Volume 10, Issue 4 (2022)
Health Educ Health Promot 2022, 10(4): 711-718 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Darabi A, Tahmasebi R, Vahdat K, Noroozi A. Predictive Factors of COVID-19 Vaccine Acceptance Based on COM-B Model. Health Educ Health Promot 2022; 10 (4) :711-718
URL: http://hehp.modares.ac.ir/article-5-61593-en.html
URL: http://hehp.modares.ac.ir/article-5-61593-en.html
1- Persian Gulf Tropical Medicine Research Center, Bushehr University of Medical Sciences, Bushehr, Iran
2- Department of Epidemiology and Biostatistics, School of Health, Bushehr University of Medical Sciences, Bushehr, Iran
3- Department of Infectious Diseases, School of Medicine, Bushehr University of Medical Science, Bushehr, Iran
4- Department of Health Education, School of Health, Bushehr University of Medical Sciences, Bushehr, Iran , azitanoroozi@yahoo.com
2- Department of Epidemiology and Biostatistics, School of Health, Bushehr University of Medical Sciences, Bushehr, Iran
3- Department of Infectious Diseases, School of Medicine, Bushehr University of Medical Science, Bushehr, Iran
4- Department of Health Education, School of Health, Bushehr University of Medical Sciences, Bushehr, Iran , azitanoroozi@yahoo.com
Full-Text [PDF 1238 kb]
(908 Downloads)
| Abstract (HTML) (1016 Views)
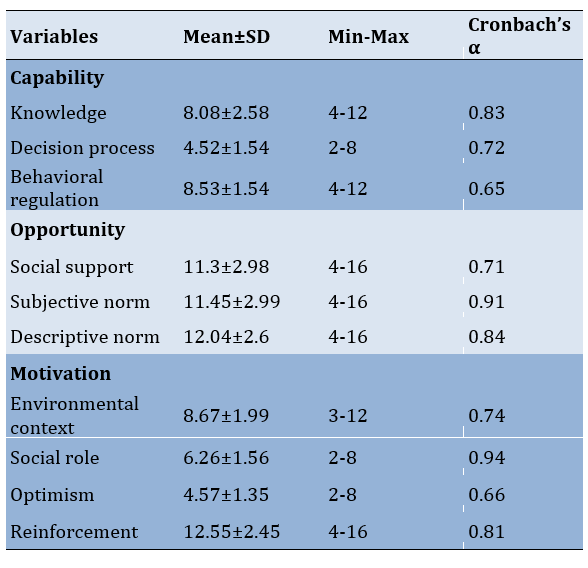
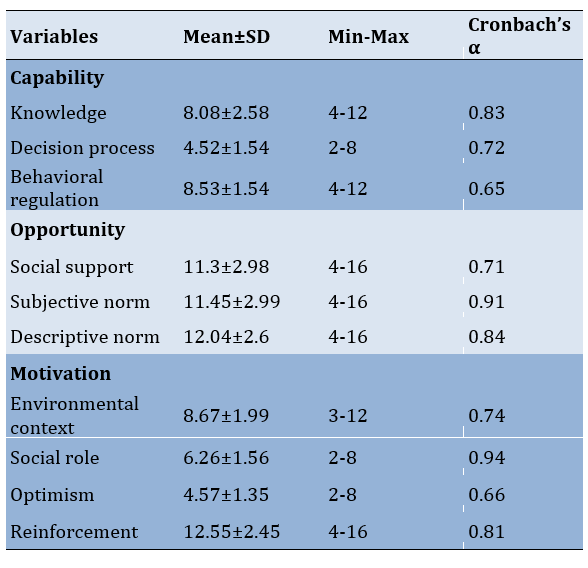
Table 1) Means, standard deviations, and minimum and maximum of the components (N=1102)
Structural equation modeling
The original hypothesized model did not produce a good fit for the data (χ2= 652.81; df = 84; p<0.001; RMSEA= 0.08 [0.07 - 0.09]; CFI= 0.57; AGFI= 0.97; AIC= 724.80). Examining the path coefficients in the hypothesized model showed that the path coefficient of opportunity of vaccine acceptance and capability to motivation were not significant (Figure 1). By considering the results of the original model and the related theoretical factors, the model was modified by dropping the paths with insignificant coefficients step by step and adding a path between capability and opportunity, and adding 6 error covariances. The fit indices showed improvement in the modified model over the original model (χ2= 388.61; df= 78; p<0.001; RMSEA= 0.06 [0.05 - 0.07]; CFI= 0.87; AGFI= 0.99; AIC= 472.61). The coefficients between the variables improved, and all the paths in the modified model were significant. All fit indices indicated a good fit for the model.
In the model fitted, opportunity was significant predictor of motivation (β=0.97, 95% CI, 0.92–0.99, p<0.001) and capability (β=0.84, 95% CI, 0.78–0.98, p<0.001). Capability (β=0.19, 95% CI, 0.03–1.02, p=0.004) and motivation (β= 0.70, 95% CI, 0.17– 0.86, p<0.001) had a Direct Effect (DE) on vaccine acceptance. Consequently, opportunity (IE=0.84, 95% CI, 0.80–0.88, p<0.001) only indirectly influenced vaccine acceptance via the mediator motivation (IE=0.68) and capability (IE=0.16), and this effect was substantial via the mediator motivation. The total effect of opportunity on vaccine acceptance was TE=0.84 making it the most important driver for vaccine acceptance, followed by Motivation, TE=0.7, and finally capability TE= 0.19 (Figure 2).
This model explained 93% of the variance in motivation, 70% of the variance in capability, and 74% of the variance in vaccine acceptance.
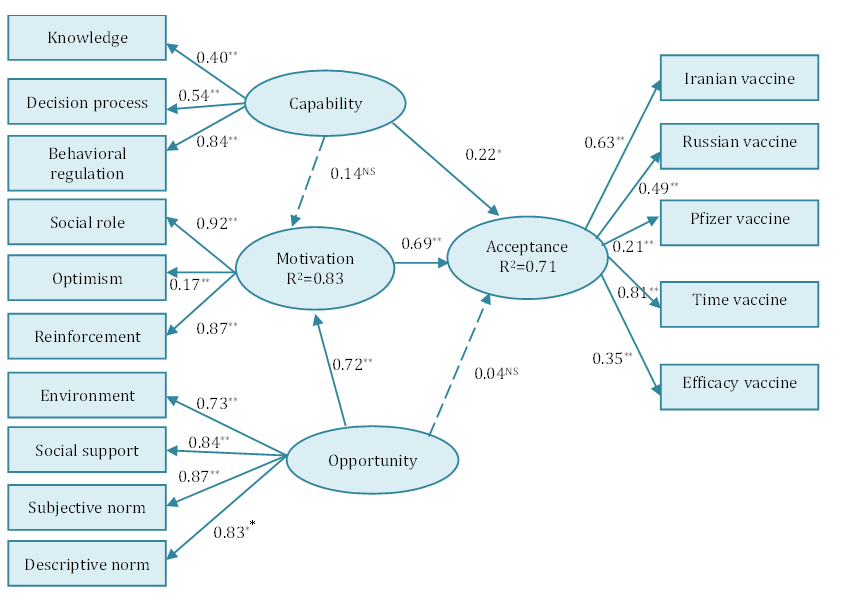
Figure 1) Original model of the COM-B. Components (latent variables) are represented by ovals and domains (observed variables) by rectangles. Outer weights of indicators and path coefficients are standardized. All paths are statistically significant (p<0.05) except for those indicated with a dashed line. *p<0.01, **p<0.001.
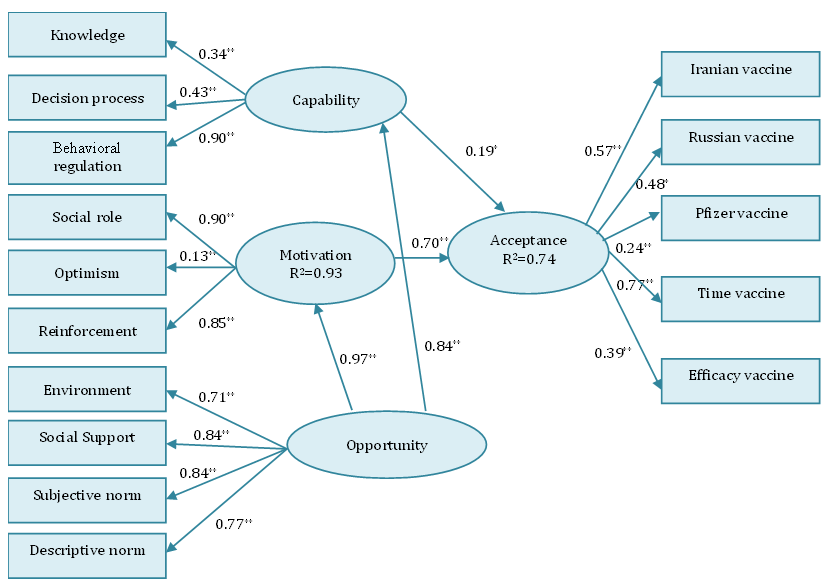
Figure 2) The fit model of the COM-B for vaccine acceptance. All paths are statistically significant (p<0.05). Standardized estimates are presented.
Discussion
This research examined the acceptance of the COVID-19 vaccine about the COM-B model of behavior change [10]. Initially, the 14 TDF domains were used to select appropriate criteria for each of the COM-B components. EFA resulted in the reduction of domains, leaving ten domains representing the three components of COM. In the modified model in SEM, all three components of the COM-B model were formed of the following domains: Capability was defined by knowledge, decisional process, and behavioral regulation; Opportunity was defined by social support, subjective norms, descriptive norms, and environmental context; Motivation was defined by social role, optimism/pessimism, and reinforcement. In capability, behavioral regulation had the strongest effect; in motivation, social role, and in opportunity, social support and subjective norm had the strongest effect. Motivation (strongly) and capability (weakly) were mediators for opportunity on vaccine acceptance. We found that all three COM-B components significantly predicted vaccine acceptance; and opportunity, followed by motivation had the greatest influence on behavior. The results show that the COM-B model, as a theoretical framework for the behavioral change wheel, is a strong predictor of COVID-19 vaccine acceptance in Iranian people (R2=0.74), and the opportunity component is a strong predictor of the motivation component (R2=0.93).
Since the strongest component of the COM-B model for vaccine acceptance is the opportunity component, which is strongly explained by social support and subjective norm, so it can be said that the most important domains affecting vaccine acceptance are social support and subjective norm.
In line with the findings of this study, it was determined that informational support in the form of knowledge about vaccination, emotional support in the form of encouragement regarding vaccination, and instrumental support in the form of access to the vaccine are effective in vaccine acceptance [19]. In our study, the opportunity component was effective in vaccine acceptance by influencing the capability component (raising knowledge, behavioral regulation, and building the decision process) and the motivation component (reinforcing individuals, optimism, and social role).
In the context of intention to be vaccinated, the critical role of subjective norm has been reported in several research studies [20-23]. Griffin et al. argued that the subjective norm could play an essential role in seeking and processing information [24]. Also, according to Baron et al. [25], peer pressure to receive influenza vaccination has an impact on the decision process, and behavioral regulation (domains of capability component) to accept influenza vaccination. In the present study, the opportunity component affected the capability component and indirectly the vaccine acceptance, so it seems that the subjective norm that is the main explanation of the opportunity component can affect people's capability and indirectly the vaccine acceptance by influencing the seeking and processing information. Also, based on the theory of planned behavior, subjective norms are somewhat useful in initiating health behaviors through motivations [26]. This implies that subjective norms may urge motivation because people feel that they are being controlled by their doctors, family members, and important others [27]. On the other hand, other studies established that people who get vaccinated generally believe that adopting this behavior is a social role (a domain of motivation component) [28-31]. In current study, subjective norm as a domain of opportunity component affects motivation and thus affects vaccine acceptance.
In the COM-B model, complex and interrelationships between the three components of capability, motivation and opportunity as well as behavior are possible, and Michie et al. did not elaborate on the role of motivation as a mediator for the effect of capability and opportunity on behavior [10]. According to this, in our study one path added from opportunity to capability, therefore two one-way paths were created from opportunity à capability à vaccine acceptance and also from opportunity à motivation à vaccine acceptance. Opportunity greatly affects motivation, as well as capability. The strong impact of opportunity on motivation and capability reflects the importance of environmental and social factors that enhance motivation and capability and indirectly affect vaccine acceptance.
This study has strengths and limitations. This is the first study to our knowledge that examines personal, interpersonal, and social factors (in the form of the COM-B model) affecting vaccine acceptance in Iran. Given the essence of this model, by identifying domains affecting the behavioral change wheel, effective interventions and policies can now be proposed to increase the acceptance of the COVID-19 vaccine. However, despite the large sample size and sampling frame, this was not a real random probability sample (it was very difficult to obtain in the current situation). Also, individuals' decisions about participating in the study could be influenced by psychological factors, so there was a possibility of sampling bias. Due to the completion of questionnaires in the form of self-report, there was a possibility of reporting bias.
Conclusion
To increase the acceptance of COVID-19 vaccination, opportunities should be created in society through environmental changes (social support and environmental context) and interpersonal relationships (subjective norm and descriptive norm). In other words, by creating communication campaigns, marketing, and demonstration of vaccine injection by policymakers, doctors, and healthcare workers, as well as making the vaccine available in offices and public centers, people should be motivated to get vaccinated. On the other hand, providing environmental and interpersonal conditions has created in people the capability to make decisions and regulate behavior, and in addition, it increases people's knowledge about COVID-19 vaccination.
Acknowledgements: None declared by the authors.
Ethical Permission: This research was approved by the Ethics Committee of Bushehr University of Medical Sciences (protocol number: IR.BpUMS.REC.1399.192), dated 10 February 2021. This study was conducted based on the Declaration of Helsinki.
Conflicts of Interests: The authors declare that they have no conflicts of interest in this work.
Authors’ Contribution: Darabi A (First Author), Introduction Writer/Main Researcher (25%); Tahmasebi R (Second Author), Methodologist/Assistant Researcher (25%); Vahdat K (Third author), Statistical Analyst (25%); Noroozi A (Fourth Author), Assistant Researcher (25%)
Funding/Support: No fund was received.
Full-Text: (438 Views)
Introduction
The coronavirus 2 (SARS-CoV-2) pandemic has infected more than 14 million people and killed more than 2 million people worldwide by March 3, 2021 [1]. This pandemic is a major threat to the public health system and has serious economic consequences for the world [2, 3]. Vaccination is essential to control COVID-19 and end social distancing. Researchers around the world are working on vaccine development and testing, and to date, several vaccines have been developed and some are available [4]. However, the success of this strategy depends on public acceptance of the vaccine. In recent years, vaccination rates and public confidence in vaccines have been declining [5, 6]. Vaccine hesitancy was evident during the H1N1 swine flu outbreak in 2009, so in most countries, less than half of the target population received the vaccine [7]. Given the potential for poor coverage of COVID-19 vaccination, the World Health Organization (WHO) recommends, "Every country should have a strategy to increase vaccination acceptance and willingness" [8].
The psychology of health and preventive behaviors play a key role in understanding the mechanisms that drive people toward behavior [9]. In this regard, behavioral scientists use theories and models of behavior change to identify factors affecting behavior and design effective interventions in this field. One of the models formed from the combination of existing models in behavior change is the Behavior Change Wheel (BCW) [10]. The BCW recognized three levels illustrating the translational process from essential conditions, through intervention functions, to policy. The researchers identified three conditions (capability, motivation, and opportunity) that are deemed essential for behavior change. These three Components, Capability, Opportunity, and Motivation, are called COM-B, which are behavioral stimuli. The COM-B components are the core of BCW, which allows the systematic development of behavior change interventions and necessary policies [10, 11]. In COM-B, the capability is defined as a person's physical and psychological capacity to perform the relevant activity, which includes having the necessary knowledge and skills. Motivation includes brain processes that stimulate and guide behavior and includes habitual processes, emotional responses as well as conscious decision-making. The opportunity involves factors that are outside the individual and make the behavior possible or prompt it [10]. According to this model, capability and opportunity affect and mediate motivation. Thus, capability and opportunity affect behavior through a direct and indirect path [10].
Summarizing the theories of behavior change shows that a total of 33 theories and 128 constructs are used to explain behavior, which lead to the theoretical domains framework (TDF), consisting of 14 domains [12, 13]. TDF covers a wide range of behavioral determinants and is used directly in the formation of the three components of COM-B [14]. The fourteen TDF domains separated by COM-B components are as follows:
• Capability includes knowledge, memory/attention and decision process, behavioral regulation, and skill.
The coronavirus 2 (SARS-CoV-2) pandemic has infected more than 14 million people and killed more than 2 million people worldwide by March 3, 2021 [1]. This pandemic is a major threat to the public health system and has serious economic consequences for the world [2, 3]. Vaccination is essential to control COVID-19 and end social distancing. Researchers around the world are working on vaccine development and testing, and to date, several vaccines have been developed and some are available [4]. However, the success of this strategy depends on public acceptance of the vaccine. In recent years, vaccination rates and public confidence in vaccines have been declining [5, 6]. Vaccine hesitancy was evident during the H1N1 swine flu outbreak in 2009, so in most countries, less than half of the target population received the vaccine [7]. Given the potential for poor coverage of COVID-19 vaccination, the World Health Organization (WHO) recommends, "Every country should have a strategy to increase vaccination acceptance and willingness" [8].
The psychology of health and preventive behaviors play a key role in understanding the mechanisms that drive people toward behavior [9]. In this regard, behavioral scientists use theories and models of behavior change to identify factors affecting behavior and design effective interventions in this field. One of the models formed from the combination of existing models in behavior change is the Behavior Change Wheel (BCW) [10]. The BCW recognized three levels illustrating the translational process from essential conditions, through intervention functions, to policy. The researchers identified three conditions (capability, motivation, and opportunity) that are deemed essential for behavior change. These three Components, Capability, Opportunity, and Motivation, are called COM-B, which are behavioral stimuli. The COM-B components are the core of BCW, which allows the systematic development of behavior change interventions and necessary policies [10, 11]. In COM-B, the capability is defined as a person's physical and psychological capacity to perform the relevant activity, which includes having the necessary knowledge and skills. Motivation includes brain processes that stimulate and guide behavior and includes habitual processes, emotional responses as well as conscious decision-making. The opportunity involves factors that are outside the individual and make the behavior possible or prompt it [10]. According to this model, capability and opportunity affect and mediate motivation. Thus, capability and opportunity affect behavior through a direct and indirect path [10].
Summarizing the theories of behavior change shows that a total of 33 theories and 128 constructs are used to explain behavior, which lead to the theoretical domains framework (TDF), consisting of 14 domains [12, 13]. TDF covers a wide range of behavioral determinants and is used directly in the formation of the three components of COM-B [14]. The fourteen TDF domains separated by COM-B components are as follows:
• Capability includes knowledge, memory/attention and decision process, behavioral regulation, and skill.
• Opportunity includes social influence (such as social support, subjective norms, and descriptive norms), environmental context and resources.
• Motivation includes social role, optimism, belief in capability, belief in consequences, intention, goals, reinforcement, and emotion [13].
• Motivation includes social role, optimism, belief in capability, belief in consequences, intention, goals, reinforcement, and emotion [13].
The relevance of these TDF domains depends on the target behavior and target population. Therefore, the use of the COM-B model for COVID-19 vaccine acceptance enables us to identify the factors influencing acceptance [13, 14], and to select the interventions and policies influencing vaccine acceptance based on the identified factors. However, the researchers have not found any study and scale based on COM-B in published documents for COVID-19 vaccine acceptance. Thus, the current study aimed to development a multi-component questionnaire based on COM-B.
Instrument and Methods
Study design
In this cross-sectional study, 1102 adults aged 18 years and older living in Bushehr province were selected from February 25 to 28, 2021 via multi-stage sampling method.
According to the previous literature review of vaccine acceptance [15], it is estimated that about 60% of the study participants showed vaccine acceptance. We estimated that with 80% power at a confidence level of 95%, the adequate sample size is 754. Accounting for a 40% attrition rate in an online survey, our final sample size was planned to be 1056.
For sampling, first, out of 10 cities of Bushehr province, four cities were randomly selected (Dayyer Port, Daylam Port, Jam, Bushehr Port); in the selected cities, according to the number of urban and rural health centers in each city, a number of centers were randomly selected. Then, based on the population of adults aged 18 and older in the selected centers of these four cities and taking into account the sample size (1054 participants), the sample size of each center in the four cities was determined.
At each center, a health care provider announced readiness for sampling. The online questionnaire was sent to health care providers, and the questionnaire link was sent by health care providers through the WhatsApp Platform to the primary participants of each center. The primary participants were requested to participate in the survey. On receiving and clicking the link, participants got auto-directed to the informed consent page, followed by the questionnaires.
Sending the questionnaire link for each center continued until the number of completed questionnaires of the center reached the desired sample size.
In this study, the inclusion criteria were older than 18 years, having the ability to read and write, having a smartphone and WhatsApp messaging tools, and having the ability to work with WhatsApp messaging software.
Instrument and measures
The self-administered questionnaire included three sections comprised of demographic factors, questions regarding the 14 TDF domains related to COM-B components, and vaccine acceptance questions.
The demographic section evaluated age, sex, education level, and income status. The second section was designed based on 14 TDF domains related to COM-B components.
In each behavior, there are some TDF domains that are deemed unnecessary. For example, in the knowledge domain, there are three components including knowledge of the condition, procedural knowledge, and knowledge of the task environment [13, 16]. Knowledge of conditions and procedural knowledge would only be relevant for vaccine acceptance. Also, the domain of intention and goal, considering that in this study the acceptance of the vaccine was examined, not the vaccination, was removed from the motivation component. Therefore, these components and knowledge of the task environment were not measured in this study.
In the capability component, 4 TDF domains including knowledge (5 items e.g. “I know how many doses I have to get the Covid-19 vaccine.”), decision process (3 items e.g. “Before deciding whether to receive the Covid-19 vaccine, I will review the protocols for this vaccine.”), behavioral regulation (3 items e.g. “I want to end corona’s lifestyle with the vaccination.”), and skill (2 items e.g. “Every year, at the beginning of the cold season, I and my family get the flu vaccine.”) were assessed with 13 questions.
In the opportunity component, 4 TDF domains including social support (4 items e.g. “The government and health policymakers plan to get people the best and most effective type of Covid-19 vaccine.”), subjective norms (4 items e.g. “My family expects me to get the Covid-19 vaccine.”), descriptive norms (4 items e.g. “I think policymakers will inject the Covid-19 vaccine.”), and environmental context (3 items e.g. “In the current socio-economic situation, sufficient financial support will be provided by the authorities, insurance companies and the government to receive the vaccine.”) were assessed with 15 questions.
In the motivation component, 6 TDF domains including social role (2 items e.g. “As a member of my family and to protect my family members, I have a responsibility to get the Covid-19 vaccine.”), optimism (4 items e.g. “I have been hoping for the future since I found out the Corona vaccine was made.”), belief in capability (2 items e.g. “If I have to pay for the vaccine, the cost for me is ......”), belief in consequences (3 items e.g. “I believe that the vaccine is effective in preventing covid-19.”), reinforcement (2 items e.g. “My family's health is important to me, and the Covid-19 vaccine helps keep my family healthy.”), and emotion (3 items e.g. “I'm worried about the side effects of the vaccine.”) were assessed with 16 questions.
All items related to domains except knowledge are scored on a 4- point Likert scale, but items related to knowledge are scored on a 3-point Likert scale.
In the study, items were adapted from a preliminary version of the COM-B self-evaluation questionnaire [16, 17]. They have developed a questionnaire in English and Dutch able to discriminately assess TDF domains based on Cane et al.’s 14-domain [14]. Exploratory factor analysis was performed for construct validity and psychometry of the questionnaire.
The third section was a self-administered questionnaire that assessed vaccine acceptance in different conditions including country of manufacture (4 items), effectiveness (2 items), and timing of vaccination (2 items). The items in this section were scored by “yes/no” or “yes/no and I do not vaccinate”. Items about the effectiveness and timing of vaccination had conditional answers. Each item received different points depending on the type of question.
For content validity, ten health education specialists were asked to evaluate the content validity of the constructs using the Content Validity Index (CVI). Its CVI values for simplicity, precision, and specificity were 0.99, 0.98, and 0.98, respectively, which indicate its appropriateness of content validity. Exploratory Factor Analysis (EFA) of COM-B scale was used to measure psychometric properties. The reliability score of each domain was obtained and reported in Table 1. The average responses of the confirmed domains and the vaccine acceptance are summarized in Table 1.
Data analysis
Data description and EFA were done with SPSS 22 software, and Structural Equation Modeling (SEM) was performed using IBM SPSS AMOS, version 22. EFA was used to determine the number of domains related to each component of the COM-B model. Oblimin with Kaiser Normalization procedures were used to rotate the factors. To examine the data via rotated factor analysis, investigators set the criteria of eigenvalue at a minimum of 1, minimum factor loading of 0.40, and a maximum of 25 rotation iterations [18].
Structural equation modeling is a multivariate statistical analysis technique used to analyze structural relationships between measured variables and latent constructs. In this study, multivariate kurtosis was estimated to be 26.04 and critical region (C.r.) 19.14; accordingly, a few of variables were abnormal. Therefore, we used the asymptotically distribution-free (Weighted Least Squared) estimation method.
The bootstrapping method was used to determine the Confidence Intervals (CI) of the path coefficients. A final measurement model was established through model trimming by removing statistically non-significant (p>0.05) paths step by step. The modification index was used to include additional parameters. The Chi-square test, Adjusted Goodness-of-Fit Index (AGFI), and Root-Mean-Square Error of Approximation (RMSEA) were used as model fit criteria. The model was considered fit if the AGFI value was greater than 0.9 and if the RMSEA value was less than 0.08. For model comparison, a Comparative Fit Index (CFI) was selected. Values of 0.90 or greater for CFI are recommended as acceptable values for this measure. Model Parsimony was evaluated by Akaike Information Criterion (AIC).
Finally, direct and indirect path coefficients were estimated and the explained variance of R2 was obtained for the two variables of motivation and vaccine acceptance. All coefficients are reported as standardized.
Findings
The link of the questionnaire was disseminated to 3226 adults, and 1102 (51%) individuals completed it. Of these, 50.4% (555) lived in Bushehr Port, and 19.5% (n=215), 15.3% (n=169), and 14.8% (n=163) lived in Jam, Dayyer Port, and Daylam Port, respectively. Most of the respondents were female (63.8%). The mean age of respondents was 35.66±10.24 years and ranged from 18 to 85 years old. Of 1102 respondents, 12.4% (n=137) were educated to primary/secondary level of education, 24.6% (n=271) were graduated to the high school level, and 53% (n=648) had obtained a university degree. Of the entire study sample, 52.5% (n=579) of respondents rated their income as fairly sufficient.
When asked whether they intend to get the COVID-19 vaccine, 726 participants (65.9%) wanted to get the Iranian vaccine, 437 (39.7%) Russian/Chinese vaccine, and 633 (57.4%) Pfizer/Moderna vaccine. 164 respondents (14.9%) also refused to receive the vaccine. Of the total 1102 respondents, 769 (69.8%) will accept vaccination if the COVID-19 vaccine was highly effective. 719 participants (65.2%) wanted to get vaccinated as soon as possible when it becomes available, while others (34.8%) will delay vaccination until they could confirm the vaccine’s safety.
Capability
The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.78, showing the sample was large enough to perform a satisfactory factor analysis. Bartlett’s test of sphericity was significant (χ2=3415.6, df= 55, p=0.0001), indicating that there were some relationships among the items. Factor analysis rotation converged at nine iterations. In this component, the factor analysis of the principal axis revealed 3 domains with an eigenvalue >1, which explains 44.47% of the total variance of the sample. Four items (one item of knowledge, one item of decision process, and all items of skill) were omitted. Therefore, this component was confirmed with 3 domains (including knowledge with 4 items, decision processes with 2 items, and behavioral regulation with 3 items).
Opportunity
The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.93, showing the sample was large enough to perform a satisfactory factor analysis. Bartlett’s test of sphericity was significant (χ2=7374.8, df= 105, p=0.0001), indicating that there were some relationships among the items. Factor analysis rotation converged at eight iterations. In this component, the factor analysis of the principal axis revealed 4 domains with an eigenvalue >1, explaining 53.49% of the total sample variance. No items were deleted in this component. Therefore, this component was confirmed with 4 domains (including social support with 4 items, subjective norm with 4 items, descriptive norm with 4 items, and environmental context with 3 items).
Motivation
The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.87, showing the sample was large enough to perform a satisfactory factor analysis. Bartlett’s test of sphericity was significant (χ2=6983.8, df= 120, p=0.0001), indicating that there were some relationships among the items. Factor analysis rotation converged at 20 iterations. In this component, the factor analysis of the principal axis revealed 3 domains with an eigenvalue >1, explaining 44.28% of the total sample variance. Six items (all items of belief about capability, two items of belief about consequences, and two items of emotion) were omitted. Two items (one item of belief about consequences, and one item of emotion) had cross-loading, and these items were omitted too. Two items of optimism converted to reinforcement domain. Therefore, this component was confirmed with 3 domains (including social role with 2 items, optimism with 2 items, and reinforcement with 4 items).
The minimum and maximum scores of each domain that can be obtained are presented in Table 1.
Findings
In the present study, 599 out of 626 questionnaires were completed for data collection (95% response rate). The mean age of the samples was 33.63±10.71, most of whom (25.5%) were in the age group of 31 to 39 years. 57.30% of the samples were females. More than 66% of them had an associate's/ bachelor's degree or higher. Furthermore, about three-quarters (74.30%) of the samples were living in urban regions, and 46.58% of them had no history of the virus. Table 1 presents other characteristics of the samples.
Instrument and Methods
Study design
In this cross-sectional study, 1102 adults aged 18 years and older living in Bushehr province were selected from February 25 to 28, 2021 via multi-stage sampling method.
According to the previous literature review of vaccine acceptance [15], it is estimated that about 60% of the study participants showed vaccine acceptance. We estimated that with 80% power at a confidence level of 95%, the adequate sample size is 754. Accounting for a 40% attrition rate in an online survey, our final sample size was planned to be 1056.
For sampling, first, out of 10 cities of Bushehr province, four cities were randomly selected (Dayyer Port, Daylam Port, Jam, Bushehr Port); in the selected cities, according to the number of urban and rural health centers in each city, a number of centers were randomly selected. Then, based on the population of adults aged 18 and older in the selected centers of these four cities and taking into account the sample size (1054 participants), the sample size of each center in the four cities was determined.
At each center, a health care provider announced readiness for sampling. The online questionnaire was sent to health care providers, and the questionnaire link was sent by health care providers through the WhatsApp Platform to the primary participants of each center. The primary participants were requested to participate in the survey. On receiving and clicking the link, participants got auto-directed to the informed consent page, followed by the questionnaires.
Sending the questionnaire link for each center continued until the number of completed questionnaires of the center reached the desired sample size.
In this study, the inclusion criteria were older than 18 years, having the ability to read and write, having a smartphone and WhatsApp messaging tools, and having the ability to work with WhatsApp messaging software.
Instrument and measures
The self-administered questionnaire included three sections comprised of demographic factors, questions regarding the 14 TDF domains related to COM-B components, and vaccine acceptance questions.
The demographic section evaluated age, sex, education level, and income status. The second section was designed based on 14 TDF domains related to COM-B components.
In each behavior, there are some TDF domains that are deemed unnecessary. For example, in the knowledge domain, there are three components including knowledge of the condition, procedural knowledge, and knowledge of the task environment [13, 16]. Knowledge of conditions and procedural knowledge would only be relevant for vaccine acceptance. Also, the domain of intention and goal, considering that in this study the acceptance of the vaccine was examined, not the vaccination, was removed from the motivation component. Therefore, these components and knowledge of the task environment were not measured in this study.
In the capability component, 4 TDF domains including knowledge (5 items e.g. “I know how many doses I have to get the Covid-19 vaccine.”), decision process (3 items e.g. “Before deciding whether to receive the Covid-19 vaccine, I will review the protocols for this vaccine.”), behavioral regulation (3 items e.g. “I want to end corona’s lifestyle with the vaccination.”), and skill (2 items e.g. “Every year, at the beginning of the cold season, I and my family get the flu vaccine.”) were assessed with 13 questions.
In the opportunity component, 4 TDF domains including social support (4 items e.g. “The government and health policymakers plan to get people the best and most effective type of Covid-19 vaccine.”), subjective norms (4 items e.g. “My family expects me to get the Covid-19 vaccine.”), descriptive norms (4 items e.g. “I think policymakers will inject the Covid-19 vaccine.”), and environmental context (3 items e.g. “In the current socio-economic situation, sufficient financial support will be provided by the authorities, insurance companies and the government to receive the vaccine.”) were assessed with 15 questions.
In the motivation component, 6 TDF domains including social role (2 items e.g. “As a member of my family and to protect my family members, I have a responsibility to get the Covid-19 vaccine.”), optimism (4 items e.g. “I have been hoping for the future since I found out the Corona vaccine was made.”), belief in capability (2 items e.g. “If I have to pay for the vaccine, the cost for me is ......”), belief in consequences (3 items e.g. “I believe that the vaccine is effective in preventing covid-19.”), reinforcement (2 items e.g. “My family's health is important to me, and the Covid-19 vaccine helps keep my family healthy.”), and emotion (3 items e.g. “I'm worried about the side effects of the vaccine.”) were assessed with 16 questions.
All items related to domains except knowledge are scored on a 4- point Likert scale, but items related to knowledge are scored on a 3-point Likert scale.
In the study, items were adapted from a preliminary version of the COM-B self-evaluation questionnaire [16, 17]. They have developed a questionnaire in English and Dutch able to discriminately assess TDF domains based on Cane et al.’s 14-domain [14]. Exploratory factor analysis was performed for construct validity and psychometry of the questionnaire.
The third section was a self-administered questionnaire that assessed vaccine acceptance in different conditions including country of manufacture (4 items), effectiveness (2 items), and timing of vaccination (2 items). The items in this section were scored by “yes/no” or “yes/no and I do not vaccinate”. Items about the effectiveness and timing of vaccination had conditional answers. Each item received different points depending on the type of question.
For content validity, ten health education specialists were asked to evaluate the content validity of the constructs using the Content Validity Index (CVI). Its CVI values for simplicity, precision, and specificity were 0.99, 0.98, and 0.98, respectively, which indicate its appropriateness of content validity. Exploratory Factor Analysis (EFA) of COM-B scale was used to measure psychometric properties. The reliability score of each domain was obtained and reported in Table 1. The average responses of the confirmed domains and the vaccine acceptance are summarized in Table 1.
Data analysis
Data description and EFA were done with SPSS 22 software, and Structural Equation Modeling (SEM) was performed using IBM SPSS AMOS, version 22. EFA was used to determine the number of domains related to each component of the COM-B model. Oblimin with Kaiser Normalization procedures were used to rotate the factors. To examine the data via rotated factor analysis, investigators set the criteria of eigenvalue at a minimum of 1, minimum factor loading of 0.40, and a maximum of 25 rotation iterations [18].
Structural equation modeling is a multivariate statistical analysis technique used to analyze structural relationships between measured variables and latent constructs. In this study, multivariate kurtosis was estimated to be 26.04 and critical region (C.r.) 19.14; accordingly, a few of variables were abnormal. Therefore, we used the asymptotically distribution-free (Weighted Least Squared) estimation method.
The bootstrapping method was used to determine the Confidence Intervals (CI) of the path coefficients. A final measurement model was established through model trimming by removing statistically non-significant (p>0.05) paths step by step. The modification index was used to include additional parameters. The Chi-square test, Adjusted Goodness-of-Fit Index (AGFI), and Root-Mean-Square Error of Approximation (RMSEA) were used as model fit criteria. The model was considered fit if the AGFI value was greater than 0.9 and if the RMSEA value was less than 0.08. For model comparison, a Comparative Fit Index (CFI) was selected. Values of 0.90 or greater for CFI are recommended as acceptable values for this measure. Model Parsimony was evaluated by Akaike Information Criterion (AIC).
Finally, direct and indirect path coefficients were estimated and the explained variance of R2 was obtained for the two variables of motivation and vaccine acceptance. All coefficients are reported as standardized.
Findings
The link of the questionnaire was disseminated to 3226 adults, and 1102 (51%) individuals completed it. Of these, 50.4% (555) lived in Bushehr Port, and 19.5% (n=215), 15.3% (n=169), and 14.8% (n=163) lived in Jam, Dayyer Port, and Daylam Port, respectively. Most of the respondents were female (63.8%). The mean age of respondents was 35.66±10.24 years and ranged from 18 to 85 years old. Of 1102 respondents, 12.4% (n=137) were educated to primary/secondary level of education, 24.6% (n=271) were graduated to the high school level, and 53% (n=648) had obtained a university degree. Of the entire study sample, 52.5% (n=579) of respondents rated their income as fairly sufficient.
When asked whether they intend to get the COVID-19 vaccine, 726 participants (65.9%) wanted to get the Iranian vaccine, 437 (39.7%) Russian/Chinese vaccine, and 633 (57.4%) Pfizer/Moderna vaccine. 164 respondents (14.9%) also refused to receive the vaccine. Of the total 1102 respondents, 769 (69.8%) will accept vaccination if the COVID-19 vaccine was highly effective. 719 participants (65.2%) wanted to get vaccinated as soon as possible when it becomes available, while others (34.8%) will delay vaccination until they could confirm the vaccine’s safety.
Capability
The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.78, showing the sample was large enough to perform a satisfactory factor analysis. Bartlett’s test of sphericity was significant (χ2=3415.6, df= 55, p=0.0001), indicating that there were some relationships among the items. Factor analysis rotation converged at nine iterations. In this component, the factor analysis of the principal axis revealed 3 domains with an eigenvalue >1, which explains 44.47% of the total variance of the sample. Four items (one item of knowledge, one item of decision process, and all items of skill) were omitted. Therefore, this component was confirmed with 3 domains (including knowledge with 4 items, decision processes with 2 items, and behavioral regulation with 3 items).
Opportunity
The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.93, showing the sample was large enough to perform a satisfactory factor analysis. Bartlett’s test of sphericity was significant (χ2=7374.8, df= 105, p=0.0001), indicating that there were some relationships among the items. Factor analysis rotation converged at eight iterations. In this component, the factor analysis of the principal axis revealed 4 domains with an eigenvalue >1, explaining 53.49% of the total sample variance. No items were deleted in this component. Therefore, this component was confirmed with 4 domains (including social support with 4 items, subjective norm with 4 items, descriptive norm with 4 items, and environmental context with 3 items).
Motivation
The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.87, showing the sample was large enough to perform a satisfactory factor analysis. Bartlett’s test of sphericity was significant (χ2=6983.8, df= 120, p=0.0001), indicating that there were some relationships among the items. Factor analysis rotation converged at 20 iterations. In this component, the factor analysis of the principal axis revealed 3 domains with an eigenvalue >1, explaining 44.28% of the total sample variance. Six items (all items of belief about capability, two items of belief about consequences, and two items of emotion) were omitted. Two items (one item of belief about consequences, and one item of emotion) had cross-loading, and these items were omitted too. Two items of optimism converted to reinforcement domain. Therefore, this component was confirmed with 3 domains (including social role with 2 items, optimism with 2 items, and reinforcement with 4 items).
The minimum and maximum scores of each domain that can be obtained are presented in Table 1.
Findings
In the present study, 599 out of 626 questionnaires were completed for data collection (95% response rate). The mean age of the samples was 33.63±10.71, most of whom (25.5%) were in the age group of 31 to 39 years. 57.30% of the samples were females. More than 66% of them had an associate's/ bachelor's degree or higher. Furthermore, about three-quarters (74.30%) of the samples were living in urban regions, and 46.58% of them had no history of the virus. Table 1 presents other characteristics of the samples.
Table 1) Means, standard deviations, and minimum and maximum of the components (N=1102)
Structural equation modeling
The original hypothesized model did not produce a good fit for the data (χ2= 652.81; df = 84; p<0.001; RMSEA= 0.08 [0.07 - 0.09]; CFI= 0.57; AGFI= 0.97; AIC= 724.80). Examining the path coefficients in the hypothesized model showed that the path coefficient of opportunity of vaccine acceptance and capability to motivation were not significant (Figure 1). By considering the results of the original model and the related theoretical factors, the model was modified by dropping the paths with insignificant coefficients step by step and adding a path between capability and opportunity, and adding 6 error covariances. The fit indices showed improvement in the modified model over the original model (χ2= 388.61; df= 78; p<0.001; RMSEA= 0.06 [0.05 - 0.07]; CFI= 0.87; AGFI= 0.99; AIC= 472.61). The coefficients between the variables improved, and all the paths in the modified model were significant. All fit indices indicated a good fit for the model.
In the model fitted, opportunity was significant predictor of motivation (β=0.97, 95% CI, 0.92–0.99, p<0.001) and capability (β=0.84, 95% CI, 0.78–0.98, p<0.001). Capability (β=0.19, 95% CI, 0.03–1.02, p=0.004) and motivation (β= 0.70, 95% CI, 0.17– 0.86, p<0.001) had a Direct Effect (DE) on vaccine acceptance. Consequently, opportunity (IE=0.84, 95% CI, 0.80–0.88, p<0.001) only indirectly influenced vaccine acceptance via the mediator motivation (IE=0.68) and capability (IE=0.16), and this effect was substantial via the mediator motivation. The total effect of opportunity on vaccine acceptance was TE=0.84 making it the most important driver for vaccine acceptance, followed by Motivation, TE=0.7, and finally capability TE= 0.19 (Figure 2).
This model explained 93% of the variance in motivation, 70% of the variance in capability, and 74% of the variance in vaccine acceptance.
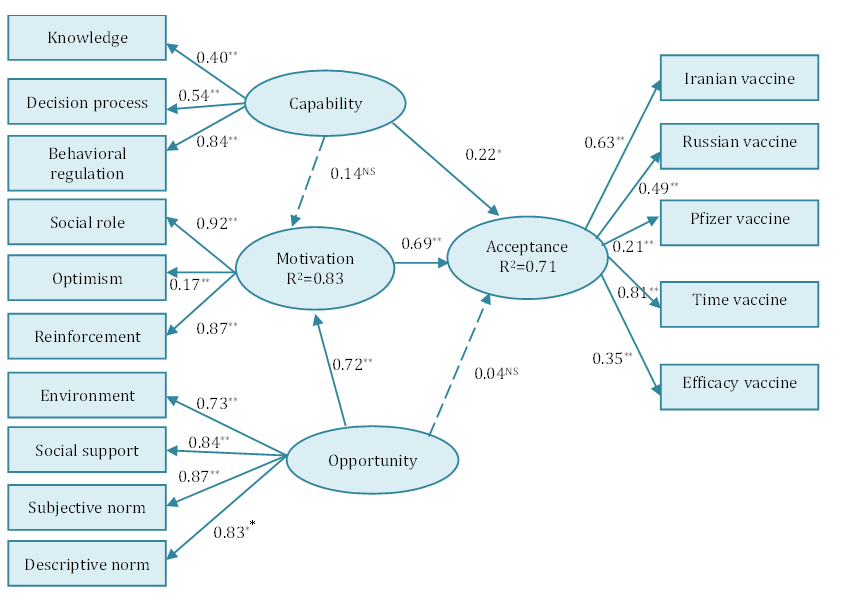
Figure 1) Original model of the COM-B. Components (latent variables) are represented by ovals and domains (observed variables) by rectangles. Outer weights of indicators and path coefficients are standardized. All paths are statistically significant (p<0.05) except for those indicated with a dashed line. *p<0.01, **p<0.001.
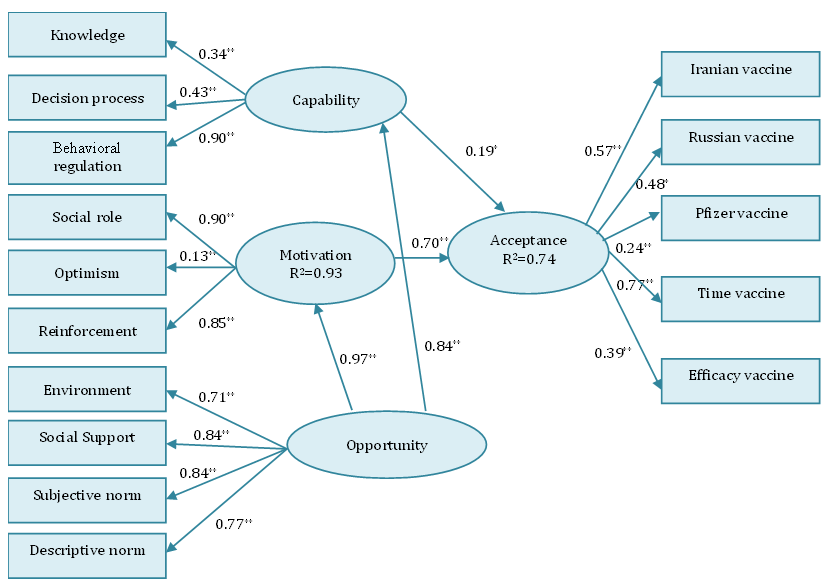
Figure 2) The fit model of the COM-B for vaccine acceptance. All paths are statistically significant (p<0.05). Standardized estimates are presented.
Discussion
This research examined the acceptance of the COVID-19 vaccine about the COM-B model of behavior change [10]. Initially, the 14 TDF domains were used to select appropriate criteria for each of the COM-B components. EFA resulted in the reduction of domains, leaving ten domains representing the three components of COM. In the modified model in SEM, all three components of the COM-B model were formed of the following domains: Capability was defined by knowledge, decisional process, and behavioral regulation; Opportunity was defined by social support, subjective norms, descriptive norms, and environmental context; Motivation was defined by social role, optimism/pessimism, and reinforcement. In capability, behavioral regulation had the strongest effect; in motivation, social role, and in opportunity, social support and subjective norm had the strongest effect. Motivation (strongly) and capability (weakly) were mediators for opportunity on vaccine acceptance. We found that all three COM-B components significantly predicted vaccine acceptance; and opportunity, followed by motivation had the greatest influence on behavior. The results show that the COM-B model, as a theoretical framework for the behavioral change wheel, is a strong predictor of COVID-19 vaccine acceptance in Iranian people (R2=0.74), and the opportunity component is a strong predictor of the motivation component (R2=0.93).
Since the strongest component of the COM-B model for vaccine acceptance is the opportunity component, which is strongly explained by social support and subjective norm, so it can be said that the most important domains affecting vaccine acceptance are social support and subjective norm.
In line with the findings of this study, it was determined that informational support in the form of knowledge about vaccination, emotional support in the form of encouragement regarding vaccination, and instrumental support in the form of access to the vaccine are effective in vaccine acceptance [19]. In our study, the opportunity component was effective in vaccine acceptance by influencing the capability component (raising knowledge, behavioral regulation, and building the decision process) and the motivation component (reinforcing individuals, optimism, and social role).
In the context of intention to be vaccinated, the critical role of subjective norm has been reported in several research studies [20-23]. Griffin et al. argued that the subjective norm could play an essential role in seeking and processing information [24]. Also, according to Baron et al. [25], peer pressure to receive influenza vaccination has an impact on the decision process, and behavioral regulation (domains of capability component) to accept influenza vaccination. In the present study, the opportunity component affected the capability component and indirectly the vaccine acceptance, so it seems that the subjective norm that is the main explanation of the opportunity component can affect people's capability and indirectly the vaccine acceptance by influencing the seeking and processing information. Also, based on the theory of planned behavior, subjective norms are somewhat useful in initiating health behaviors through motivations [26]. This implies that subjective norms may urge motivation because people feel that they are being controlled by their doctors, family members, and important others [27]. On the other hand, other studies established that people who get vaccinated generally believe that adopting this behavior is a social role (a domain of motivation component) [28-31]. In current study, subjective norm as a domain of opportunity component affects motivation and thus affects vaccine acceptance.
In the COM-B model, complex and interrelationships between the three components of capability, motivation and opportunity as well as behavior are possible, and Michie et al. did not elaborate on the role of motivation as a mediator for the effect of capability and opportunity on behavior [10]. According to this, in our study one path added from opportunity to capability, therefore two one-way paths were created from opportunity à capability à vaccine acceptance and also from opportunity à motivation à vaccine acceptance. Opportunity greatly affects motivation, as well as capability. The strong impact of opportunity on motivation and capability reflects the importance of environmental and social factors that enhance motivation and capability and indirectly affect vaccine acceptance.
This study has strengths and limitations. This is the first study to our knowledge that examines personal, interpersonal, and social factors (in the form of the COM-B model) affecting vaccine acceptance in Iran. Given the essence of this model, by identifying domains affecting the behavioral change wheel, effective interventions and policies can now be proposed to increase the acceptance of the COVID-19 vaccine. However, despite the large sample size and sampling frame, this was not a real random probability sample (it was very difficult to obtain in the current situation). Also, individuals' decisions about participating in the study could be influenced by psychological factors, so there was a possibility of sampling bias. Due to the completion of questionnaires in the form of self-report, there was a possibility of reporting bias.
Conclusion
To increase the acceptance of COVID-19 vaccination, opportunities should be created in society through environmental changes (social support and environmental context) and interpersonal relationships (subjective norm and descriptive norm). In other words, by creating communication campaigns, marketing, and demonstration of vaccine injection by policymakers, doctors, and healthcare workers, as well as making the vaccine available in offices and public centers, people should be motivated to get vaccinated. On the other hand, providing environmental and interpersonal conditions has created in people the capability to make decisions and regulate behavior, and in addition, it increases people's knowledge about COVID-19 vaccination.
Acknowledgements: None declared by the authors.
Ethical Permission: This research was approved by the Ethics Committee of Bushehr University of Medical Sciences (protocol number: IR.BpUMS.REC.1399.192), dated 10 February 2021. This study was conducted based on the Declaration of Helsinki.
Conflicts of Interests: The authors declare that they have no conflicts of interest in this work.
Authors’ Contribution: Darabi A (First Author), Introduction Writer/Main Researcher (25%); Tahmasebi R (Second Author), Methodologist/Assistant Researcher (25%); Vahdat K (Third author), Statistical Analyst (25%); Noroozi A (Fourth Author), Assistant Researcher (25%)
Funding/Support: No fund was received.
Article Type: Descriptive & Survey |
Subject:
Health Education and Health Behavior
Received: 2022/05/18 | Accepted: 2022/07/10 | Published: 2022/10/1
Received: 2022/05/18 | Accepted: 2022/07/10 | Published: 2022/10/1
References
1. World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. Geneva: World Health Organization; 2022 [cited 2022, 13 Apr]. Available from: https://covid19.who.int/?gclid=Cj0KCQiApY6BBhCsARIsAOI_GjYiSlIK4qboz_KSKiYnZc3SQTZHP5eQxFUmBc6XXAAjmN8M_D4tU9YaAuGrEALw_wcB. [Link]
2. Chakraborty C, Sharma AR, Bhattacharya M, Sharma G, Lee SS. The 2019 novel coronavirus disease (COVID-19) pandemic: a zoonotic prospective. Asian Pac J Trop Med. 2020;13(6):242-6. [Link] [DOI:10.4103/1995-7645.281613]
3. Taherinia M, Hassanvand A. Economic consequences of Covid-19 disease on the Iranian economy; with an emphasis on employment. Q J Nurs Manag. 2020;9(3):43-58. [Persian] [Link]
4. Thanh Le T, Andreadakis Z, Kumar A, Gomez Roman R, Tollefsen S, Saville M, Mayhew S. The COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19(5):305-6. [Link] [DOI:10.1038/d41573-020-00073-5]
5. Larson HJ, De Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Jones NS. The state of vaccine confidence 2016: Global insights through a 67-country survey. EBioMedicine. 2016;12:295-301. [Link] [DOI:10.1016/j.ebiom.2016.08.042]
6. Lane S, Macdonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF joint reporting Form data-2015-2017. Vaccine. 2018;36(26):3861-7. [Link] [DOI:10.1016/j.vaccine.2018.03.063]
7. Brien S, Kwong JC. The determinants of 2009 pandemic A/H1N1 influenza vaccination: A systematic review. Vaccine. 2012;30(7):1255-64. [Link] [DOI:10.1016/j.vaccine.2011.12.089]
8. World Health Organization. The guide to tailoring immunization programmes (TIP): Increasing coverage of infant and child vaccination in the WHO European Region [Internet]. Geneva: World Health Organization; 2014 [cited 2022, 15 Apr]. Available from: https://apps.who.int/iris/handle/10665/351166 [Link]
9. Miller JG, Hartman TK, Levita L, Martinez AP, Mason L, et al. Capability, opportunity, and motivation to enact hygienic practices in the early stages of the COVID-19 outbreak in the United Kingdom. Br J Health Psychol 2020;25(4):856-64. [Link] [DOI:10.1111/bjhp.12426]
10. Michie S, Stralen MM, West R. The behavior change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. [Link] [DOI:10.1186/1748-5908-6-42]
11. Howlett N, Schulz J, Trivedi D, Troop N, Chater A. A prospective study exploring the construct and predictive validity of the COM-B model for physical activity. J Health Psychol. 2019;24(10):1378-91. [Link] [DOI:10.1177/1359105317739098]
12. Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence- based practice: A consensus approach. Qual Saf Health Care. 2005;14(1): 26-33. [Link] [DOI:10.1136/qshc.2004.011155]
13. Atkins L, Francis J, Islam R, O'Connor D, Patey A, et al. A guide to using the Theoretical Domains Framework of behavior change to investigate implementation problems. Implement Sci. 2017;12:77-95. [Link] [DOI:10.1186/s13012-017-0605-9]
14. Cane J, O'Connor D and Michie S. Validation of the theoretical domains framework for use in behavior change and implementation research. Implement Sci. 2012;7(1): 37. [Link] [DOI:10.1186/1748-5908-7-37]
15. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225-8. [Link] [DOI:10.1038/s41591-020-1124-9]
16. Huijg JM, Gebhardt WA, Crone MR, Dusseldorp E, Presseau J. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement Sci. 2014;9:11-27. [Link] [DOI:10.1186/1748-5908-9-11]
17. West R, Michie S, Atkins L, Chadwick P. Achieving behavior change: A guide for local government and partners. London, UK: PHE publications; 2019. [Link]
18. Costello AB, Osborne JW. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1-9. [Link]
19. Galbraith-Gyan KV, Lechuga J, Jenerette CM, Palmer MH, Moore AD, Hamilton JB. HPV vaccine acceptance among African- American mothers and their daughters: an inquiry grounded in culture. Ethn Health. 2019;24(3):323-40. [Link] [DOI:10.1080/13557858.2017.1332758]
20. Gaston Godin G, Ve'zina-Im LA, Naccache H. Determinants of Influenza vaccination among healthcare workers. Infect Control Hosp Epidemiol. 2010;31(7):689-93. [Link] [DOI:10.1086/653614]
21. Dillard JP. An application of the integrative model to women's intention to be vaccinated against HPV: Implications for message design. Health Commun. 2011;26(5):479-86. [Link] [DOI:10.1080/10410236.2011.554170]
22. Cornally N, Deasy EA, McCarthy G, Moran J, Weathers E. Student nurses' intention to get the influenza vaccine. Br J Nurs. 2013;22(21):1207-11. [Link] [DOI:10.12968/bjon.2013.22.21.1207]
23. Kim SY, Seo JW, Ryu E. Korean college students' attitudes and health behaviour regarding human papillo-mavirus vaccination. 2020;28(1):57-62. [Link] [DOI:10.1016/j.colegn.2020.04.009]
24. Griffin RJ, Dunwoody S, Neuwirth K. Proposed model of the relationship of risk information seeking and processing to the development of preventive behaviors. Environ Res. 1999;80(2 Pt 2):S230-45. [Link] [DOI:10.1006/enrs.1998.3940]
25. Baron G, De wals P, Milord F. Vaccination practices of Quebec family physicians: Influenza vaccination status and professional practices for influenza vaccination. Can Fam Physician. 2001;47:2261-6. [Link]
26. Weinstein ND, Kwitel A, McCaul KD, Magnan RE, Gerrard M, Gibbons FX. Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychol. 2007;26(2):146-51. [Link] [DOI:10.1037/0278-6133.26.2.146]
27. Williams GC, Minicucci DS, Kouides RW, Levesque CS, Chirkov VI, Ryan RM, Deci EL. Self-determination, smoking, diet and health. Health Educ Res. 2002;17(5):512-21. [Link] [DOI:10.1093/her/17.5.512]
28. Nejaddadgar N, Jafarzadeh M, Ziapour A, Rezaei F. Determinants of COVID-19 Vaccine Acceptance in Ardabil: a WebBased Survey. Health Educ Health Promot. 2022;10(2):221-5. [Link]
29. Falomir-Pichastor JM, Toscani L, Despointes SH. Determinants of flu vaccination among nurses: the effect of group identification and professional responsibility. Appl Psychol Int Rev. 2009;58(1):42-58. [Link] [DOI:10.1111/j.1464-0597.2008.00381.x]
30. Nichol KL, Hauge M. Influenza vaccination of healthcare workers. Infect Control Hosp Epidemiol 1997;18(3):189-94. [Link] [DOI:10.2307/30141980]
31. LaVela SL, Smith B, Weaver FM, Legro MW, Goldstein B, Nichol K. Attitudes and practices regarding influenza vaccination among healthcare workers providing services to individuals with spinal cord injuries and disorders. Infect Control Hosp Epidemiol 2004;25(11):933-40. [Link] [DOI:10.1086/502323]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |