Volume 10, Issue 4 (2022)
Health Educ Health Promot 2022, 10(4): 727-733 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khaksar S, Shahzeydi A, Ajoodanian N, Joonbakhsh F, Sabzghabaee A, Kalhor F. Family Empowerment: Knowledge, Performance, and Attitude of Nurses and Nursing Students toward Family Education. Health Educ Health Promot 2022; 10 (4) :727-733
URL: http://hehp.modares.ac.ir/article-5-59133-en.html
URL: http://hehp.modares.ac.ir/article-5-59133-en.html
1- “Nursing and Midwifery Care Research Center” and “Department of Paediatric and Neonate Nursing, Faculty of Nursing and Midwifery”, Isfahan University of Medical Sciences, Isfahan, Iran
2- Isfahan Clinical Toxicology Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
2- Isfahan Clinical Toxicology Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Keywords: Drug Therapy [MeSH], Family Nursing [MeSH], Home Care Services [MeSH], Nurses [MeSH], Pediatrics [MeSH]
Full-Text [PDF 1024 kb]
(3649 Downloads)
| Abstract (HTML) (2041 Views)
Full-Text: (474 Views)
Introduction
The term patient education refers to formal and informal interactive activities performed by healthcare professionals that provide information, knowledge, and skills necessary to manage health and illness concerns to achieve better outcomes for patients' health [1]. Patient education is a planned learning experience using a combination of teaching methods, counseling, and behavioral modification that affect knowledge and behavior of individuals' health and illness [2]. In addition, patient education involves not only the patient specifically but also the involvement of the family and others [3].
Concerning children, those around the child, including the family and caregivers, are of particular importance. Regardless of the physical presence of parents or other family members, their influence contributes to the provision of health services because they are also central to the childcare team in addition to having the greatest and most lasting impact on children's lives [4]. Therefore, the health and well-being of children are closely associated with the physical, emotional, and social health of parents, social conditions, and parenting styles [5, 6].
In the composition of families, there is great diversity in ethnic and racial heritage, religious and spiritual orientation, how they communicate with each other, their relationships with society, their experiences, the family's ability to adapt to stress, and their attitudes toward treatment and care [7, 11]. Parents' attitudes and differences in care and treatment not only have a direct impact on how the disease is treated in childhood but can also determine behaviors related to the sustainable health of children in adulthood [12-14]. Research has shown that parents' attitudes not only affect their use of care, including medication but also have a direct effect on children's use of medication [15, 16]; therefore, parents, especially mothers, have a significant impact on health-related orientations and children's expectations concerning medication so that children's attitudes towards drug use seem to have a pattern similar to adults [17]. In this regard, there is increasing evidence to emphasize supporting families by various clinical specialties when facing serious illnesses [18, 19].
Nurses, as the majority of health care professionals at the forefront of patient care, are mainly involved in providing patients and families with educational programs and activities [20, 21]. Although nurses are often regarded as the best healthcare professionals for effective patient education, there are often uncertainties concerning their capacity to do so, with some reports of dissatisfaction with nurses' performance in patient education [22, 23]. However, most nurses believe that patient education is an essential part of their care, for which they consider themselves responsible. Unless they are unsure of their role in providing specific information, they delegate this responsibility to the physicians [24-26]. Yet, reports from several studies have shown discrepancies between the patient's educational activities that nurses accepted they had to do and what they did in reality, while there are ambiguities regarding the role of nurses in patient education [1, 27].
Nurses' failure to educate patients has often faced criticism because even if physical care is not an important nursing task, it takes precedence over patient education. While most nurses believe that patient education is a foremost priority and an important part of nursing practice, it ranks lower than other tasks, such as physical care, prescribing medications, and writing reports [28]. Various studies have investigated such ambiguities in the role of nurses in patient education [29-31]. The uncertainties about the nurses’ responsibilities, lack of time, and the insufficient number of nurses to provide education to patients are among the main reasons for their failure to participate [32, 33]. A study found that 78% of nursing staff reported not spending enough time educating patients when faced with competing demands at work [34]. Therefore, it seems that ensuring the readiness of patients and their families for discharge from the hospital is a complex and challenging task for healthcare staff that requires an understanding of many different concepts [35].
There are many influential factors on patient and family education, including patients' demographic characteristics, such as previous hospitalization history, cultural issues, language, age, personality traits, the required enhancement of self-care, and finally, learning barriers that potentially affect self-care [36]. But another important part is related to the healthcare staff, whose knowledge, skills, and perceived attitudes toward patient education affect this process. According to the evidence, nurses, as part of the healthcare team, perform most of the training and planning for patients in the hospital [37].
Healthcare staff should have a positive belief and attitude toward the effectiveness and outcomes of education for patients and their families to obtain effective education of favorable behavior to patients and families. Healthcare staff must also believe in their responsibility to provide patients and families with the required education and their capabilities to carry out such education. Conversely, in the absence of effective patient and family education, it is important to determine which variable potentially requires specific intervention to facilitate behavioral change [38].
However, there is little research on the beliefs and attitudes of nurses in the drug care phase and the importance of its family-centered approach. No study has focused on the attitudes, beliefs, knowledge, and practices of nurses and students in pediatric wards; hence, this study aimed to determine the knowledge, skills, and attitudes of nurses and nursing students concerning patient and family education in pediatric wards.
Instruments and Methods
The present descriptive-analytical study was performed in the pediatric wards of hospitals affiliated with Isfahan University of Medical Sciences over a period of 6 months in 2018-2019. The affiliated hospitals were visited by the researcher after receiving the necessary permits from the Research Center of the School of Nursing and the Ethics Committee of Isfahan University of Medical Sciences. The study sample consisted of nurses and nursing students who met the inclusion criteria. Inclusion criteria for nurses were having at least 6 months of work experience in pediatric wards regardless of employment status or shift work, working in pediatric emergency departments, pediatric internal medicine, pediatric intensive care, and surgery wards, consent to participate in the study. Inclusion criteria for students were not having clinical work experience, studying in the 7th and 8th semesters of nursing, and consent to participate in the study. Reluctance to continue the study and absence from the hospital during the study (due to annual leave or childbirth, sick leave, etc.) were considered as exclusion criteria. Based on the G-Power software, the initial sample size of 280 people was determined considering α=0.05, power=0.95 and d=0.4. The sample size of 320 people was considered due to the possibility of dropping 15% of the samples; therefore, based on the inclusion criteria, 160 nurses and 160 students were selected to participate in the study.
Study tools
The research tool was a researcher-made questionnaire, for the design of which the head nurses of the wards were initially asked to develop questions to evaluate the pharmacological knowledge of their staff in the field of family education and the items that needed teaching to families. Comments and questions were then reviewed and categorized based on scientific sources after collection. Also, 6 questions related to attitudes were designed by reviewing the texts. The opinions of 10 experts (three pediatric nursing professors, one clinical pharmacist, two pediatric medical professors, and four senior nursing experts) were used (CVR=0.8, CVI = 0.86) for formal and content validity of the 15-item questionnaire (9 knowledge questions, 6 attitude questions). Cronbach's alpha was utilized for instrument reliability with 40 samples (0.735).
The obtained questionnaire included 15 questions classified in the field of family empowerment (four statements), documentation (two statements), drug side effects (three statements), and drug safety (6 statements). The answers to the questions were in the form of a 4-point Likert scale (the correct option, I do not know, and 2 false answers). There were also 6 motivational questions with 2-choice answers and explanations if needed. The total score of the knowledge questionnaire was 100 points, according to which scores above 80, 60-80, 40-60, and less than 40 were good, acceptable, poor, and unacceptable, respectively. These statements had a qualitative and quantitative nature. The performance observation checklist also included 10 items reported as fully done, incompletely done, and did not do. The agreement coefficient of the two researchers was used for reliability (r=0.7) after performing face and content validity.
The researcher referred to selected hospitals after receiving the code of ethics from the ethics committee of Isfahan University of Medical Sciences with the ID IR.MUI.RESEARCH.REC.1398.731 and obtaining written permission from the School of Nursing and Midwifery of the Isfahan University of Medical Sciences. Then, the researcher presented the letter of introduction and explained the objectives of the research to the officials of the center to obtain their consent and cooperation. Then, the samples meeting the inclusion criteria were selected and invited to take part in the research. To comply with the ethical standards, written consent was obtained from the participants after providing them with sufficient information on the objectives and procedures of the study. Privacy and confidentiality of data were guaranteed throughout the research.
Overall, 156 nurses and 145 students completed the pharmacological knowledge questionnaire. The performance of nurses was investigated using the observation method so that an observer attended the ward for one month, observed the performance of nurses during training, and completed the performance observation checklist. The average of three observations indicated the overall score of performance.
Statistical analysis
Data were analyzed using SPSS 16 software at the alpha level of 0.05. The independent t-test and Fisher's exact test were utilized to calculate the difference between nurses and students, while analysis of variance was used for nurses in different wards. The correlation between variables was examined using the Pearson correlation test. It is noteworthy that the incomplete questionnaires were excluded from the study and were not analyzed.
Findings
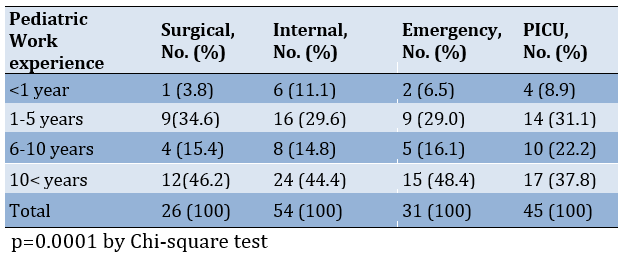
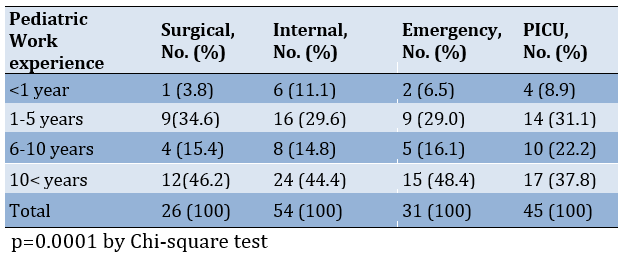
Out of 310 questionnaires distributed among employed nurses and students, 300 questionnaires were acceptable for study, including 156 nurses (52%) and 144 students (48%). There were 151 female (97.5%) and four male (2.5%) nurses, and 90 female (62%) and 55 male (48%) students. 91% of respondents had BSc, and 19% had MSc in nursing. The mean age of nurses and students participating in the study was 32.29±4.09 and 23.6±0.8 years, respectively. Out of 155 respondents, 8.3% had <1 year of work experience, and 43.8% had >10 years of experience. The mean work experience was significantly different in different wards (p=0.0001; Table 1).
Table 1) Frequency distribution of work experience in pediatric wards
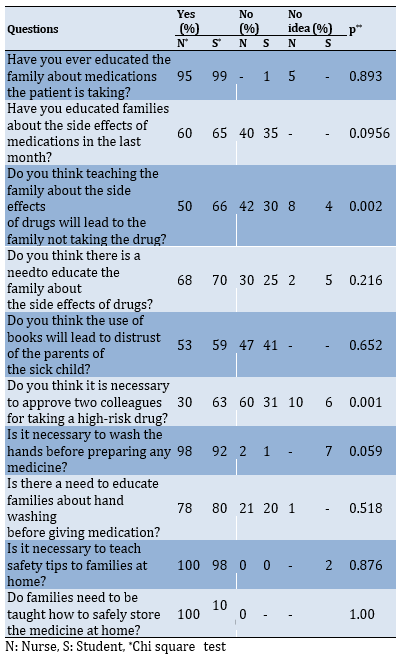
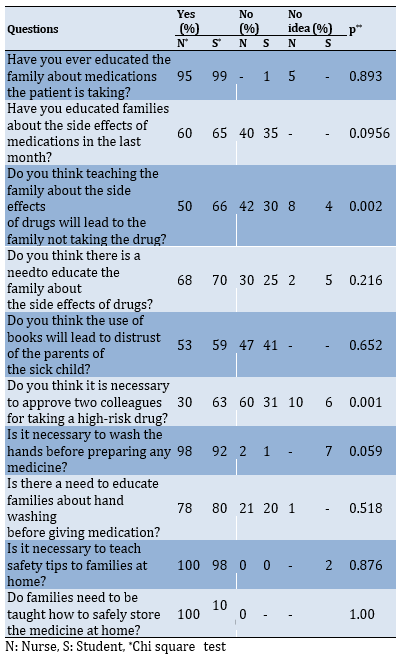
All nurses (100%) agreed with teaching home medication safety tips, but only 60% agreed with educating families about the side effects of drugs. Also, among the students, 100% agreed with teaching about home medication safety tips, while only 65% agreed with teaching families about the side effects of drugs. Another point observed among nurses and nursing students was that 50% of nurses and 44% of nursing students stated that teaching families about the side effects of medications would lead them to avoid giving medication to their children (Table 2).
Table 2) Comparison of nurses' and students' viewpoints on family education about medication
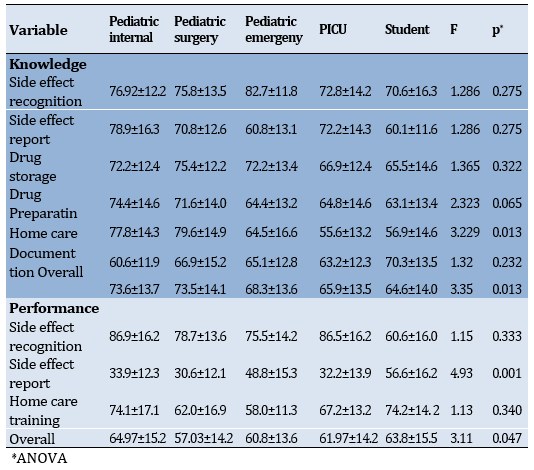
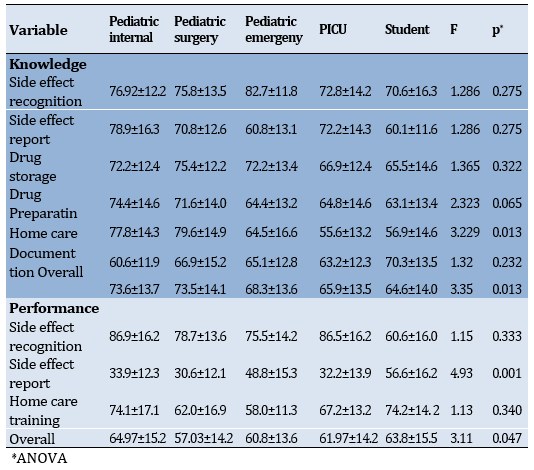
The mean score of pharmacological knowledge concerning drug side effects was 68.3±13.6, 65.9±13.5, 73.6±13.7, and 73.5±14.1 for nurses in the pediatric emergency department, pediatric intensive care unit, internal pediatric ward, and pediatric surgery ward, respectively, while it was 54.6±14 for students, indicating a statistically significant difference (p<0.05). The mean score of performance in observing the correct principles of medication was 60.8±13.6, 61.97±14.13, 64.97±15.2, and 57.03±03 for nurses in the pediatric emergency department, pediatric intensive care unit, internal pediatric ward, and pediatric surgery ward, respectively, while it was 63.8±15.5 for students, indicating a statistically significant difference (p<0.05;
Table 3).
Table 3) Comparing the mean scores of nurses' and students' knowledge and performance related to family education about medication
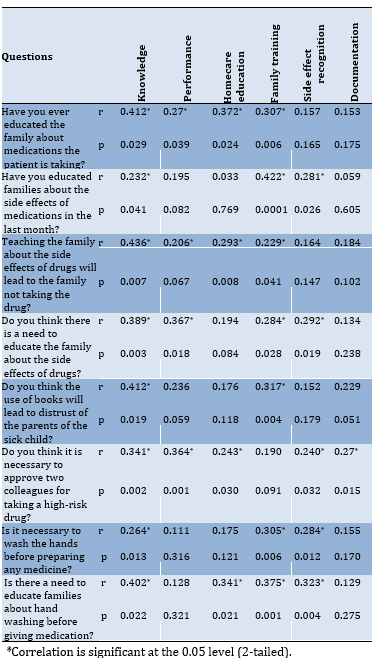
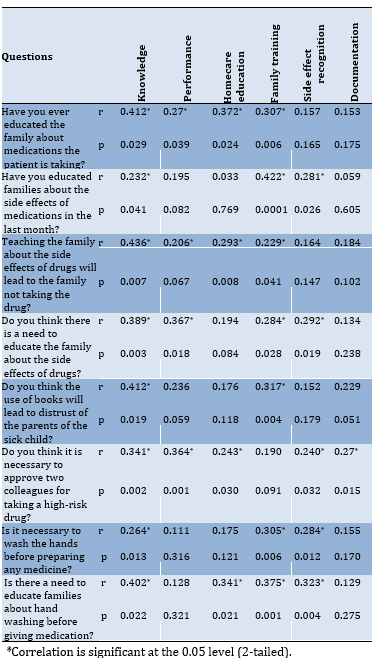
There was a significant relationship between the viewpoints of nurses and students about refusing to take drugs in case of teaching families about drug side effects and their knowledge (r=0.436; p<0.05). Also, there was a weak but significant relationship between viewpoints of nurses and students about refusing to take drugs in case of teaching families about drug side effects and their performance (r=0.206; p<0.05). There were no significant relationships between nurses' knowledge and opinions about the need for handwashing (p>0.05), but there was a significant relationship between pharmacological knowledge and handwashing education for families (r=0.406; p<0.05; Table 4).
The term patient education refers to formal and informal interactive activities performed by healthcare professionals that provide information, knowledge, and skills necessary to manage health and illness concerns to achieve better outcomes for patients' health [1]. Patient education is a planned learning experience using a combination of teaching methods, counseling, and behavioral modification that affect knowledge and behavior of individuals' health and illness [2]. In addition, patient education involves not only the patient specifically but also the involvement of the family and others [3].
Concerning children, those around the child, including the family and caregivers, are of particular importance. Regardless of the physical presence of parents or other family members, their influence contributes to the provision of health services because they are also central to the childcare team in addition to having the greatest and most lasting impact on children's lives [4]. Therefore, the health and well-being of children are closely associated with the physical, emotional, and social health of parents, social conditions, and parenting styles [5, 6].
In the composition of families, there is great diversity in ethnic and racial heritage, religious and spiritual orientation, how they communicate with each other, their relationships with society, their experiences, the family's ability to adapt to stress, and their attitudes toward treatment and care [7, 11]. Parents' attitudes and differences in care and treatment not only have a direct impact on how the disease is treated in childhood but can also determine behaviors related to the sustainable health of children in adulthood [12-14]. Research has shown that parents' attitudes not only affect their use of care, including medication but also have a direct effect on children's use of medication [15, 16]; therefore, parents, especially mothers, have a significant impact on health-related orientations and children's expectations concerning medication so that children's attitudes towards drug use seem to have a pattern similar to adults [17]. In this regard, there is increasing evidence to emphasize supporting families by various clinical specialties when facing serious illnesses [18, 19].
Nurses, as the majority of health care professionals at the forefront of patient care, are mainly involved in providing patients and families with educational programs and activities [20, 21]. Although nurses are often regarded as the best healthcare professionals for effective patient education, there are often uncertainties concerning their capacity to do so, with some reports of dissatisfaction with nurses' performance in patient education [22, 23]. However, most nurses believe that patient education is an essential part of their care, for which they consider themselves responsible. Unless they are unsure of their role in providing specific information, they delegate this responsibility to the physicians [24-26]. Yet, reports from several studies have shown discrepancies between the patient's educational activities that nurses accepted they had to do and what they did in reality, while there are ambiguities regarding the role of nurses in patient education [1, 27].
Nurses' failure to educate patients has often faced criticism because even if physical care is not an important nursing task, it takes precedence over patient education. While most nurses believe that patient education is a foremost priority and an important part of nursing practice, it ranks lower than other tasks, such as physical care, prescribing medications, and writing reports [28]. Various studies have investigated such ambiguities in the role of nurses in patient education [29-31]. The uncertainties about the nurses’ responsibilities, lack of time, and the insufficient number of nurses to provide education to patients are among the main reasons for their failure to participate [32, 33]. A study found that 78% of nursing staff reported not spending enough time educating patients when faced with competing demands at work [34]. Therefore, it seems that ensuring the readiness of patients and their families for discharge from the hospital is a complex and challenging task for healthcare staff that requires an understanding of many different concepts [35].
There are many influential factors on patient and family education, including patients' demographic characteristics, such as previous hospitalization history, cultural issues, language, age, personality traits, the required enhancement of self-care, and finally, learning barriers that potentially affect self-care [36]. But another important part is related to the healthcare staff, whose knowledge, skills, and perceived attitudes toward patient education affect this process. According to the evidence, nurses, as part of the healthcare team, perform most of the training and planning for patients in the hospital [37].
Healthcare staff should have a positive belief and attitude toward the effectiveness and outcomes of education for patients and their families to obtain effective education of favorable behavior to patients and families. Healthcare staff must also believe in their responsibility to provide patients and families with the required education and their capabilities to carry out such education. Conversely, in the absence of effective patient and family education, it is important to determine which variable potentially requires specific intervention to facilitate behavioral change [38].
However, there is little research on the beliefs and attitudes of nurses in the drug care phase and the importance of its family-centered approach. No study has focused on the attitudes, beliefs, knowledge, and practices of nurses and students in pediatric wards; hence, this study aimed to determine the knowledge, skills, and attitudes of nurses and nursing students concerning patient and family education in pediatric wards.
Instruments and Methods
The present descriptive-analytical study was performed in the pediatric wards of hospitals affiliated with Isfahan University of Medical Sciences over a period of 6 months in 2018-2019. The affiliated hospitals were visited by the researcher after receiving the necessary permits from the Research Center of the School of Nursing and the Ethics Committee of Isfahan University of Medical Sciences. The study sample consisted of nurses and nursing students who met the inclusion criteria. Inclusion criteria for nurses were having at least 6 months of work experience in pediatric wards regardless of employment status or shift work, working in pediatric emergency departments, pediatric internal medicine, pediatric intensive care, and surgery wards, consent to participate in the study. Inclusion criteria for students were not having clinical work experience, studying in the 7th and 8th semesters of nursing, and consent to participate in the study. Reluctance to continue the study and absence from the hospital during the study (due to annual leave or childbirth, sick leave, etc.) were considered as exclusion criteria. Based on the G-Power software, the initial sample size of 280 people was determined considering α=0.05, power=0.95 and d=0.4. The sample size of 320 people was considered due to the possibility of dropping 15% of the samples; therefore, based on the inclusion criteria, 160 nurses and 160 students were selected to participate in the study.
Study tools
The research tool was a researcher-made questionnaire, for the design of which the head nurses of the wards were initially asked to develop questions to evaluate the pharmacological knowledge of their staff in the field of family education and the items that needed teaching to families. Comments and questions were then reviewed and categorized based on scientific sources after collection. Also, 6 questions related to attitudes were designed by reviewing the texts. The opinions of 10 experts (three pediatric nursing professors, one clinical pharmacist, two pediatric medical professors, and four senior nursing experts) were used (CVR=0.8, CVI = 0.86) for formal and content validity of the 15-item questionnaire (9 knowledge questions, 6 attitude questions). Cronbach's alpha was utilized for instrument reliability with 40 samples (0.735).
The obtained questionnaire included 15 questions classified in the field of family empowerment (four statements), documentation (two statements), drug side effects (three statements), and drug safety (6 statements). The answers to the questions were in the form of a 4-point Likert scale (the correct option, I do not know, and 2 false answers). There were also 6 motivational questions with 2-choice answers and explanations if needed. The total score of the knowledge questionnaire was 100 points, according to which scores above 80, 60-80, 40-60, and less than 40 were good, acceptable, poor, and unacceptable, respectively. These statements had a qualitative and quantitative nature. The performance observation checklist also included 10 items reported as fully done, incompletely done, and did not do. The agreement coefficient of the two researchers was used for reliability (r=0.7) after performing face and content validity.
The researcher referred to selected hospitals after receiving the code of ethics from the ethics committee of Isfahan University of Medical Sciences with the ID IR.MUI.RESEARCH.REC.1398.731 and obtaining written permission from the School of Nursing and Midwifery of the Isfahan University of Medical Sciences. Then, the researcher presented the letter of introduction and explained the objectives of the research to the officials of the center to obtain their consent and cooperation. Then, the samples meeting the inclusion criteria were selected and invited to take part in the research. To comply with the ethical standards, written consent was obtained from the participants after providing them with sufficient information on the objectives and procedures of the study. Privacy and confidentiality of data were guaranteed throughout the research.
Overall, 156 nurses and 145 students completed the pharmacological knowledge questionnaire. The performance of nurses was investigated using the observation method so that an observer attended the ward for one month, observed the performance of nurses during training, and completed the performance observation checklist. The average of three observations indicated the overall score of performance.
Statistical analysis
Data were analyzed using SPSS 16 software at the alpha level of 0.05. The independent t-test and Fisher's exact test were utilized to calculate the difference between nurses and students, while analysis of variance was used for nurses in different wards. The correlation between variables was examined using the Pearson correlation test. It is noteworthy that the incomplete questionnaires were excluded from the study and were not analyzed.
Findings
Out of 310 questionnaires distributed among employed nurses and students, 300 questionnaires were acceptable for study, including 156 nurses (52%) and 144 students (48%). There were 151 female (97.5%) and four male (2.5%) nurses, and 90 female (62%) and 55 male (48%) students. 91% of respondents had BSc, and 19% had MSc in nursing. The mean age of nurses and students participating in the study was 32.29±4.09 and 23.6±0.8 years, respectively. Out of 155 respondents, 8.3% had <1 year of work experience, and 43.8% had >10 years of experience. The mean work experience was significantly different in different wards (p=0.0001; Table 1).
Table 1) Frequency distribution of work experience in pediatric wards
All nurses (100%) agreed with teaching home medication safety tips, but only 60% agreed with educating families about the side effects of drugs. Also, among the students, 100% agreed with teaching about home medication safety tips, while only 65% agreed with teaching families about the side effects of drugs. Another point observed among nurses and nursing students was that 50% of nurses and 44% of nursing students stated that teaching families about the side effects of medications would lead them to avoid giving medication to their children (Table 2).
Table 2) Comparison of nurses' and students' viewpoints on family education about medication
The mean score of pharmacological knowledge concerning drug side effects was 68.3±13.6, 65.9±13.5, 73.6±13.7, and 73.5±14.1 for nurses in the pediatric emergency department, pediatric intensive care unit, internal pediatric ward, and pediatric surgery ward, respectively, while it was 54.6±14 for students, indicating a statistically significant difference (p<0.05). The mean score of performance in observing the correct principles of medication was 60.8±13.6, 61.97±14.13, 64.97±15.2, and 57.03±03 for nurses in the pediatric emergency department, pediatric intensive care unit, internal pediatric ward, and pediatric surgery ward, respectively, while it was 63.8±15.5 for students, indicating a statistically significant difference (p<0.05;
Table 3).
Table 3) Comparing the mean scores of nurses' and students' knowledge and performance related to family education about medication
There was a significant relationship between the viewpoints of nurses and students about refusing to take drugs in case of teaching families about drug side effects and their knowledge (r=0.436; p<0.05). Also, there was a weak but significant relationship between viewpoints of nurses and students about refusing to take drugs in case of teaching families about drug side effects and their performance (r=0.206; p<0.05). There were no significant relationships between nurses' knowledge and opinions about the need for handwashing (p>0.05), but there was a significant relationship between pharmacological knowledge and handwashing education for families (r=0.406; p<0.05; Table 4).
Table 4) Correlation of nurses’ and students' viewpoints, knowledge, and performance concerning family education about medication
Discussion
This study aimed to determine knowledge, skills, and attitudes of nurses and nursing students concerning patient and family education in pediatric wards. The findings of this study showed that all nurses and students agreed with teaching safety issues of home medication to families, but only 60% of nurses and 65% of students agreed with teaching families about drug side effects because based on their viewpoint if the families were taught about the side effects of the drugs, they would refuse to give the medications to their children. Also, there was a significant relationship between the opinions of nurses and students concerning failure to take drugs in case of teaching about drug side effects and knowledge and drug performance.
However, in other studies, nurses referred to a lack of education as the reason for insufficient preparedness to provide information [39]. Another study pointed out the fear of being asked a question by the family and the potential inability to speak or answer adequately [40]. In another study, some argued that providing information was not their responsibility [20]. Yet, Family-Centered Care (FCC), and subsequently good communication and education can be a consistent norm in the pediatric ward and one of the needs of families that should receive priority. The presence of such issues makes nurses distance themselves from the family.
Another finding of this study was related to the nurses’ pharmacological knowledge in different wards, according to which the nurses of the internal ward had the highest pharmacological knowledge, followed by the nurses of the surgical and emergency departments. The lowest levels of pharmacological knowledge belonged to the nurses of the intensive care unit, and the students' pharmacological knowledge ranked the last. Besides, the nurses of the pediatric ward had the best performance in observing the correct principles of medication, followed by the students and nurses of the pediatric intensive care unit, the pediatric emergency department, and finally the pediatric surgery ward. Since one of the important factors in the occurrence of medication errors is related to the performance and knowledge of healthcare workers, it seems necessary to pay attention to this issue [41]. In this regard, the results of another study conducted in Iran showed moderate levels of medication awareness among nurses [42]. Another study in China [42] also provided a similar report of weakness in nurses' pharmacological knowledge. Contrary to our expectations in the present study, although the drug performance of these nurses was better than other wards, their pharmacological knowledge was lower in the Intensive Care Unit (ICU) compared to other wards. ICU nurses deal with more acute cases and face more special education, such as continuing education and more examinations to work in this ward. However, it was not reported in our study, which was also contrary to the results reported by Zyoud et al. [43].
The student's knowledge of pharmacology was at a lower level than the nurses, but they observed the principles of medicine significantly better than the nurses, probably because they remembered their training on the principles of pharmacy during the internship, while this does not apply to experienced nurses and they need in-service training [44]. Therefore, nurses and students have to receive comprehensive knowledge of pharmacology not only during nursing education at the university but also during ongoing hospital education. Besides, it is important to bridge the gap between physicians, clinical pharmacists, and nurses through effective communication because it helps reduce medication errors and improve patient care [45].
There was no significant relationship between the nurses' knowledge and opinions about the necessity of handwashing before giving medication, but there was a significant relationship between pharmacological knowledge and handwashing education for families. Concerning medication consumption, complex processes, including knowledge, attitudes, social norms, socio-economic conditions, peer pressure, experiences, and the physical and socio-behavioral environment affect human behavior; therefore, the same complex processes can be applied to handwashing behavior [46].
Given that parents have a direct impact on how children are cared for and treated, teaching sustainable health-related behaviors to patients and families is one of the most professional collaborative tasks of nurses. Also, considering that education and empowerment of families in the process of home treatment, prevention, and early detection of complications is very important, more emphasis is recommended to be placed on this issue in the training of nurses.
Research limitations
Presence at the bedside to observe performance was extremely stressful during the COVID-19 pandemic, while there was also the potential effect of the observer’s presence on individual performance, which was sought to be reduced by long-term presence. Besides, there was sample loss in the study, which was addressed by considering more samples according to the predictions.
It is suggested that the effect of family empowerment on the level of stress and anxiety, and its effect on treatment and follow-up should be investigated in future studies. Also, it seems necessary to investigate and conduct more studies on empowering families with children suffering from chronic diseases.
Conclusion
Many nurses and nursing students do not have positive attitudes towards parts of family pharmaceutical care education, including drug side effects. Also, they have low and medium knowledge and performance in teaching pharmaceutical care to families, which is related to their attitudes.
Acknowledgements: The authors would like to thank all the nurses of the selected hospitals who participated in this study. Professors and nurses contributing to the evaluation of the validity and reliability of the study tools are also appreciated.
Ethical Permission: The researcher referred to selected hospitals after receiving the code of ethics from the ethics committee of Isfahan University of Medical Sciences with the ID IR.MUI.RESEARCH.REC.1398.731 and obtaining written permission from the School of Nursing and Midwifery of the Isfahan University of Medical Sciences.
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Khaksar S. (First author), Introduction author/Original researcher/Discussion author (20%); Shahzeydi A. (Second author), Introduction author/Methodologist/Original researcher (20%); Ajoodanian N. (Third author), Introduction author/Methodologist/Original researcher (20%); Joonbakhsh F. (Fourth author), Introduction author/Methodologist/Assistant (15%); Sabzghabaee A.M. (Fifth author), Methodologist/Assistant (10%); Kalhor F. (Sixth author), Introduction author/Methodologist/Assistant/Statistical analyst (15%)
Funding: This study was done with the financial support of Isfahan Nursing and Midwifery Research Center.
Discussion
This study aimed to determine knowledge, skills, and attitudes of nurses and nursing students concerning patient and family education in pediatric wards. The findings of this study showed that all nurses and students agreed with teaching safety issues of home medication to families, but only 60% of nurses and 65% of students agreed with teaching families about drug side effects because based on their viewpoint if the families were taught about the side effects of the drugs, they would refuse to give the medications to their children. Also, there was a significant relationship between the opinions of nurses and students concerning failure to take drugs in case of teaching about drug side effects and knowledge and drug performance.
However, in other studies, nurses referred to a lack of education as the reason for insufficient preparedness to provide information [39]. Another study pointed out the fear of being asked a question by the family and the potential inability to speak or answer adequately [40]. In another study, some argued that providing information was not their responsibility [20]. Yet, Family-Centered Care (FCC), and subsequently good communication and education can be a consistent norm in the pediatric ward and one of the needs of families that should receive priority. The presence of such issues makes nurses distance themselves from the family.
Another finding of this study was related to the nurses’ pharmacological knowledge in different wards, according to which the nurses of the internal ward had the highest pharmacological knowledge, followed by the nurses of the surgical and emergency departments. The lowest levels of pharmacological knowledge belonged to the nurses of the intensive care unit, and the students' pharmacological knowledge ranked the last. Besides, the nurses of the pediatric ward had the best performance in observing the correct principles of medication, followed by the students and nurses of the pediatric intensive care unit, the pediatric emergency department, and finally the pediatric surgery ward. Since one of the important factors in the occurrence of medication errors is related to the performance and knowledge of healthcare workers, it seems necessary to pay attention to this issue [41]. In this regard, the results of another study conducted in Iran showed moderate levels of medication awareness among nurses [42]. Another study in China [42] also provided a similar report of weakness in nurses' pharmacological knowledge. Contrary to our expectations in the present study, although the drug performance of these nurses was better than other wards, their pharmacological knowledge was lower in the Intensive Care Unit (ICU) compared to other wards. ICU nurses deal with more acute cases and face more special education, such as continuing education and more examinations to work in this ward. However, it was not reported in our study, which was also contrary to the results reported by Zyoud et al. [43].
The student's knowledge of pharmacology was at a lower level than the nurses, but they observed the principles of medicine significantly better than the nurses, probably because they remembered their training on the principles of pharmacy during the internship, while this does not apply to experienced nurses and they need in-service training [44]. Therefore, nurses and students have to receive comprehensive knowledge of pharmacology not only during nursing education at the university but also during ongoing hospital education. Besides, it is important to bridge the gap between physicians, clinical pharmacists, and nurses through effective communication because it helps reduce medication errors and improve patient care [45].
There was no significant relationship between the nurses' knowledge and opinions about the necessity of handwashing before giving medication, but there was a significant relationship between pharmacological knowledge and handwashing education for families. Concerning medication consumption, complex processes, including knowledge, attitudes, social norms, socio-economic conditions, peer pressure, experiences, and the physical and socio-behavioral environment affect human behavior; therefore, the same complex processes can be applied to handwashing behavior [46].
Given that parents have a direct impact on how children are cared for and treated, teaching sustainable health-related behaviors to patients and families is one of the most professional collaborative tasks of nurses. Also, considering that education and empowerment of families in the process of home treatment, prevention, and early detection of complications is very important, more emphasis is recommended to be placed on this issue in the training of nurses.
Research limitations
Presence at the bedside to observe performance was extremely stressful during the COVID-19 pandemic, while there was also the potential effect of the observer’s presence on individual performance, which was sought to be reduced by long-term presence. Besides, there was sample loss in the study, which was addressed by considering more samples according to the predictions.
It is suggested that the effect of family empowerment on the level of stress and anxiety, and its effect on treatment and follow-up should be investigated in future studies. Also, it seems necessary to investigate and conduct more studies on empowering families with children suffering from chronic diseases.
Conclusion
Many nurses and nursing students do not have positive attitudes towards parts of family pharmaceutical care education, including drug side effects. Also, they have low and medium knowledge and performance in teaching pharmaceutical care to families, which is related to their attitudes.
Acknowledgements: The authors would like to thank all the nurses of the selected hospitals who participated in this study. Professors and nurses contributing to the evaluation of the validity and reliability of the study tools are also appreciated.
Ethical Permission: The researcher referred to selected hospitals after receiving the code of ethics from the ethics committee of Isfahan University of Medical Sciences with the ID IR.MUI.RESEARCH.REC.1398.731 and obtaining written permission from the School of Nursing and Midwifery of the Isfahan University of Medical Sciences.
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Khaksar S. (First author), Introduction author/Original researcher/Discussion author (20%); Shahzeydi A. (Second author), Introduction author/Methodologist/Original researcher (20%); Ajoodanian N. (Third author), Introduction author/Methodologist/Original researcher (20%); Joonbakhsh F. (Fourth author), Introduction author/Methodologist/Assistant (15%); Sabzghabaee A.M. (Fifth author), Methodologist/Assistant (10%); Kalhor F. (Sixth author), Introduction author/Methodologist/Assistant/Statistical analyst (15%)
Funding: This study was done with the financial support of Isfahan Nursing and Midwifery Research Center.
Article Type: Descriptive & Survey |
Subject:
Family Health Education/Promotion
Received: 2022/01/29 | Accepted: 2022/08/1 | Published: 2022/10/1
Received: 2022/01/29 | Accepted: 2022/08/1 | Published: 2022/10/1
References
1. Yeh M-Y, Wu S-C, Tung T-H. The relation between patient education, patient empowerment, and patient satisfaction: A cross-sectional-comparison study. Appl Nurs Res. 2018;39:11-7. [Link] [DOI:10.1016/j.apnr.2017.10.008]
2. Jimenez YA, Cumming S, Wang W, Stuart K, Thwaites DI, Lewis SJ. Patient education using virtual reality increases knowledge and positive experience for breast cancer patients undergoing radiation therapy. Support Care Cancer. 2018;26(8):2879-88. [Link] [DOI:10.1007/s00520-018-4114-4]
3. Finset A. Family involvement, patient engagement and benefits of patient education interventions. Patient Educ Couns. 2018;101(6):969. [Link] [DOI:10.1016/j.pec.2018.04.008]
4. Reid JL, Kagan SL, Brooks-Gunn J, Melvin SAJC, Review YS. Promoting quality in programs for infants and toddlers: Comparing the family child care and center-based teaching workforce. Child Youth Serv Rev. 2021;122:105890. [Link] [DOI:10.1016/j.childyouth.2020.105890]
5. Liaqat M, Hussain M, Afzal M, Gillani SA. Role of parents, community, and health care system in child health. J Med Physiol Biophys. 2019;62:11-5. [Link]
6. Almqvist-Tangen G, Arvidsson S, Alm B, Bergman S, Roswall J, Dahlgren J, et al. What makes parents act and react? Parental views and considerations relating to 'child health'during infancy. J Child Health Care. 2017;21(4):415-23. [Link] [DOI:10.1177/1367493517727069]
7. Behrman JA, Erman J. An exploration of differences in ideal family size between Muslim and non-Muslim women in France. Demoghraph Res. 2019;41(22):617-48. [Link] [DOI:10.4054/DemRes.2019.41.22]
8. Lee S-A. Family structure effects on student outcomes. In: Schneider B, Coleman JS, editors. Parents, their children, and schools. Routledge; 1993. p. 43-76. [Link] [DOI:10.4324/9780429498497-3]
9. Umaña‐Taylor AJ, Hill NE. Ethnic-racial socialization in the family: A decade's advance on precursors and outcomes. J Marriage Family. 2020;82(1):244-71. [Link] [DOI:10.1111/jomf.12622]
10. Gabb J, de Jong S. Focus: Families and relationships across crises. Discov Soc. 2017;44. [Link]
11. Pisula E, Porębowicz-Dörsmann A. Family functioning, parenting stress and quality of life in mothers and fathers of Polish children with high functioning autism or Asperger syndrome. PLoS One. 2017;12(10):e0186536. [Link] [DOI:10.1371/journal.pone.0186536]
12. Walsh AM, Hyde MK, Hamilton K, White KM. Predictive modelling: parents' decision making to use online child health information to increase their understanding and/or diagnose or treat their child's health. BMC Med Inform Decis Mak. 2012;12(1):144. [Link] [DOI:10.1186/1472-6947-12-144]
13. Chen J-L, Guo J, Esquivel JH, Chesla CA. Like mother, like child: the influences of maternal attitudes and behaviors on weight-related health behaviors in their children. J Transcult Nurs. 2018;29(6):523-31. [Link] [DOI:10.1177/1043659617736883]
14. Isaksson H, Koch G, Alm A, Nilsson M, Wendt L-K, Birkhed D. Parental factors in early childhood are associated with approximal caries experience in young adults-A longitudinal study. Community Dent Oral Epidemiol. 2019;47(1):49-57. [Link] [DOI:10.1111/cdoe.12421]
15. Chung H, Meuleman B. European parents' attitudes towards public childcare provision: The role of current provisions, interests and ideologies. Erou Soc. 2017;19(1):49-68. [Link] [DOI:10.1080/14616696.2016.1235218]
16. Al-Shawi MM, Darwish MA, Wahab MMA, Al-Shamlan NA. Misconceptions of parents about antibiotic use in upper respiratory tract infections: A survey in primary schools of the Eastern province, KSA. J Family Community Med. 2018;25(1):5-12. [Link]
17. Brooks M, Miller E, Abebe K, Mulvey E. The observed longitudinal relationship between future orientation and substance use among a cohort of youth with serious criminal offenses. Subst Use Misuse. 2018;53(12):1925-36. [Link] [DOI:10.1080/10826084.2018.1441311]
18. Bell JF, Whitney RL, Young HM. Family caregiving in serious illness in the United States: Recommendations to support an invisible workforce. J Am Geriart Soc. 2019;67(S2):S451-S6. [Link] [DOI:10.1111/jgs.15820]
19. Pilapil M, Coletti DJ, Rabey C, DeLaet D. Caring for the caregiver: supporting families of youth with special health care needs. Curr Probl Pediatr Adolesc Health Care. 2017;47(8):190-9. [Link] [DOI:10.1016/j.cppeds.2017.07.003]
20. Adams A, Mannix T, Harrington A. Nurses' communication with families in the intensive care unit-a literature review. Nurs Crit Care. 2017;22(2):70-80. [Link] [DOI:10.1111/nicc.12141]
21. Coster S, Watkins M, Norman I. What is the impact of professional nursing on patients' outcomes globally? An overview of research evidence. Int J Nurs Stud. 2018;78:76-83. [Link] [DOI:10.1016/j.ijnurstu.2017.10.009]
22. Karaca A, Durna Z. Patient satisfaction with the quality of nursing care. Nurs Open. 2019;6(2):535-45. [Link] [DOI:10.1002/nop2.237]
23. Fawaz MA, Hamdan-Mansour AM, Tassi A. Challenges facing nursing education in the advanced healthcare environment. Int J Afr Nurs Sci. 2018;9:105-10. [Link] [DOI:10.1016/j.ijans.2018.10.005]
24. Sherman JR. An initiative to improve patient education by clinical nurses. Med Surg Nurs. 2016;25(5):297. [Link]
25. Woo BFY, Lee JXY, Tam WWS. The impact of the advanced practice nursing role on quality of care, clinical outcomes, patient satisfaction, and cost in the emergency and critical care settings: a systematic review. Hum Resour Health. 2017;15(1):63. [Link] [DOI:10.1186/s12960-017-0237-9]
26. Matthys E, Remmen R, Van Bogaert P. An overview of systematic reviews on the collaboration between physicians and nurses and the impact on patient outcomes: what can we learn in primary care? BMC Fam Pract. 2017;18(1):110. [Link] [DOI:10.1186/s12875-017-0698-x]
27. Aiken LH, Sloane DM, Ball J, Bruyneel L, Rafferty AM, Griffiths P. Patient satisfaction with hospital care and nurses in England: an observational study. BMJ Open. 2021;8(1):e019189. [Link] [DOI:10.1136/bmjopen-2017-019189]
28. Nedjat-Haiem FR, Cadet TJ, Amatya A, Mishra SI. Healthcare providers' attitudes, knowledge, and practice behaviors for educating patients about advance directives: A national survey. Am J Hosp Palliat Care. 2019;36(5):387-95. [Link] [DOI:10.1177/1049909118813720]
29. Baummer-Carr A, Nicolau DP. The challenges of patient satisfaction: influencing factors and the patient-provider relationship in the United States. Expert Rev Anti Infect Ther. 2017;15(10):955-62. [Link] [DOI:10.1080/14787210.2017.1378097]
30. Samimi M, Safaie A, Sotoodehnia M, Rasooli F, Abdollahi A. The impact of the coordinating nurse role on patient satisfaction in the emergency department: a semi-experimental study. J Emerg Pract Truma. 2021;7(1):22-7. [Link] [DOI:10.34172/jept.2020.31]
31. Schutt RK, Woodford ML. Increasing health service access by expanding disease coverage and adding patient navigation: challenges for patient satisfaction. BMC Health Serv Res. 2020;20:175. [Link] [DOI:10.1186/s12913-020-5009-x]
32. Livne Y, Peterfreund I, Sheps J. Barriers to patient education and their relationship to nurses' perceptions of patient education climate. J Clin Nurs Stud. 2017;5(4):65. [Link] [DOI:10.5430/cns.v5n4p65]
33. Jung MJ, Roh YS. Factors influencing the patient education performance of hemodialysis unit nurses. Patient Educ Couns. 2020;S0738-3991(20):30328-1. [Link]
34. Fajriyanti LA, Nurmala I, Hargono R. The Phenomenon of patient health education by nurses in hospital. Ind J Public Health Res Dev. 2020;11(3):1605-9. [Link]
35. John IJS, Englund HM. Improving Patient discharge education through daily educational bursts: A pilot study. J Nurses Prof Dev. 2020;36(5):283-7. [Link] [DOI:10.1097/NND.0000000000000627]
36. Weinberger SE, Johnson BH, Ness DL. Patient-and family-centered medical education: the next revolution in medical education? Ann Intern Med. 2014;161(1):73-5. [Link] [DOI:10.7326/M13-2993]
37. Smith JA, Zsohar H. Patient-education tips for new nurses. Nursing. 2013;43(10):1-3. [Link] [DOI:10.1097/01.NURSE.0000434224.51627.8a]
38. Shivnan JC, Kennedy MM. The nurse in the modern hospital. In: Latifi E, editore. The modern hospital. Springer; 2019. p. 341-56. [Link] [DOI:10.1007/978-3-030-01394-3_32]
39. Wittenberg E, Reb A, Kanter E. Communicating with patients and families around difficult topics in cancer care using the COMFORT communication curriculum. Semin Oncol Nurs. 2018;34(3):264-73. [Link] [DOI:10.1016/j.soncn.2018.06.007]
40. Loghmani L, Borhani F, Abbasszadeh A. Determination of the content of communication between the care team and family members of patients in the intensive care unit: The experience of nurses and patients' families. J Qual Res Health Sci. 2020;3(3):257-68. [Persian] [Link]
41. Gajdács M, Paulik E, Szabó A. Knowledge, attitude and practice of community pharmacists regarding antibiotic use and infectious diseases: a cross-sectional survey in Hungary (KAPPhA-HU). Antibiotics (Basel). 2020;9(2):41. [Link] [DOI:10.3390/antibiotics9020041]
42. Ashtiani F, Hadavand N, Momeni B, Ansarifar A. Evaluation of knowledge of pharmacology among nurses at Rajaie Heart Hospital and its position in care ethics. Iran J Biomed Law Ethics. 2019;1(1):36-46. [Persian] [Link]
43. Zyoud SH, Khaled SM, Kawasmi BM, Habeba AM, Hamadneh AT, Anabosi HH, et al. Knowledge about the administration and regulation of high alert medications among nurses in Palestine: a cross-sectional study. BMC Nurs. 2019;18:11. [Link] [DOI:10.1186/s12912-019-0336-0]
44. Khajeali N, Baghaei R. Comparison of pharmacological knowledge and skills in pharmaceutical calculations in nurses of general and ICU wards in educational hospitals in Ahvaz. Q J Nurs Manag. 2014;2(4):48-55. [Persian] [Link]
45. Salman M, Mustafa ZU, Rao AZ, Khan Q-u-A, Asif N, Hussain K, et al. Serious inadequacies in high alert medication-related knowledge among Pakistani nurses: Findings of a large, multicenter, cross-sectional survey. Front Pharmacol. 2020;11:1026. [Link] [DOI:10.3389/fphar.2020.01026]
46. Diwan V, Gustafsson C, Rosales Klintz S, Joshi SC, Joshi R, Sharma M, et al. Understanding healthcare workers self-reported practices, knowledge and attitude about hand hygiene in a medical setting in rural India. PLoS One. 2016;11(10):e0163347. [Link] [DOI:10.1371/journal.pone.0163347]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





