Volume 10, Issue 2 (2022)
Health Educ Health Promot 2022, 10(2): 221-225 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nejaddadgar N, Jafarzadeh M, Ziapour A, Rezaei F. Determinants of COVID-19 Vaccine Acceptance in Ardabil: a Web-Based Survey. Health Educ Health Promot 2022; 10 (2) :221-225
URL: http://hehp.modares.ac.ir/article-5-56325-en.html
URL: http://hehp.modares.ac.ir/article-5-56325-en.html
1- Department of Health Promotion and Education, School of Public Health, Ardabil University of Medical Sciences, Ardabil, Iran
2- Department of Infectious Diseases, School of Medicine, Ardabil University of Medical Sciences, Ardabil, Iran
3- Cardiovascular Research Center, Health Institute, Imam-Ali hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran
4- Health Education and Promotion Department, health deputy, Ministry of Health, Iran
2- Department of Infectious Diseases, School of Medicine, Ardabil University of Medical Sciences, Ardabil, Iran
3- Cardiovascular Research Center, Health Institute, Imam-Ali hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran
4- Health Education and Promotion Department, health deputy, Ministry of Health, Iran
Full-Text [PDF 750 kb]
(1046 Downloads)
| Abstract (HTML) (977 Views)
Full-Text: (149 Views)
Introduction
COVID-19 disease is a new species of the coronavirus family that was first identified in Wuhan city, Hubei province, China, and from there it spread to other countries [1, 2]. The new coronavirus pandemic in 2020 posed a global health concern [3]. On January 30, 2020, the Director-General of the World Health Organization (WHO) declared the outbreak of coronavirus as a public health emergency and international concern [4]. The virus spreads through small droplets from coughing, sneezing, and talking [5]. Adults may also become infected by touching a contaminated surface and then touching their face (eye, nose, and mouth). The transmission also occurs through aerosols that can stay suspended in the air for longer periods [6]. Coronavirus has infected close to 132 million people with more than 2.8 million deaths as of April 7, 2021 [7]. In the United States alone, the number of COVID-19 cases surpassed 30.5 million with more than 552,000 deaths [8]. Equitable access to safe and effective vaccines and observance of health protocols is critical to ending the COVID-19 pandemic [9]. WHO recommends that initial vaccination should prioritize groups at the highest risk of exposure to infection in each country, including health workers, older persons, and those with other health issues. Once COVID-19 vaccines become more available, countries can expand to vaccinate other priority groups and the general population [10, 11]. In the Islamic Republic of Iran from 3 January 2020 to12 October 2021, there have been 5,716,394 confirmed cases of COVID-19 with 122,868 deaths, reported to WHO, and of 2 October 2021, a total of 57,676,540 vaccine doses have been administered [12].
Yet there is a small group of people who have refused to get COVID-19 vaccines [4]. The anti-vaccine sentiment gets more attention than the actual number of vaccine refusers and appears to have a disproportionate impact on public discourse. In turn, this persistent questioning of vaccine safety despite overwhelming scientific evidence has increased vaccine hesitancy, questions about the safety and efficacy of vaccines among some parents even if they comply with the vaccination recommendations [5], Because vaccine hesitancy in the United States, the proportion of adults who get flu vaccines remains low [6]. On the other hand, to control the epidemic herd immunity is needed. herd immunity occurs when a large portion of a community becomes immune to a disease, making the spread of disease from person to person unlikely. As a result, the whole community becomes protected [7].
This study aimed to examine the determinants of COVID-19 vaccine acceptance.
Materials and Methods
This cross-sectional survey was designed using the Survey Monkey platform and was performed in 2021 on the people of Ardabil province, Iran. Using the snowball sampling strategy, the study investigators shared the survey link on social media (WhatsApp, Telegram channel, and email) for those aged 20 and above (because, at the time of the study, this age group was eligible to receive the vaccine). Data were gathered from 768 adults.
A researcher-made questionnaire with 24 questions was used. This questionnaire consisted of two parts. The first part consisted of 7 questions on sex, age, education, ensuring the health system and vaccine, marital status, and being urban or rural, and the second part consisted of 10 questions in 5 domains, (Perceptions of risk, vaccine safety, vaccine side- effect, chronic disease, religious/personal beliefs). Perceptions of risk had two dimensions: perception of susceptibility and perception of severity, and each one was measured using three questions on a four-point scale Maximum score was set at 24 and the minimum score was four. For assessment, participants’ knowledge about COVID-19 and vaccination was assessed using 6 questions, which were adapted from previous research with “true,” “false” or “not sure”. Each correct response to a knowledge item has been assigned 1 point, and 0 points have been assigned to each incorrect/not sure response. For knowledge items, the total score ranged from 0 to 6. Ensure the health system and vaccine were measured by 2 questions asking respondents to indicate whether they have “a great deal of ensuring”, “only some ensure” or “hardly any ensure at all” in the health system. For analysis, we dichotomized the responses into “a great deal of ensuring” and “hardly any ensure” the total score ranged from 0 to 2. Religious/personal beliefs were measured using three questions on a four-point scale Maximum score was set at 12 and the minimum score was four. Vaccine safety by 2 questions in this part each correct response to a vaccine safety item has been assigned 1 point, and 0 points have been assigned to each incorrect/not sure response the total score ranged from 0 to 2, and vaccine side- effect by 3 questions, in this part each correct response to a vaccine safety item has been assigned 1 point, and 0 points have been assigned to each incorrect/not sure response the total score ranged from 0 to 3. chronic disease with a question total score ranged from 0 to1. The validity of the questionnaire was determined by two methods of face validity and content validity, which were confirmed by experts in health education and Infectious disease specialist. The total content validity index (CVI) in the “relevancy”, “simplicity”, and “clarity” were 83.6, 92.9, and 91.7. The reliability of the questionnaire was further evaluated through internal consistency (α=0.83) and test-retest (r=0.82).
The study was approved ethically by the Ardabil University of Medical Science. The primary participants were requested to roll out the survey further. On receiving and clicking the link, participants got auto-directed to the informed consent page. After they were allowed to take the survey. Participants were aware of the purpose of the study and provided informed consent before accessing the questionnaire and participated voluntarily. No compensation was provided, and all collected data was stored securely.
The data were analyzed by SPSS software version 23 using descriptive statistical methods chi-square and regression tests.
Findings
In our sample, about 68.2% said that they were ready to get the vaccine.
Mean age of study participants was 42.47±12.07 years. The majority of the participants were female, married, and had a college degree. Among the respondents, 18.09% were Unemployed/retired (Table 1).
Table 1) Demographic characteristics of participants
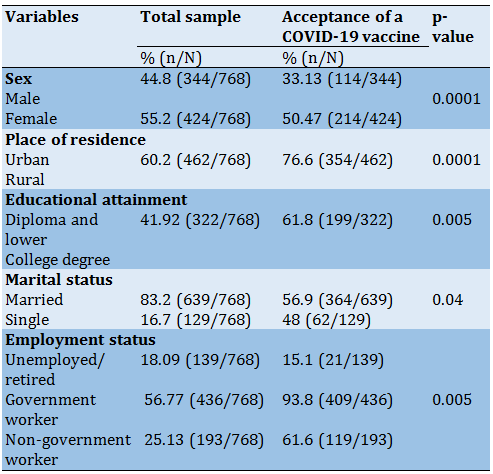
The result showed Women were more likely than men to get the vaccine against COVID (p<0.001), and government worker were the most willing group to receive vaccination against COVID-19 (p<0.002). The mean COVID-19 knowledge score for participants about COVID-19 and vaccination was 4.37±1.41 (range: 0–6) and Participant’s knowledge significantly differed across genders, occupations, and residence places (p<0.05). Willingness to get the vaccine is relatively high among older age groups (59.4% among 40+ year old), being married (56.9%), and city dwellers participants (83.09%).
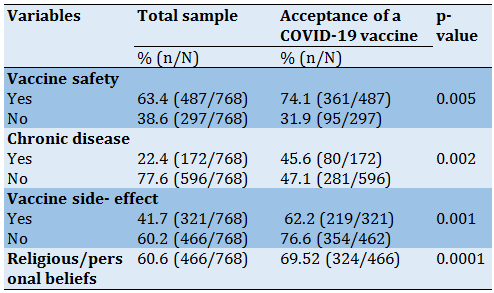
In multivariate model, respondents who were above 40 years (OR: 0.7; 95% CI:0.5-0.94), and married (OR: 1.43; 95% CI: 0.97-2.09) most wanted to get vaccine. Besides, people having trust in the health system were most likely to accept the vaccine (OR: 1.26; 95% CI: 1.01-1.56), and those having a higher perceived risk of acquiring infection were 4.83 times (95% CI: 3.78-6.17) were more likely to receive the vaccine.
According to the findings, the most important factor was the perceived risk of acquiring infection (β=0.68, p=0.001) and the second factor was, religious/personal beliefs Which were impressed on receiving the vaccine (β=0.28, p=0.001).
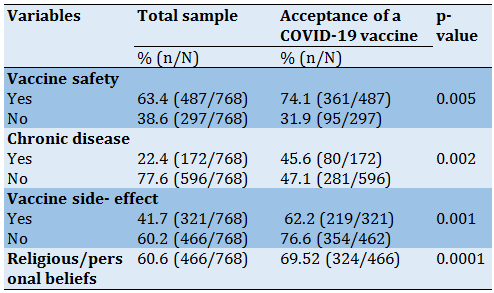
The necessary information about factors adjusted associations related to acceptance COVID-19 vaccine was given in Table 2.
Table 2) Factors adjusted associations related to acceptance COVID-19 vaccine
Discussion
Vaccination is considered one of the most outstanding public health inventions in the 21 st century [13]. In this study, results show that 68.2% of participants were shown willingness to receive vaccination against COVID-19. level of acceptability is considerably low given the magnitude of the COVID-19 pandemic [14-16]. Researchers suggest that herd immunity occurs when a large portion of a community becomes immune to a disease, making the spread of disease from person to person unlikely [17-19]. Herd immunity also can be reached when enough people have been vaccinated against the disease [20]. But reaching herd immunity through vaccination against COVID-19 might be difficult for many reasons [20, 21]. If the proportion of vaccinated people in a community is below the herd immunity threshold, contagious diseases could continue to spread [18, 19]. The level of acceptance of a COVID-19 vaccine in our study was lower than that among Malaysian residents (94.3%) [16], adults in the United States (70%) [17], and residents of 7 European countries [22]. Moreover, a study conducted in Saudi conducted in 2020 showed an acceptability level of 64.7% [21], which is close to our estimate. We identified several factors associated with acceptance of a COVID-19 vaccine; Females were more likely than males to accept vaccination against COVID-19 and people over 40 years (59.4%). Moreover, acceptability in these groups was similar to the findings of a study conducted among adults in Saudi [19]. Nevertheless, local public health strategies should aim to improve acceptance of a potential COVID-19 vaccine among younger adults [20-23].
Moreover, the acceptability of COVID-19 vaccination differed according to marital and employment status, results show government staff, people living in the city, and married people were more willing than those in other [24]. Also, results showed, that acceptance of a COVID-19 vaccine was related to self-perceived chances of contracting the infection and its severity [25-27]. Also, the majority of study participants were concerned about side effects and the safety of the vaccine. Such factors have been reported in prior studies [28, 29]. Studies have shown that a higher trust in the health system is associated with the utilization of preventive health services such as vaccination [30-33]. Although our study sample was large, the generalizability of our results is hampered by the doubtful representativeness of our study sample due to the nonrandom sampling technique used. Another limitation of our study is that participants needed access to a smartphone, tablet, or computer to be able to participate, which might have introduced a possible selection bias. Nevertheless, our study assessed a wide range of factors about the acceptability of COVID-19 vaccination, which may help in guiding future public health efforts that aim to increase the uptake of COVID-19 vaccines.
Conclusion
This study reflected a high level of acceptance of COVID-19 vaccination among the adult population in Ardabil city during the pandemic period. To expand vaccine uptake in response to the COVID-19 pandemic, immunization programs should be designed to remove barriers in vaccine price and vaccination convenience. In addition, health education and communication from authoritative sources will be important to alleviate public concerns about vaccine safety.
Acknowledgments: Our grateful thanks go to all participants in the present study.
Ethical Permissions: This study was drawn from a research project (No. IR.AUMS.REC. 1399.089).
Conflicts of Interests: Nothing to declare
Authors’ Contributions: Nejaddadgar N (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst/Discussion Writer (50%); Jafarzadeh M (Second Author), Assistant Researcher (20%); Ziapour A (Third Author), Methodologist (15%); Rezaei F (Third Author), Assistant Researcher (15%)
Funding/Sources: This study was sponsored by the Deputy of Research and Technology at AUMS.
COVID-19 disease is a new species of the coronavirus family that was first identified in Wuhan city, Hubei province, China, and from there it spread to other countries [1, 2]. The new coronavirus pandemic in 2020 posed a global health concern [3]. On January 30, 2020, the Director-General of the World Health Organization (WHO) declared the outbreak of coronavirus as a public health emergency and international concern [4]. The virus spreads through small droplets from coughing, sneezing, and talking [5]. Adults may also become infected by touching a contaminated surface and then touching their face (eye, nose, and mouth). The transmission also occurs through aerosols that can stay suspended in the air for longer periods [6]. Coronavirus has infected close to 132 million people with more than 2.8 million deaths as of April 7, 2021 [7]. In the United States alone, the number of COVID-19 cases surpassed 30.5 million with more than 552,000 deaths [8]. Equitable access to safe and effective vaccines and observance of health protocols is critical to ending the COVID-19 pandemic [9]. WHO recommends that initial vaccination should prioritize groups at the highest risk of exposure to infection in each country, including health workers, older persons, and those with other health issues. Once COVID-19 vaccines become more available, countries can expand to vaccinate other priority groups and the general population [10, 11]. In the Islamic Republic of Iran from 3 January 2020 to12 October 2021, there have been 5,716,394 confirmed cases of COVID-19 with 122,868 deaths, reported to WHO, and of 2 October 2021, a total of 57,676,540 vaccine doses have been administered [12].
Yet there is a small group of people who have refused to get COVID-19 vaccines [4]. The anti-vaccine sentiment gets more attention than the actual number of vaccine refusers and appears to have a disproportionate impact on public discourse. In turn, this persistent questioning of vaccine safety despite overwhelming scientific evidence has increased vaccine hesitancy, questions about the safety and efficacy of vaccines among some parents even if they comply with the vaccination recommendations [5], Because vaccine hesitancy in the United States, the proportion of adults who get flu vaccines remains low [6]. On the other hand, to control the epidemic herd immunity is needed. herd immunity occurs when a large portion of a community becomes immune to a disease, making the spread of disease from person to person unlikely. As a result, the whole community becomes protected [7].
This study aimed to examine the determinants of COVID-19 vaccine acceptance.
Materials and Methods
This cross-sectional survey was designed using the Survey Monkey platform and was performed in 2021 on the people of Ardabil province, Iran. Using the snowball sampling strategy, the study investigators shared the survey link on social media (WhatsApp, Telegram channel, and email) for those aged 20 and above (because, at the time of the study, this age group was eligible to receive the vaccine). Data were gathered from 768 adults.
A researcher-made questionnaire with 24 questions was used. This questionnaire consisted of two parts. The first part consisted of 7 questions on sex, age, education, ensuring the health system and vaccine, marital status, and being urban or rural, and the second part consisted of 10 questions in 5 domains, (Perceptions of risk, vaccine safety, vaccine side- effect, chronic disease, religious/personal beliefs). Perceptions of risk had two dimensions: perception of susceptibility and perception of severity, and each one was measured using three questions on a four-point scale Maximum score was set at 24 and the minimum score was four. For assessment, participants’ knowledge about COVID-19 and vaccination was assessed using 6 questions, which were adapted from previous research with “true,” “false” or “not sure”. Each correct response to a knowledge item has been assigned 1 point, and 0 points have been assigned to each incorrect/not sure response. For knowledge items, the total score ranged from 0 to 6. Ensure the health system and vaccine were measured by 2 questions asking respondents to indicate whether they have “a great deal of ensuring”, “only some ensure” or “hardly any ensure at all” in the health system. For analysis, we dichotomized the responses into “a great deal of ensuring” and “hardly any ensure” the total score ranged from 0 to 2. Religious/personal beliefs were measured using three questions on a four-point scale Maximum score was set at 12 and the minimum score was four. Vaccine safety by 2 questions in this part each correct response to a vaccine safety item has been assigned 1 point, and 0 points have been assigned to each incorrect/not sure response the total score ranged from 0 to 2, and vaccine side- effect by 3 questions, in this part each correct response to a vaccine safety item has been assigned 1 point, and 0 points have been assigned to each incorrect/not sure response the total score ranged from 0 to 3. chronic disease with a question total score ranged from 0 to1. The validity of the questionnaire was determined by two methods of face validity and content validity, which were confirmed by experts in health education and Infectious disease specialist. The total content validity index (CVI) in the “relevancy”, “simplicity”, and “clarity” were 83.6, 92.9, and 91.7. The reliability of the questionnaire was further evaluated through internal consistency (α=0.83) and test-retest (r=0.82).
The study was approved ethically by the Ardabil University of Medical Science. The primary participants were requested to roll out the survey further. On receiving and clicking the link, participants got auto-directed to the informed consent page. After they were allowed to take the survey. Participants were aware of the purpose of the study and provided informed consent before accessing the questionnaire and participated voluntarily. No compensation was provided, and all collected data was stored securely.
The data were analyzed by SPSS software version 23 using descriptive statistical methods chi-square and regression tests.
Findings
In our sample, about 68.2% said that they were ready to get the vaccine.
Mean age of study participants was 42.47±12.07 years. The majority of the participants were female, married, and had a college degree. Among the respondents, 18.09% were Unemployed/retired (Table 1).
Table 1) Demographic characteristics of participants
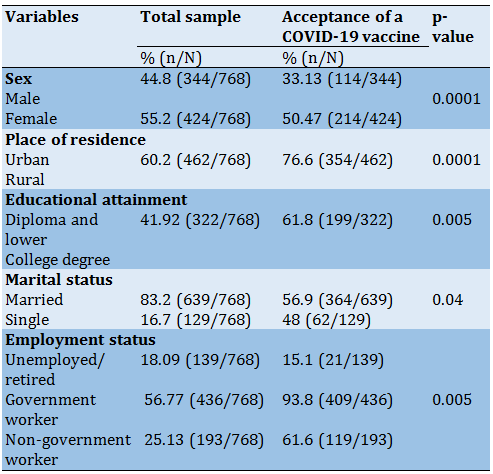
The result showed Women were more likely than men to get the vaccine against COVID (p<0.001), and government worker were the most willing group to receive vaccination against COVID-19 (p<0.002). The mean COVID-19 knowledge score for participants about COVID-19 and vaccination was 4.37±1.41 (range: 0–6) and Participant’s knowledge significantly differed across genders, occupations, and residence places (p<0.05). Willingness to get the vaccine is relatively high among older age groups (59.4% among 40+ year old), being married (56.9%), and city dwellers participants (83.09%).
In multivariate model, respondents who were above 40 years (OR: 0.7; 95% CI:0.5-0.94), and married (OR: 1.43; 95% CI: 0.97-2.09) most wanted to get vaccine. Besides, people having trust in the health system were most likely to accept the vaccine (OR: 1.26; 95% CI: 1.01-1.56), and those having a higher perceived risk of acquiring infection were 4.83 times (95% CI: 3.78-6.17) were more likely to receive the vaccine.
According to the findings, the most important factor was the perceived risk of acquiring infection (β=0.68, p=0.001) and the second factor was, religious/personal beliefs Which were impressed on receiving the vaccine (β=0.28, p=0.001).
The necessary information about factors adjusted associations related to acceptance COVID-19 vaccine was given in Table 2.
Table 2) Factors adjusted associations related to acceptance COVID-19 vaccine
Discussion
Vaccination is considered one of the most outstanding public health inventions in the 21 st century [13]. In this study, results show that 68.2% of participants were shown willingness to receive vaccination against COVID-19. level of acceptability is considerably low given the magnitude of the COVID-19 pandemic [14-16]. Researchers suggest that herd immunity occurs when a large portion of a community becomes immune to a disease, making the spread of disease from person to person unlikely [17-19]. Herd immunity also can be reached when enough people have been vaccinated against the disease [20]. But reaching herd immunity through vaccination against COVID-19 might be difficult for many reasons [20, 21]. If the proportion of vaccinated people in a community is below the herd immunity threshold, contagious diseases could continue to spread [18, 19]. The level of acceptance of a COVID-19 vaccine in our study was lower than that among Malaysian residents (94.3%) [16], adults in the United States (70%) [17], and residents of 7 European countries [22]. Moreover, a study conducted in Saudi conducted in 2020 showed an acceptability level of 64.7% [21], which is close to our estimate. We identified several factors associated with acceptance of a COVID-19 vaccine; Females were more likely than males to accept vaccination against COVID-19 and people over 40 years (59.4%). Moreover, acceptability in these groups was similar to the findings of a study conducted among adults in Saudi [19]. Nevertheless, local public health strategies should aim to improve acceptance of a potential COVID-19 vaccine among younger adults [20-23].
Moreover, the acceptability of COVID-19 vaccination differed according to marital and employment status, results show government staff, people living in the city, and married people were more willing than those in other [24]. Also, results showed, that acceptance of a COVID-19 vaccine was related to self-perceived chances of contracting the infection and its severity [25-27]. Also, the majority of study participants were concerned about side effects and the safety of the vaccine. Such factors have been reported in prior studies [28, 29]. Studies have shown that a higher trust in the health system is associated with the utilization of preventive health services such as vaccination [30-33]. Although our study sample was large, the generalizability of our results is hampered by the doubtful representativeness of our study sample due to the nonrandom sampling technique used. Another limitation of our study is that participants needed access to a smartphone, tablet, or computer to be able to participate, which might have introduced a possible selection bias. Nevertheless, our study assessed a wide range of factors about the acceptability of COVID-19 vaccination, which may help in guiding future public health efforts that aim to increase the uptake of COVID-19 vaccines.
Conclusion
This study reflected a high level of acceptance of COVID-19 vaccination among the adult population in Ardabil city during the pandemic period. To expand vaccine uptake in response to the COVID-19 pandemic, immunization programs should be designed to remove barriers in vaccine price and vaccination convenience. In addition, health education and communication from authoritative sources will be important to alleviate public concerns about vaccine safety.
Acknowledgments: Our grateful thanks go to all participants in the present study.
Ethical Permissions: This study was drawn from a research project (No. IR.AUMS.REC. 1399.089).
Conflicts of Interests: Nothing to declare
Authors’ Contributions: Nejaddadgar N (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst/Discussion Writer (50%); Jafarzadeh M (Second Author), Assistant Researcher (20%); Ziapour A (Third Author), Methodologist (15%); Rezaei F (Third Author), Assistant Researcher (15%)
Funding/Sources: This study was sponsored by the Deputy of Research and Technology at AUMS.
Article Type: Original Research |
Subject:
Health Education and Health Behavior
Received: 2021/10/13 | Accepted: 2022/01/10 | Published: 2022/03/11
Received: 2021/10/13 | Accepted: 2022/01/10 | Published: 2022/03/11
References
1. World Health Organization. Coronavirus disease 2019 (COVID-19): situation report, 72. Geneva: World Health Organization; 2020. [Link]
2. NeJhaddadgar N, Ziapour A, Zakkipour G, Abbas J, Abolfathi M, Shabani M. Effectiveness of telephone-based screening and triage during COVID-19 outbreak in the promoted primary healthcare system: a case study in Ardabil province, Iran. J Public Health. 2020;(30):1301-6. [Link] [DOI:10.1007/s10389-020-01407-8]
3. McKee M, Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat Med. 2020;26:640-2. [Link] [DOI:10.1038/s41591-020-0863-y]
4. Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic?. Lancet . 2020;395(10228):931-4. [Link] [DOI:10.1016/S0140-6736(20)30567-5]
5. Barry M, Ghonem L, Alsharidi A, Alanazi A, Alotaibi NH, Al-Shahrani FS, et al. Coronavirus disease-2019 pandemic in the kingdom of Saudi Arabia: Mitigation measures and hospital preparedness. J Nat Sci Med. 2020;3(3):155-8. [Link] [DOI:10.4103/JNSM.JNSM_29_20]
6. Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine hesitancy: causes, consequences, and a call to action. Am J Prev Med. 2015;49(6 Suppl 4):S391-8. [Link] [DOI:10.1016/j.amepre.2015.06.009]
7. Taherinia M, Hassanvand A. Economic consequences of COVID-19 disease on the Iranian economy; with an emphasis on employment. Q J Nurs Manag. 2020;9(3):43-58. [Persian] [Link]
8. Kaadan MI, Abdulkarim J, Chaar M, Zayegh O, Keblawi MA. Determinants of COVID-19 vaccine acceptance in the Arab world: a cross-sectional study. Global Health Research and Policy. 2021;6(1):1-7. [Link] [DOI:10.1186/s41256-021-00202-6]
9. Thanh Le T, Andreadakis Z, Kumar A, Gomez Roman R, Tollefsen S, Saville M, et al. The COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19(5):305-6. [Link] [DOI:10.1038/d41573-020-00073-5]
10. NeJhaddadgar N, Toghroli R, Yoosefi lebni J, Melca I, Ziapour A. Exploring the barriers in maintaining the health guidelines amid the covid-19 pandemic: a qualitative study approach. INQ. 2022; 59; 1-11. [Link] [DOI:10.1177/00469580221100348]
11. Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, et al. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295-301. [Link] [DOI:10.1016/j.ebiom.2016.08.042]
12. Jorgensen P, Mereckiene J, Cotter S, Johansen K, Tsolova S, Brown C. How close are countries of the WHO European Region to achieving the goal of vaccinating 75% of key risk groups against influenza? Results from national surveys on seasonal influenza vaccination programmes, 2008/2009 to 2014/2015. Vaccine. 2018;36(4):442-52. [Link] [DOI:10.1016/j.vaccine.2017.12.019]
13. Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel). 2021;9(2):160. [Link] [DOI:10.3390/vaccines9020160]
14. Cornally N, Ann Deasy E, McCarthey G, McAuley C, Moran J, Weathers E, et al. Student nurses' intention to get the influenza vaccine. Br J Nurs. 2013;22(21):1207-11. [Link] [DOI:10.12968/bjon.2013.22.21.1207]
15. Kim SY, Seo JW, Ryu E. Korean college students' attitudes and health behaviour regarding human papillomavirus vaccination. Collegian. 2021;28(1):57-62. [Link] [DOI:10.1016/j.colegn.2020.04.009]
16. Weinstein ND, Kwitel A, McCaul KD, Magnan RE, Gerrard M, Gibbons FX. Risk perceptions: assessment and relationship to influenza vaccination. Health Psychol. 2007;26(2):146-51. [Link] [DOI:10.1037/0278-6133.26.2.146]
17. Williams GC, Minicucci DS, Kouides RW, Levesque CS, Chirkov VI, Ryan RM, et al. Self-determination, smoking, diet and health. Health Educ Res. 2002;17(5):512-21. [Link] [DOI:10.1093/her/17.5.512]
18. Griffith J, Marani H, Monkman H. COVID-19 vaccine hesitancy in Canada: content analysis of tweets using the theoretical domains framework. J Med Internet Res. 2021;23(4):e26874. [Link] [DOI:10.2196/26874]
19. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Ann Intern Med. 2020;173(12):964-73. [Link] [DOI:10.7326/M20-3569]
20. Al-Mohaithef M, Padhi BK. Determinants of Covid-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657-63. [Link] [DOI:10.2147/JMDH.S276771]
21. Pogue K, Jensen JL, Stancil CK, Ferguson DG, Hughes SJ, Mello EJ, et al. Influences on attitudes regarding potential Covid-19 vaccination in the United States. Vaccines. 2020;8(4):582. [Link] [DOI:10.3390/vaccines8040582]
22. Sethi S, Kumar A, Shaikh M, Hall CA, Kirk JM, Moss P, et al. The UPTAKE study: a cross-sectional survey examining the insights and beliefs of the UK population on COVID-19 vaccine uptake and hesitancy. BMJ Open. 2021;11(6):e048856. [Link]
23. National Academies of Sciences, Engineering and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, Board on Health Sciences Policy, Committee on Equitable Allocation of Vaccine for the Novel Coronavirus, et al. Framework for equitable allocation of COVID-19 vaccine. National Academies Press (US); 2020. [Link]
24. Garcia L. Willingness to pay for a Covid-19 vaccine high in chile. PharmacoEcon Outcomes News. 2020;858(1):35. [Link] [DOI:10.1007/s40274-020-7008-x]
25. Daly M, Robinson E. Willingness to vaccinate against Covid-19 in the US: Longitudinal evidence from a nationally representative sample of adults from April-October 2020. medRxiv. 2020 Nov. [Link] [DOI:10.1101/2020.11.27.20239970]
26. Machida M, Nakamura I, Kojima T, Saito R, Nakaya T, Hanibuchi T, et al. Acceptance of a COVID-19 Vaccine in Japan during the COVID-19 Pandemic. Vaccines. 2021;9(3):210. [Link] [DOI:10.3390/vaccines9030210]
27. Barry M, Al Amri M, Memish ZA. COVID-19 in the Shadows of MERS-CoV in the Kingdom of Saudi Arabia. J Epidemiol Glob Health. 2020;10(1):1-3. [Link] [DOI:10.2991/jegh.k.200218.003]
28. Hassanat AB, Mnasri S, Aseeri M, Alhazmi K, Cheikhrouhou O, Altarawneh G, et al. A simulation model for forecasting covid-19 pandemic spread: Analytical results based on the current saudi Covid-19 data. Sustainability. 202;13(9):4888. [Link] [DOI:10.3390/su13094888]
29. Callaway E. The race for coronavirus vaccines: a graphical guide. Nature. 2020;580:576-7. [Link] [DOI:10.1038/d41586-020-01221-y]
30. Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 vaccines at pandemic speed. N Engl J Med. 2020;382(21):1969-73. [Link] [DOI:10.1056/NEJMp2005630]
31. Renner B, Reuter T. Predicting vaccination using numerical and affective risk perceptions: the case of A/H1N1 influenza. Vaccine. 2012;30(49):7019-26. [Link] [DOI:10.1016/j.vaccine.2012.09.064]
32. Yamey G, Schäferhoff M, Hatchett R, Pate M, Zhao F, McDade KK. Ensuring global access to COVID-19 vaccines. Lancet. 2020;395(10234):1405-6. [Link] [DOI:10.1016/S0140-6736(20)30763-7]
33. Nguyen T, Holdt Henningsen K, Brehaut JC, Hoe E, Wilson K. Acceptance of a pandemic influenza vaccine: a systematic review of surveys of the general public. Infect Drug Resist. 2011;4:197-207 [Link] [DOI:10.2147/IDR.S23174]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |