Volume 10, Issue 2 (2022)
Health Educ Health Promot 2022, 10(2): 315-321 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Omid M, Aminshokravi F, Zarei F. Design and Psychometrics of a Questionnaire on COVID-19 Preventive Behaviors Evaluation based on Health Behavior Model. Health Educ Health Promot 2022; 10 (2) :315-321
URL: http://hehp.modares.ac.ir/article-5-58318-en.html
URL: http://hehp.modares.ac.ir/article-5-58318-en.html
1- Department of Health Education and Health Promotion, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
Keywords: Behavior [MeSH], COVID-19 [MeSH], Health Belief Model [MeSH], Prevention [MeSH], Psychometrics [MeSH], Questionnaire [MeSH]
Full-Text [PDF 470 kb]
(919 Downloads)
| Abstract (HTML) (723 Views)
Full-Text: (170 Views)
Introduction
An outbreak of an unexplained respiratory infection was first reported in Wuhan, China, on December 31st, 2019, to the World Health Organization. The causative agent of the disease has been attributed to a new virus belonging to the coronavirus family, which causes diseases ranging from the common cold to more severe illnesses that lead to death [1].
On February 11th, 2020, the World Health Organization announced that the disease caused by the new coronavirus is called COVID-19, which stands for ‘Coronavirus 2019’. On the same day, the International Committee for the Classification of Viruses named the virus SARS-CoV-2, originally called nCoV 2019 [2].
In the past 20 years, two other coronavirus epidemics have occurred. The SARS epidemic, which began in China and affected 29 countries and caused more than 8,000 cases and more than 800 deaths (9.6% mortality rate), and the MERS epidemic, which began in Saudi Arabia and caused about 2,500 cases and 800 deaths (35% mortality rate) [3, 4]. Despite the higher mortality rate of SARS and MERS, due to the high number of COVID-19 patients, the total number of deaths due to this disease was higher [5].
Since the beginning of 2020, the new coronavirus has spread rapidly around the world [1]. According to the latest statistics, more than 202 million cases and more than 4 million deaths due to COVID-19 have been reported worldwide [6]. In the Eastern Mediterranean region, Iran had the highest COVID-19 incidence and mortality [7-9]. On February 19th, 2020, the first case of death from COVID-19 was reported in Iran, and the disease rapidly spread across the country [10, 11].
The incubation period of COVID-19 is between 2 and 14 days [12]. The most common clinical symptoms of COVID-19 are fever, cough, muscle aches, sputum, shortness of breath, sore throat, headache, diarrhea, nausea or vomiting, loss of sense of smell and taste, nasal congestion, and bloody sputum [13, 14]. More than 80% of COVID-19 patients experience a mild illness and 20% of them experience severe illness and suffer from shortness of breath, septic shock, and failure of various organs of the body [15]. The main routes of transmission of the novel coronavirus are inhalation of respiratory droplets from an infected person and close contact with the infected person or their secretions [16]. Given the lack of medications and universal vaccination in society, prevention is the best way to reduce the number of cases of disease [17]. COVID-19 preventive behaviors include using a mask, frequent hand-washing with soap and water, covering the mouth and nose with a handkerchief when coughing and sneezing, avoiding contact with the eyes, mouth, and nose with a dirty hand, avoiding close contact with affected people and social distancing [18-20].
Due to the importance of COVID-19 preventive behaviors, the availability of a specific and standard tool is necessary to conduct the study. Health Belief Model is one of the suitable models to teach preventive behaviors. The Health belief model emphasizes how a person's perception causes an Increase motivation to adopt preventive behaviors [21]. HBM is widely used to comprehensively understand people's health-related behaviors, plays an important role in predicting preventive measures compliance, and has been used in many previous studies [22, 23]. According to the Health Belief Model (HBM), people react appropriately to disease prevention when they believe they are at risk (perceived susceptibility) and that the risk is serious to them (perceived severity). Also, when they feel that behavior change has many benefits for them (perceived benefits) and they can remove the obstacles to performing the recommended behavior (perceived barriers), they are more likely to engage in that behavior. Self-efficacy is likewise the belief in one's ability to perform the recommended behavior. Cues to action are internal and external stimuli that lead a person to perform healthy behaviors.
In their search, the research team did not find a specific tool based on the HBM measuring knowledge, beliefs, and behavior of individuals regarding COVID-19. Therefore, this study aimed to design and psychometric a tool for measuring the knowledge, beliefs, and behavior of teachers regarding COVID-19 preventive behaviors.
Instrument and Methods
To develop and psychometric an instrument to assess the COVID-19 preventive behaviors of Iranian teachers, the items required in this study were extracted from other COVID-19 tools available in the world, and a literature review of relevant texts measuring knowledge, attitude, and practice in individuals with regards to COVID-19, based on the HBM model and concerning two main following stages had been done: Development of the questionnaire, and Psychometric characteristics of the questionnaire.
Development of the questionnaire
Conceptual framework and Item generation
Due to the high incidence and mortality of COVID-19 in Iran and the lack of specific treatment for it, it seems to be necessary to promote knowledge, attitudes, and preventive behaviors toward the disease. Because of relationships with many students, and playing an effective role in them and their parents' attitudes, it seems essential to consider the health of teachers and their health behaviors. Promoting COVID-19 preventive behaviors based on theoretical frameworks of behavior change can be useful. The review of the literature suggests that the Health Belief Model may be effective in promoting COVID-19 preventive behaviors. The Health Belief Model was one of the first theories to be developed exclusively for health-related behaviors.
Contextual item generation based on HBM constructs
Items of the questionnaire were generated through the deductive-inductive approach. This approach helps to find appropriate items based on literature review and World Health Organization and CDC guidelines. This combination resulted in a 101-item draft scale designed on concept labels that accurately reflected the content of each dimension.
Psychometric properties of the questionnaire
In this stage, the psychometric properties of the developed instrument were assessed.
The current instrument consists of four parts;
-A demographic information including gender, age, educational status, Marital status, and history of COVID-19 infection.
-Assessment of teacher’s knowledge regarding COVID-19: This part of the questionnaire aimed to assess knowledge. It contains 10 questions including COVID-19 signs and symptoms, mode of transmission, and prevention. knowledge questions were weighed with three options: "True", "False" and "I do not know".
-Health belief model structures: This part of the questionnaire was developed to examine perceived susceptibility (8 items), perceived severity (5 items), perceived benefits (5 items), perceived barriers (6 items), cues to action (4 items) and self-efficacy (11 items). Responses for each item ranged from "strongly disagree" to "strongly agree".
-COVID-19 preventive behaviors: This part of the questionnaire aimed to assess COVID-19 preventive behaviors. It contains 11 items with response ranging from "never" to "always". It contains 11 items.The scale’s score ranges from 50 to 270.
The face validity of an index was used to determine if it is a reasonable measure of word order, structure order, and evaluation form [24]. In contrast, content validity is used to assess the relevance, clarity, simplicity, and completeness of the tool [25]. Fifteen people including health education specialists (N=12) and health care providers (N=3) as experts on issues related to COVID-19 prevention were asked to review the initial draft of the instrument. Both quantitatively and qualitatively content validity was assessed. They were asked to present their corrective views in writing after carefully studying the items and their final opinion was received and analyzed through a qualitative approach. It was also emphasized that the qualitative evaluation of content validity in terms of grammar criteria should assess the use of appropriate words and the necessity, importance, and placement of phrases in their proper places. After collecting the experts’ opinions, the necessary changes were applied to the questionnaire. Content Validity Ratio (CVR) and Content Validity Index (CVI) were used to evaluate the content validity quantitatively. In calculating the CVR, experts were asked to choose one of the options “necessary”, “not necessary but useful” and “not necessary” for the items in each of the scales. Responses were calculated using the following formula and adapted to the Lawshe table. According to this table, items with a CVR above 0.49 were considered acceptable.
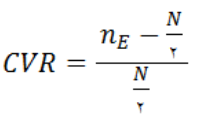
nE: The number of experts by whom the “necessary” option was selected.
N: Total number of experts (panel members)
The Waltz and Basel index was used to evaluate the validity index. For this purpose, scales were presented to the experts to calculate the CVI and they were asked to comment on each of the items with the following three criteria based on the quadratic Likert scale (1: irrelevant, 2: somewhat relevant, 3: relevant, and 4: completely relevant): relevance, simplicity, and clarity. To calculate CVI scores, the total number of “agreeing” scores for each item that scored 3 or 4 (highest score) was calculated for the total number of voters. The minimum acceptable value for the CVI index was 0.8 and if the CVI index for an item was less than 0.7, that item was removed and if it was between 0.7 and 0.79, it was corrected.
Cronbach's alpha was used to evaluate the reliability (internal correlation) [26]. And intra-cluster homogeneity of the questionnaire based on the ICC coefficient was calculated. If ICC (Intraclass coefficient correlation) values are 0.8 or higher, there is excellent reliability; if it is between 0.6 and 0.79, there is moderate reliability, and if it is less than 0.6, there is poor reliability [27]. To evaluate the reliability of the scale at test-retest, which indicates the reproducibility of an index, the questionnaire was given to 30 people with similar characteristics in the target group. Ten days later, they were asked to complete the questionnaire again.
Findings
The mean age of participants was 39.11±9.76 years. The demographic characteristics of the target group were presented in Table 1.
Table 1) Demographic characteristics of the target group
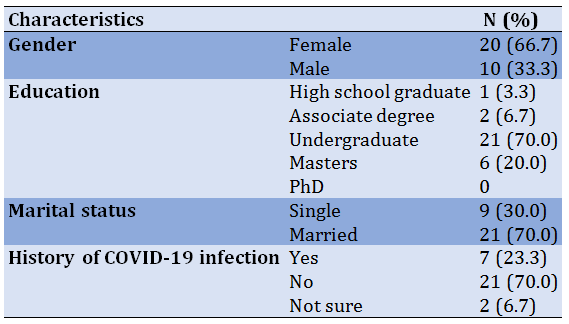
Table 2) Final questionnaire with Content Validity Ratio and Content Validity Index scores
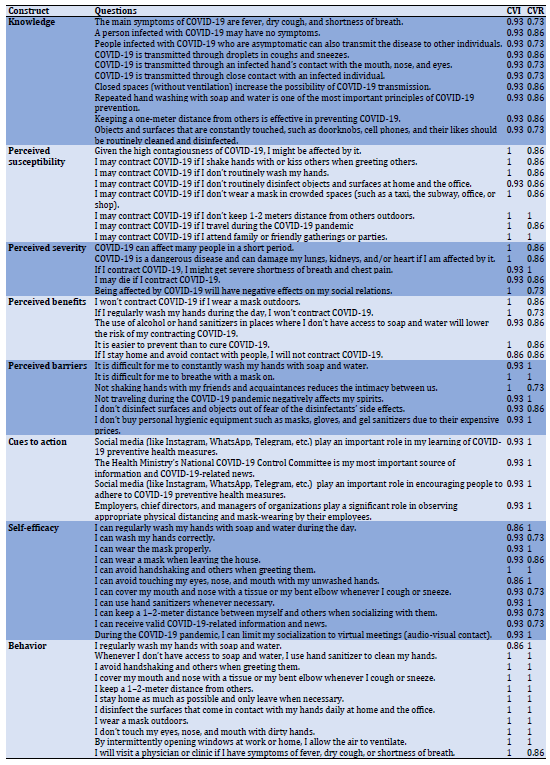
The results of the validity ratio for all items except 4 items were larger than the number specified in the standard Lawshe table (0.49). This suggests that essential and relevant items were present in this tool. The results of the content validity index showed that all items except one item scored higher than 0.79 (Table 2).
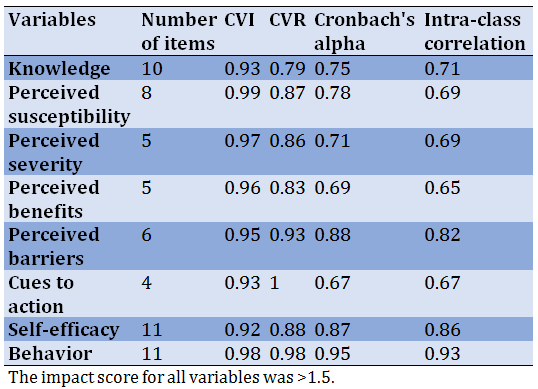
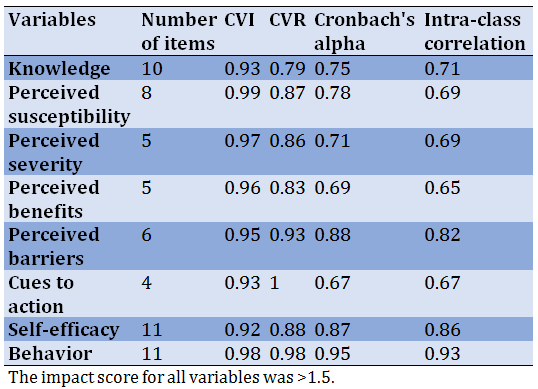
Upon assessing the reliability of items on the perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavior scales, Cronbach's alpha ranged from 0.669 to 0.950 and ICC ranged between 0.652 and 0.938 (Table 3).
Table 3) Average values of validity and reliability indices of items in each scale
Discussion
Based on our results, the psychometric evaluation of the COVID-19 prevention scales showed good content validity, such that the average validity index for all items of the eight scales of knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy and behavior was higher than 0.93 and its average validity ratio was calculated above 0.72.
Upon assessing the reliability of items in the knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavior scales, the degree of internal correlation (Cronbach's alpha coefficient) was, respectively, 0.75, 0.78, 0.71, 0.69, 0.88, 0.67, 0.87, and 0.95. The measurement tool in Tong et al.’s 2020 study contains 24 items. In this tool, only one item was used for perceived susceptibility, and Cronbach's alpha for perceived severity, perceived benefits, perceived barriers, and cues to action was reported at 0.79, 0.89, 0.74, and 0.68, respectively [28]. Fathian-Dastgerdi et al. conducted a study to assess adolescents' perceptions of COVID-19 preventive behaviors based on the Health Belief Model. They designed 4, 4, 4, 4, 3, 2, and 5 questions for perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and behavior, respectively, and reported Cronbach's alpha for these scales at 0.66, 0.74, 0.71, 0.72, 0.58, and 0.82, respectively [29]. In a study aimed at measuring the predictive power of the HBM for COVID-19 preventive behaviors regarding perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, cues to action and behavior, 4, 9, 9, 4, 7, 6 and 20 questions were considered, respectively. Cronbach's alpha for perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and behavior scales in this study was reported at 0.79, 0. 87, 0.84, 0.66, 0.92, and 0.91, respectively [30]. In a study to measure ophthalmologists' perception of COVID-19 using the Health Belief Model for perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, cues to action and behavior, 9, 5, 4, 5, 4, 5 and 8 questions were designed and Cronbach's alpha for these scales was reported at 0.78, 0.69, 0.73, 0.76, 0.71, 0.67, and 0.79, respectively [31].
The results of the abovementioned studies are consistent with the findings of the present study and in all three studies, the reliability of the ‘cues to action’ construct was lower than the others. This could be due to receiving information from various sources to prevent COVID-19. The audience may also be exposed to pseudo-knowledge about COVID-19 preventive behaviors.
Tong et al.’s questionnaire was not designed for knowledge, self-efficacy, and behavior scales [28]. In Fathian-Dastgerdi et al.’s questionnaire, there were no questions on knowledge and ‘cues to action’ scales [29]. Similarly, the questionnaires designed by Mirzaei et al. [30] and Almazyad EM et al. [31] had no knowledge scale questions.
Therefore, it was necessary to design a valid and reliable questionnaire that covered all these scales. The psychometric instrument designed in the present study has considered all the constructs of the Health Belief Model, although some constructs, such as self-efficacy, behavior [28], and cues to action [29] have not been assessed in similar studies.
Comparing the results of this study with other tools based on the Health Belief Model that are designed for COVID-19 preventive behaviors indicated that the Cronbach alpha values obtained for the scales used in the present tool were lower in some cases and higher in some others compared to those calculated for those tools.
Conclusion
In the present study, the tool "Measuring COVID-19 Preventive Behaviors" was developed to assess knowledge, Health Belief Model constructs, and behavior. During this psychometric study, the content validity, content reliability, and internal correlation of the tool were calculated. The COVID-19 Preventive Behaviors tool is an objective tool for assessing knowledge, Health Belief Model constructs, and behavior. It is also a suitable tool for research in educational fields.
Acknowledgments: We would like to thank the supervisors, consultants, and the Education Department staff of District 4, Karaj, who participated in this research.
Ethical Permissions: The present study is the result of a research project with the ethical code IR.MODARES.REC.1399.182.
Conflicts of Interests: This article is part of a research dissertation for Tarbiat Modares University in the field of Health Education and Promotion.
Authors’ Contributions: Omid M (First author), Main researcher (50%); Aminshokravi F (Second author), Assistant researcher (25%); Zarei F (Third author), Methodologist (25%)
Funding/Support: This work was supported by Tarbiat Modares University.
An outbreak of an unexplained respiratory infection was first reported in Wuhan, China, on December 31st, 2019, to the World Health Organization. The causative agent of the disease has been attributed to a new virus belonging to the coronavirus family, which causes diseases ranging from the common cold to more severe illnesses that lead to death [1].
On February 11th, 2020, the World Health Organization announced that the disease caused by the new coronavirus is called COVID-19, which stands for ‘Coronavirus 2019’. On the same day, the International Committee for the Classification of Viruses named the virus SARS-CoV-2, originally called nCoV 2019 [2].
In the past 20 years, two other coronavirus epidemics have occurred. The SARS epidemic, which began in China and affected 29 countries and caused more than 8,000 cases and more than 800 deaths (9.6% mortality rate), and the MERS epidemic, which began in Saudi Arabia and caused about 2,500 cases and 800 deaths (35% mortality rate) [3, 4]. Despite the higher mortality rate of SARS and MERS, due to the high number of COVID-19 patients, the total number of deaths due to this disease was higher [5].
Since the beginning of 2020, the new coronavirus has spread rapidly around the world [1]. According to the latest statistics, more than 202 million cases and more than 4 million deaths due to COVID-19 have been reported worldwide [6]. In the Eastern Mediterranean region, Iran had the highest COVID-19 incidence and mortality [7-9]. On February 19th, 2020, the first case of death from COVID-19 was reported in Iran, and the disease rapidly spread across the country [10, 11].
The incubation period of COVID-19 is between 2 and 14 days [12]. The most common clinical symptoms of COVID-19 are fever, cough, muscle aches, sputum, shortness of breath, sore throat, headache, diarrhea, nausea or vomiting, loss of sense of smell and taste, nasal congestion, and bloody sputum [13, 14]. More than 80% of COVID-19 patients experience a mild illness and 20% of them experience severe illness and suffer from shortness of breath, septic shock, and failure of various organs of the body [15]. The main routes of transmission of the novel coronavirus are inhalation of respiratory droplets from an infected person and close contact with the infected person or their secretions [16]. Given the lack of medications and universal vaccination in society, prevention is the best way to reduce the number of cases of disease [17]. COVID-19 preventive behaviors include using a mask, frequent hand-washing with soap and water, covering the mouth and nose with a handkerchief when coughing and sneezing, avoiding contact with the eyes, mouth, and nose with a dirty hand, avoiding close contact with affected people and social distancing [18-20].
Due to the importance of COVID-19 preventive behaviors, the availability of a specific and standard tool is necessary to conduct the study. Health Belief Model is one of the suitable models to teach preventive behaviors. The Health belief model emphasizes how a person's perception causes an Increase motivation to adopt preventive behaviors [21]. HBM is widely used to comprehensively understand people's health-related behaviors, plays an important role in predicting preventive measures compliance, and has been used in many previous studies [22, 23]. According to the Health Belief Model (HBM), people react appropriately to disease prevention when they believe they are at risk (perceived susceptibility) and that the risk is serious to them (perceived severity). Also, when they feel that behavior change has many benefits for them (perceived benefits) and they can remove the obstacles to performing the recommended behavior (perceived barriers), they are more likely to engage in that behavior. Self-efficacy is likewise the belief in one's ability to perform the recommended behavior. Cues to action are internal and external stimuli that lead a person to perform healthy behaviors.
In their search, the research team did not find a specific tool based on the HBM measuring knowledge, beliefs, and behavior of individuals regarding COVID-19. Therefore, this study aimed to design and psychometric a tool for measuring the knowledge, beliefs, and behavior of teachers regarding COVID-19 preventive behaviors.
Instrument and Methods
To develop and psychometric an instrument to assess the COVID-19 preventive behaviors of Iranian teachers, the items required in this study were extracted from other COVID-19 tools available in the world, and a literature review of relevant texts measuring knowledge, attitude, and practice in individuals with regards to COVID-19, based on the HBM model and concerning two main following stages had been done: Development of the questionnaire, and Psychometric characteristics of the questionnaire.
Development of the questionnaire
Conceptual framework and Item generation
Due to the high incidence and mortality of COVID-19 in Iran and the lack of specific treatment for it, it seems to be necessary to promote knowledge, attitudes, and preventive behaviors toward the disease. Because of relationships with many students, and playing an effective role in them and their parents' attitudes, it seems essential to consider the health of teachers and their health behaviors. Promoting COVID-19 preventive behaviors based on theoretical frameworks of behavior change can be useful. The review of the literature suggests that the Health Belief Model may be effective in promoting COVID-19 preventive behaviors. The Health Belief Model was one of the first theories to be developed exclusively for health-related behaviors.
Contextual item generation based on HBM constructs
Items of the questionnaire were generated through the deductive-inductive approach. This approach helps to find appropriate items based on literature review and World Health Organization and CDC guidelines. This combination resulted in a 101-item draft scale designed on concept labels that accurately reflected the content of each dimension.
Psychometric properties of the questionnaire
In this stage, the psychometric properties of the developed instrument were assessed.
The current instrument consists of four parts;
-A demographic information including gender, age, educational status, Marital status, and history of COVID-19 infection.
-Assessment of teacher’s knowledge regarding COVID-19: This part of the questionnaire aimed to assess knowledge. It contains 10 questions including COVID-19 signs and symptoms, mode of transmission, and prevention. knowledge questions were weighed with three options: "True", "False" and "I do not know".
-Health belief model structures: This part of the questionnaire was developed to examine perceived susceptibility (8 items), perceived severity (5 items), perceived benefits (5 items), perceived barriers (6 items), cues to action (4 items) and self-efficacy (11 items). Responses for each item ranged from "strongly disagree" to "strongly agree".
-COVID-19 preventive behaviors: This part of the questionnaire aimed to assess COVID-19 preventive behaviors. It contains 11 items with response ranging from "never" to "always". It contains 11 items.The scale’s score ranges from 50 to 270.
The face validity of an index was used to determine if it is a reasonable measure of word order, structure order, and evaluation form [24]. In contrast, content validity is used to assess the relevance, clarity, simplicity, and completeness of the tool [25]. Fifteen people including health education specialists (N=12) and health care providers (N=3) as experts on issues related to COVID-19 prevention were asked to review the initial draft of the instrument. Both quantitatively and qualitatively content validity was assessed. They were asked to present their corrective views in writing after carefully studying the items and their final opinion was received and analyzed through a qualitative approach. It was also emphasized that the qualitative evaluation of content validity in terms of grammar criteria should assess the use of appropriate words and the necessity, importance, and placement of phrases in their proper places. After collecting the experts’ opinions, the necessary changes were applied to the questionnaire. Content Validity Ratio (CVR) and Content Validity Index (CVI) were used to evaluate the content validity quantitatively. In calculating the CVR, experts were asked to choose one of the options “necessary”, “not necessary but useful” and “not necessary” for the items in each of the scales. Responses were calculated using the following formula and adapted to the Lawshe table. According to this table, items with a CVR above 0.49 were considered acceptable.
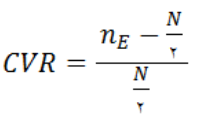
nE: The number of experts by whom the “necessary” option was selected.
N: Total number of experts (panel members)
The Waltz and Basel index was used to evaluate the validity index. For this purpose, scales were presented to the experts to calculate the CVI and they were asked to comment on each of the items with the following three criteria based on the quadratic Likert scale (1: irrelevant, 2: somewhat relevant, 3: relevant, and 4: completely relevant): relevance, simplicity, and clarity. To calculate CVI scores, the total number of “agreeing” scores for each item that scored 3 or 4 (highest score) was calculated for the total number of voters. The minimum acceptable value for the CVI index was 0.8 and if the CVI index for an item was less than 0.7, that item was removed and if it was between 0.7 and 0.79, it was corrected.
Cronbach's alpha was used to evaluate the reliability (internal correlation) [26]. And intra-cluster homogeneity of the questionnaire based on the ICC coefficient was calculated. If ICC (Intraclass coefficient correlation) values are 0.8 or higher, there is excellent reliability; if it is between 0.6 and 0.79, there is moderate reliability, and if it is less than 0.6, there is poor reliability [27]. To evaluate the reliability of the scale at test-retest, which indicates the reproducibility of an index, the questionnaire was given to 30 people with similar characteristics in the target group. Ten days later, they were asked to complete the questionnaire again.
Findings
The mean age of participants was 39.11±9.76 years. The demographic characteristics of the target group were presented in Table 1.
Table 1) Demographic characteristics of the target group
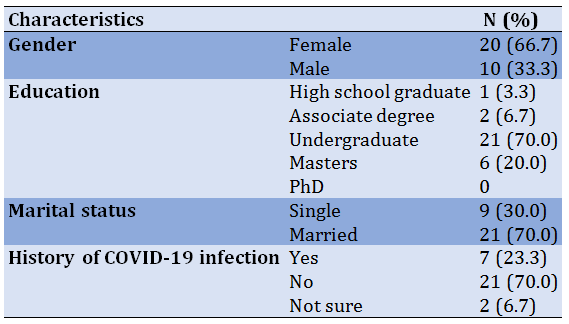
Table 2) Final questionnaire with Content Validity Ratio and Content Validity Index scores
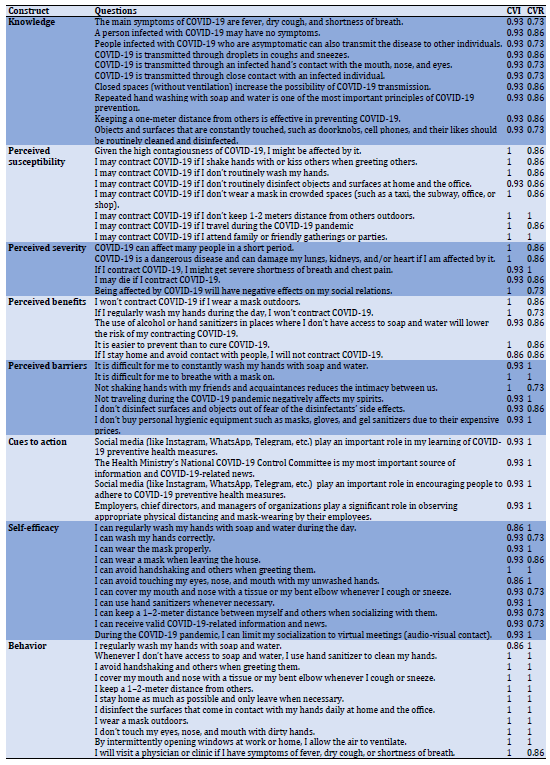
The results of the validity ratio for all items except 4 items were larger than the number specified in the standard Lawshe table (0.49). This suggests that essential and relevant items were present in this tool. The results of the content validity index showed that all items except one item scored higher than 0.79 (Table 2).
Upon assessing the reliability of items on the perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavior scales, Cronbach's alpha ranged from 0.669 to 0.950 and ICC ranged between 0.652 and 0.938 (Table 3).
Table 3) Average values of validity and reliability indices of items in each scale
Discussion
Based on our results, the psychometric evaluation of the COVID-19 prevention scales showed good content validity, such that the average validity index for all items of the eight scales of knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy and behavior was higher than 0.93 and its average validity ratio was calculated above 0.72.
Upon assessing the reliability of items in the knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavior scales, the degree of internal correlation (Cronbach's alpha coefficient) was, respectively, 0.75, 0.78, 0.71, 0.69, 0.88, 0.67, 0.87, and 0.95. The measurement tool in Tong et al.’s 2020 study contains 24 items. In this tool, only one item was used for perceived susceptibility, and Cronbach's alpha for perceived severity, perceived benefits, perceived barriers, and cues to action was reported at 0.79, 0.89, 0.74, and 0.68, respectively [28]. Fathian-Dastgerdi et al. conducted a study to assess adolescents' perceptions of COVID-19 preventive behaviors based on the Health Belief Model. They designed 4, 4, 4, 4, 3, 2, and 5 questions for perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and behavior, respectively, and reported Cronbach's alpha for these scales at 0.66, 0.74, 0.71, 0.72, 0.58, and 0.82, respectively [29]. In a study aimed at measuring the predictive power of the HBM for COVID-19 preventive behaviors regarding perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, cues to action and behavior, 4, 9, 9, 4, 7, 6 and 20 questions were considered, respectively. Cronbach's alpha for perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and behavior scales in this study was reported at 0.79, 0. 87, 0.84, 0.66, 0.92, and 0.91, respectively [30]. In a study to measure ophthalmologists' perception of COVID-19 using the Health Belief Model for perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, cues to action and behavior, 9, 5, 4, 5, 4, 5 and 8 questions were designed and Cronbach's alpha for these scales was reported at 0.78, 0.69, 0.73, 0.76, 0.71, 0.67, and 0.79, respectively [31].
The results of the abovementioned studies are consistent with the findings of the present study and in all three studies, the reliability of the ‘cues to action’ construct was lower than the others. This could be due to receiving information from various sources to prevent COVID-19. The audience may also be exposed to pseudo-knowledge about COVID-19 preventive behaviors.
Tong et al.’s questionnaire was not designed for knowledge, self-efficacy, and behavior scales [28]. In Fathian-Dastgerdi et al.’s questionnaire, there were no questions on knowledge and ‘cues to action’ scales [29]. Similarly, the questionnaires designed by Mirzaei et al. [30] and Almazyad EM et al. [31] had no knowledge scale questions.
Therefore, it was necessary to design a valid and reliable questionnaire that covered all these scales. The psychometric instrument designed in the present study has considered all the constructs of the Health Belief Model, although some constructs, such as self-efficacy, behavior [28], and cues to action [29] have not been assessed in similar studies.
Comparing the results of this study with other tools based on the Health Belief Model that are designed for COVID-19 preventive behaviors indicated that the Cronbach alpha values obtained for the scales used in the present tool were lower in some cases and higher in some others compared to those calculated for those tools.
Conclusion
In the present study, the tool "Measuring COVID-19 Preventive Behaviors" was developed to assess knowledge, Health Belief Model constructs, and behavior. During this psychometric study, the content validity, content reliability, and internal correlation of the tool were calculated. The COVID-19 Preventive Behaviors tool is an objective tool for assessing knowledge, Health Belief Model constructs, and behavior. It is also a suitable tool for research in educational fields.
Acknowledgments: We would like to thank the supervisors, consultants, and the Education Department staff of District 4, Karaj, who participated in this research.
Ethical Permissions: The present study is the result of a research project with the ethical code IR.MODARES.REC.1399.182.
Conflicts of Interests: This article is part of a research dissertation for Tarbiat Modares University in the field of Health Education and Promotion.
Authors’ Contributions: Omid M (First author), Main researcher (50%); Aminshokravi F (Second author), Assistant researcher (25%); Zarei F (Third author), Methodologist (25%)
Funding/Support: This work was supported by Tarbiat Modares University.
Article Type: Descriptive & Survey |
Subject:
Health Promotion Setting
Received: 2022/01/1 | Accepted: 2022/03/14 | Published: 2022/06/15
Received: 2022/01/1 | Accepted: 2022/03/14 | Published: 2022/06/15
References
1. Cascella M, Rajnik M, Aleem A, Dulebohn S, Di Napoli R. Features, evaluation, and treatment of coronavirus (COVID-19). Treasure Island: StatPearls; 2022. [Link]
2. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. [Link] [DOI:10.1016/j.ijantimicag.2020.105924]
3. McIntosh K, Hirsch MS, Bloom A. Coronavirus disease 2019 (COVID-19). UpToDate Hirsch MS Bloom. 2020;5(1):23-7. [Link]
4. Al-Kobaisi MF. Jawetz, Melnick & Adelberg's medical microbiology. Sultan Qaboos Univ Med J. 2007;7(3):273-5. [Link]
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-42. [Link] [DOI:10.1001/jama.2020.2648]
6. World Health Organization. WHO Coronavirus (COVID-19) dashbord [Inretnet]. Genva: World Health Organization; 2021 [cited 2021 Aug 9]. Available from: https://covid19.who.int/. [Link]
7. Rupani PF, Nilashi M, Abumalloh RA, Asadi S, Samad S, Wang S. Coronavirus pandemic (COVID-19) and its natural environmental impacts. Int J Environ Sci Technol. 2020;17(11):4655-66. [Link] [DOI:10.1007/s13762-020-02910-x]
8. Salameh P. COVID-19 in the Eastern Mediterranean region: testing frequency, cumulative cases and mortality analysis. East Mediterr Health J. 2020;26(9):1005-10. [Link] [DOI:10.26719/emhj.20.110]
9. Dil S, Dil N, Maken ZH. COVID-19 trends and forecast in the Eastern Mediterranean region with a particular focus on Pakistan. Cureus. 2020;12(6):e8582. [Link] [DOI:10.7759/cureus.8582]
10. Takian A, Raoofi A, Kazempour-Ardebili S. COVID-19 battle during the toughest sanctions against Iran. Lancet. 2020;395(10229):1035-6. [Link] [DOI:10.1016/S0140-6736(20)30668-1]
11. Maghsudlu M, Eshghi P, Amini Kafi‐Abad S, Sedaghat A, Ranjbaran H, Mohammadi S, et al. Blood supply sufficiency and safety management in Iran during the COVID‐19 outbreak. Vox Sang. 2020;116(2):175-80. [Link] [DOI:10.1111/vox.13012]
12. da Silva ML, Rocha RS, Buheji M, Jahrami H, Cunha KD. A systematic review of the prevalence of anxiety symptoms during coronavirus epidemics. J Health Psychol 2021;26(1):115-25. [Link] [DOI:10.1177/1359105320951620]
13. Patel U, Malik P, Usman MS, Mehta D, Sharma A, Malik FA, et al. Age-adjusted risk factors associated with mortality and mechanical ventilation utilization amongst covid-19 hospitalizations-a systematic review and meta-analysis. SN Compr Clin Med. 2020;2:1740-9. [Link] [DOI:10.1007/s42399-020-00476-w]
14. Samaranayake LP, Fakhruddin KS, Panduwawala C. Sudden onset, acute loss of taste and smell in coronavirus disease 2019 (COVID-19): a systematic review. Acta Odontol Scand. 2020;78(6):467-73. [Link] [DOI:10.1080/00016357.2020.1787505]
15. Kulcsar MA, Montenegro FL, Arap SS, Tavares MR, Kowalski LP. High risk of COVID-19 infection for head and neck surgeons. IntArch Otorhinolaryngol. 2020;24:129-30. [Link] [DOI:10.1055/s-0040-1709725]
16. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. [Link] [DOI:10.1016/S0140-6736(20)30183-5]
17. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973-87. [Link] [DOI:10.1016/S0140-6736(20)31142-9]
18. Min C, Shen F, Yu W, Chu Y. The relationship between government trust and preventive behaviors during the COVID-19 pandemic in China: Exploring the roles of knowledge and negative emotion. Prev Med. 2020;141:106288. [Link] [DOI:10.1016/j.ypmed.2020.106288]
19. Hadi AG, Kadhom M, Yousif E, Hairunisa N. In COVID-19 time, how to protect myself and others? a review. Jurnal Biomedika Dan Kesehatan. 2020;3(3):153-8. [Link] [DOI:10.18051/JBiomedKes.2020.v3.153-158]
20. Di Gennaro F, Pizzol D, Marotta C, Antunes M, Racalbuto V, Veronese N, et al. Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int J Environ Res Public Health. 2020;17(8):2690. [Link] [DOI:10.3390/ijerph17082690]
21. Khazaee-Pool M, Shahrvsand S, Naghibi SA. Predicting Covid-19 Preventive Behaviors Based on Health Belief Model: An Internet-Based Study in Mazandaran Province, Iran. J Mazandaran Univ Med Sci. 2020;30(190):56-66. [Persian] [Link]
22. Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136. [Link] [DOI:10.1037/0278-6133.26.2.136]
23. Elgzar WT, Al-Qahtani AM, Elfeki NK, Ibrahim HA. COVID-19 outbreak: effect of an educational intervention based on health belief model on nursing students' awareness and health beliefs at Najran University, Kingdom of Saudi Arabia. Afr J Reprod Health. 2020;24(2):78-86. [Link]
24. Creswell JW. Educational research: Planning, conducting, and evaluating quantitative. Upper Saddle River, NJ: Prentice Hall; 2002. [Link]
25. Rodrigues IB, Adachi JD, Beattie KA, MacDermid JC. Development and validation of a new tool to measure the facilitators, barriers and preferences to exercise in people with osteoporosis. BMC Musculoskeletal disorders. 2017;18:540. [Link] [DOI:10.1186/s12891-017-1914-5]
26. Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53-55. [Link] [DOI:10.5116/ijme.4dfb.8dfd]
27. Selin KH. Test-retest reliability of the alcohol use disorder identification test in a general population sample. Alcohol Clin Exp Res. 2003;27(9):1428-35. [Link] [DOI:10.1097/01.ALC.0000085633.23230.4A]
28. Tong KK, Chen JH, Yu EWy, Wu AM. Adherence to COVID‐19 Precautionary Measures: Applying the Health Belief Model and Generalised Social Beliefs to a Probability Community Sample. Appl Psychol Health Well Being. 2020;12(4):1205-23. [Link] [DOI:10.1111/aphw.12230]
29. Fathian-Dastgerdi Z, Tavakoli B, Jaleh M. Factors associated with preventive behaviors of COVID-19 among adolescents: Applying the health belief model. Res Soc Adm Pharm. 2021;17(10):1786-90. [Link] [DOI:10.1016/j.sapharm.2021.01.014]
30. Mirzaei A, Kazembeigi F, Kakaei H, Jalilian M, Mazloomi S, Nourmoradi H. Application of health belief model to predict COVID-19-preventive behaviors among a sample of Iranian adult population. J Educ Health Promot. 2021;10:69. [Link] [DOI:10.4103/jehp.jehp_747_20]
31. Almazyad EM, Ahmad A, Jomar DE, Khandekar RB, Al-Swailem S. Perception of ophthalmologists of COVID-19 using the health belief model. Cureus. 2021;13(1):e12681. [Link] [DOI:10.7759/cureus.12681]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |