Behav Sci (Basel). 2018;8(11):98. [Link] [DOI:10.3390/bs8110098]
14. Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res. 2010;10:231. [Link] [DOI:10.1186/1472-6963-10-231]
15. Janssen A, Donnelly C, Elder E, Pathmanathan N, Shaw T. Electronic medical record implementation in tertiary care: factors influencing adoption of an electronic medical record in a cancer centre. BMC Health Serv Res. 2021;21(1):23. [Link] [DOI:10.1186/s12913-020-06015-6]
16. Kupchunas WR. Personal health record: New opportunity for patient education. Orthop Nurs. 2007;26(3):185-91. [Link] [DOI:10.1097/01.NOR.0000276971.86937.c4]
17. Toni E, Pirnejad H, Niazkhani Z. The content and structure of electronic personal health records: A systematic review. J Health Biomed Inform. 2020;7(1):73-90. [Persian] [Link]
18. Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. BMJ. 2010;341:c5814. [Link] [DOI:10.1136/bmj.c5814]
19. Moeil Tabaghdehi K, Ghazisaeedi M, Shahmoradi L, Karami H. Designing and creating personal electronic health records for thalassemia major patients. J Payavard Salamat. 2018;11(5):567-77. [Persian] [Link]
20. Tanhapour M, Safaei AA. Designing and modeling personal health record systems based on health social network. J Health Biomed Inform. 2017;4(3):168-80. [Persian] [Link]
21. Tanhapour M, Safaei AA. Requirements specification of creating a hybrid model of phr based on social networking. J Payavard Salamat. 2018;11(6):618-31. [Persian] [Link]
22. Salehi F, Bastani P, Ahmadian L, Samadi K, Yazdani A, Sharifian R. Prerequisites of personal health record for chronic kidney disease: A scoping review and evaluation of the content validity. Stud Health Technol Inform. 2021;285:179-84. [Link] [DOI:10.3233/SHTI210594]
23. Saeedi MG, Javid GE, Mohammadzadeh N, Vali HAK. Determining the minimum data set of diabetic foot ulcer patients' electronic medical records. J Payavard Salamat. 2021;14(5):443-53. [Persian] [Link]
24. Farzandipour M, Nabovati E, Farrokhian A, Akbari H, Rezaei hasanvand F, Sharif R. Designing and usability assessing an electronic personal health record for patients with chronic heart failure in a developing country. Inform Med Unlocked. 2021;27:100804. [Link] [DOI:10.1016/j.imu.2021.100804]
25. Aalipour E, Ghazisaeedi M, Sedighi Moghadam MR, Shahmoradi L, Mousavi B, Beigy H. A minimum data set of user profile or electronic health record for chemical warfare victims' recommender system. J Family Med Prim Care. 2020;9(6):2995-3004. [Link] [DOI:10.4103/jfmpc.jfmpc_261_20]
26. Hashemi N, Sheikhtaheri A, Hashemi NS, Rawassizadeh R. Electronic medical records for mental disorders: what data elements should these systems contain? Stud Health Technol Inform. 2019;260:25-32. [Link]
27. Abbasi R, Khajouei R, Mirzaee M. Evaluating the demographic and clinical minimum data sets of Iranian National Electronic Health Record. BMC Health Serv Res. 2019;19(1):450. [Link] [DOI:10.1186/s12913-019-4284-x]
28. Safdari R, Mahdavi S, Shahmoradi L, Adabi K, Tahmasebian S, Nazari M. Designing and development of electronic health records for patients with hydatidiform mole and evaluation of completeness of medical records. J Payavard Salamat. 2019;12(5):359-66. [Persian] [Link]
29. Sadoughi F, Yazdanian A, Hamedan F. Provision of the minimum dataset of asthma for electronic health record. J Family Med Prim Care. 2018;7(6):1309-13. [Link] [DOI:10.4103/jfmpc.jfmpc_46_18]
30. Shahbazi M, Safdari R, Zarei M. Determining the minimum data set for uveitis patient's electronic health records in Iran. J Payavard Salamat. 2018;12(2):120-7. [Persian] [Link]
31. Ghazi Saeidi M, Moghimi Araghi S, Babadi S. Determining the required minimum data set and data elements to create a web-based electronic record for glaucoma patients. J Payavard Salamat. 2018;11(6):675-84. [Persian] [Link]
32. Rezaee R, AlizadehNaini M, Halim Z. Designing and implementation of web-based personal health record for patients with inflammatory bowel disease. Govaresh. 2018;23(2):100-6. [Persian] [Link]
33. Asgari I. Development an electronic oral health record application for educational dental setting. J Educ Health Promot. 2018;7:124. [Link] [DOI:10.4103/jehp.jehp_177_17]
34. Farzandipour M, Jeddi FR, Gilasi HR, Shirzadi D. Clinical and para clinical information needs of infertility electronic health records in Iran: A delphi study. Acta Inform Med. 2017;25(3):163-8. [Link] [DOI:10.5455/aim.2017.25.163-168]
35. Ghazisaeedi M, Tansaz M, Shahmoradi L, Nasiri A, Tahmasebi F, Sahraei Z. Electronic record for infertile patients based on traditional medicine approach. J Health Biomed Inform. 2017;3(4):259-71. [Persian] [Link]
36. Safdari R, Mohammazadeh N, Ggheibi N. Designing of elementary school student's health measurement electronic records. Health Inform Manag. 2017;13(7):491-7. [Persian] [Link]
37. Kamel Ghalibaf A, Mazloum Khorasani Z, Gholian-Aval M, Tabesh H, Tara M. Design, implementation, and evaluation of self-describing diabetes medical records: A pilot study. JMIR Med Inform. 2017;5(2):e10. [Link] [DOI:10.2196/medinform.6862]
38. Rezaei Hachesu P, Samad T, Soltani, Mirnia K. Designing an electronic medical record system of infants in hospitals of Tabriz University of Medical Sciences. J Health Biomed Inform. 2016;2(4):229-39. [Persian] [Link]
39. Safdari R, Ghazisaeidi M, Pezeshki A, Mahmoodzadeh B, Nikmaram A. The introduction of electronic medical records for chronic kidney disease as a reliable method for the diagnosis of the disease. J Adv Med Biomed Res. 2016;24(104):112-20. [Persian] [Link]
40. Azizi A, Aboutorabi R, Mazloum-Khorasani Z, Afzal-Aghaea M, Tara M. Development, validation, and evaluation of web-based iranian diabetic personal health record: rationale for and protocol of a randomized controlled trial. JMIR Res Protoc. 2016;5(1):e39. [Link] [DOI:10.2196/resprot.5201]
41. Langarizadeh M, Samimi M, Behzadian H. Development of personal health record applicationfor gestational diabetes, based on smart phone. Nurs Midwifery J. 2016;14(8):714-27. [Persian] [Link]
42. Samadpour H, Sadoughi F. Data set of electronic personal health records for Iranian students of medical sciences. Health Inform Manag. 2015;12(4):416-25. [Persian] [Link]
43. Babalhavaeji F, Emami Z, Shahrokhi Farid R. Information needs study on electronic health records of diabetic patients from endocrinologist perspective. J Health Manag. 2014;5(2):13-24. [Persian] [Link]
44. Abdolkhani R, Halabchi F, Safdari R, Dargahi H, Shadanfar K. Designing an electronic personal health record for professional Iranian athletes. Asian J Sports Med. 2014;5(4):e23809. [Link] [DOI:10.5812/asjsm.23809]
45. Ahmadi M, Khoshkam M, Babaei R. Information needs study on electronic health records of diabetic patients from nephrologist's perspective. J Health Admin. 2012;15(47):13-24. [Persian] [Link]
46. Afrizal SH, Hidayanto AN, Handayani PW, Budiharsana M, Eryando T. Narrative review for exploring barriers to readiness of electronic health record implementation in primary health care. Healthc Inform Res. 2019;25(3):141-52. [Link] [DOI:10.4258/hir.2019.25.3.141]
47. Jahanbakhsh M, Tavakoli N, Mokhtari H. Challenges of EHR implementation and related guidelines in Isfahan. Proc Comput Sci. 2011;3:1199-204. [Link] [DOI:10.1016/j.procs.2010.12.194]
48. Mansour E. Egyptian patients' perceptions of using personal health records (PHRs): an exploratory study. Global Knowledge, Memory and Communication. 2018;67(8/9):523-46. [Link] [DOI:10.1108/GKMC-04-2018-0034]
49. George TP, Hopla DL. Advantages of personal health records. Nurs 2020 Critic Care. 2015;10(6):10-2. [Link] [DOI:10.1097/01.CCN.0000472852.70431.1b]
50. Heart T, Ben-Assuli O, Shabtai I. A review of PHR, EMR and EHR integration: A more personalized healthcare and public health policy. Health Policy Technol. 2017;6(1):20-5. [Link] [DOI:10.1016/j.hlpt.2016.08.002]
51. Sadoughi F, Nasiri S, Langarizadeh M. Necessity for designing national minimum data set of perinatal period in Iran: A review article. Med J Mashhad Univ Med Sci. 2014;57(5):727-37. [Persian] [Link]
52. Mahmoudvand Z, Kamkar M, Shahmoradi L, Nejad AF. Determination of Minimum Data Set (msd) in echocardiography reporting system to exchange with iran's Electronic Health Record (EHR) system. Acta Inform Med. 2016;24(2):116-9. [Link] [DOI:10.5455/aim.2016.24.116-119]
53. Weintraub WS, Karlsberg RP, Tcheng JE, Boris JR, Buxton AE, et al. ACCF/AHA 2011 key data elements and definitions of a base cardiovascular vocabulary for electronic health records: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards. Circulation. 2011;124(1):103-23. [Link] [DOI:10.1161/CIR.0b013e31821ccf71]
54. Abbasi M, Ahmadian L, Amirian M, Tabesh H, Eslami S. The development of a minimum data set for an infertility registry. Perspec Health Inf Manag. 2018;15(Winter):1b [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |