Volume 10, Issue 2 (2022)
Health Educ Health Promot 2022, 10(2): 403-409 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mollazadeh A, Mohebbi S, Kharazifard M, Rouzmeh N. Senior Dental Students’ Knowledge and Practice regarding Oral Health of Diabetic Patients in Tehran, Iran. Health Educ Health Promot 2022; 10 (2) :403-409
URL: http://hehp.modares.ac.ir/article-5-54968-en.html
URL: http://hehp.modares.ac.ir/article-5-54968-en.html
1- Department of Orthodontics, Qazvin University of Medical Sciences, Qazvin, Iran
2- Dentistry Research Institute, Tehran University of Medical Sciences, Tehran, Iran
3- Periodontology Department, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
2- Dentistry Research Institute, Tehran University of Medical Sciences, Tehran, Iran
3- Periodontology Department, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
Keywords: Oral health [MeSH], Diabetes Mellitus [MeSH], Health Knowledge, Attitudes, Practice [MeSH], Dental Students [MeSH]
Full-Text [PDF 651 kb]
(973 Downloads)
| Abstract (HTML) (765 Views)
Full-Text: (213 Views)
Introduction
Diabetes mellitus (DM) is among the most common and costliest chronic diseases worldwide. The incidence of DM is on the rise due to lifestyle changes, urbanization, industrialization of communities, and increasing prevalence of obesity and sedentary lifestyle, as well as the improvement of the healthcare systems, which has increased life expectancy [1]. DM is one of the four non-communicable diseases that are intended to be eradicated by world leaders as stated in the 2011 Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases [2]. The Middle East and North Africa (MENA) have the highest prevalence of DM according to the International Diabetes Federation [3]. Iran is one of the 21 members of the International Diabetes Federation of the MENA region. A total of 537 million people worldwide are afflicted with DM; over 73 million of which reside in the MENA; this rate would reach 135.7 million by the year 2045. In 2022, there are 5,450,300 diabetic adult patients in Iran [4]. It is estimated that by the year 2035, the MENA region would rank second for the global rate of increase in the number of diabetic patients [3]. DM is the sixth most common cause of morbidity and mortality in the United States, and the estimated cost of medical care and disability for diabetic patients reaches 91.5 billion dollars annually.
DM has a wide range of long-term complications. It can lead to blindness, end-stage renal disease, and amputation of the extremities [5]. Its macrovascular complications include cardiac disease, cardiovascular diseases, and peripheral vein disease. Such consequences adversely affect the quality of life, and occupational efficiency of patients and impose a great financial burden on both the families and the community due to high healthcare costs. Therefore, early diagnosis and effective treatment of DM are strongly emphasized [6].
Several oral soft tissue and inflammatory conditions may be associated with DM; the most important of which include gingivitis and periodontitis [7]. Reduction of salivary flow, change in the composition of the saliva, and impairment of the sense of taste may also occur [8]. Oral bacterial and fungal infections have been reported in diabetic patients as well. Furthermore, some reports are available regarding oral mucosal lesions such as stomatitis, geographic tongue, benign migratory glossitis, traumatic ulcers, lichen planus, lichenoid reactions, and angular cheilitis in diabetic patients [9-12]. Moreover, delayed healing of mucosal ulcers, mucosal neurosensory disturbances, periapical diseases, dental caries, and tooth loss have been reported in diabetic patients [13]. Diabetic patients are at higher risk of oral mucosal lesions compared with healthy individuals [14]. Nonetheless, the public knowledge regarding the complications of DM is insufficient worldwide [15].
Periodontal disease is the sixth most common complication of DM. It is more common than other oral symptoms such as xerostomia and dental caries in diabetic patients [16]. A mutual relationship exists between DM and periodontal disease [17]. Periodontitis, the severe destructive form of periodontal disease, is a common complaint in diabetic patients. In patients with uncontrolled DM, the risk of development of periodontitis is 3 times higher than the rate in non-diabetic controls [17, 18]. Moreover, periodontitis has a faster and more aggressive development in diabetic patients compared with healthy individuals [17, 19, 20]. Poorly controlled and uncontrolled DM also increases the susceptibility of patients to oral opportunistic infections such as oral candidiasis and also plays a role in the development and aggravation of xerostomia, which can lead to dental caries, oral mucosal ulcers, and infection [8, 13, 21, 22]. Early detection and management of such oral symptoms may aid in the early diagnosis of DM and control of blood glucose levels.
Articles and textbooks have extensively explained how to properly manage diabetic patients in dentistry, with emphasis on knowledge - identifying signs and symptoms - and practice - changing treatment plans according to the patient's diabetes control conditions and playing an effective role in the management of glycemic control of these patients. Despite this broad agreement about guidelines for dental treatment of diabetic patients among dentists, their practice in terms of clinical performance is less than desirable [23].
Knowledge enhancement is the foundation of acquiring health-related habits. Schools and universities are the best places for the implementation of knowledge enhancement programs regarding a healthy lifestyle, healthy nutrition, and the significance of exercise. Some studies have assessed the clinical knowledge of medical students, physicians, and endocrinologists regarding DM [24-29]. Also, the public knowledge level regarding DM has been previously evaluated [30]. However, to the best of the authors’ knowledge, the knowledge level and practice of dental students regarding DM in Iran have not been investigated before. Thus, this study aimed to assess the knowledge and practice of senior dental students in Tehran regarding the oral health of diabetic patients.
Instrument and Methods
This cross-sectional study was conducted on senior dental students of four dental schools in Tehran, namely the School of Dentistry of Tehran University of Medical Sciences, the School of Dentistry of Shahid Beheshti University of Medical Sciences, the School of Dentistry of Shahed University of Medical Sciences, and the School of Dentistry of Islamic Azad University. Senior dental students of the abovementioned four dental schools were selected for participation in this study by convenience sampling. The minimum sample size was calculated to be 130 according to a previous study [31], assuming α=0.05, β=0.2, the number of independent variables to be 6, and R2=0.1 using the Multiple Regression Power Analysis feature of PASS 11 software.
A researcher-made questionnaire was designed by the researchers to assess the knowledge and practice of senior dental students regarding the oral health of diabetic patients by reviewing the relevant literature. The validity of the designed questionnaire was quantitatively assessed by a group of experts including two periodontists, two oral health and community dentistry specialists, two oral medicine specialists, and one epidemiologist. The necessary modifications were made to the questionnaire according to the opinion of the experts. To assess its reliability, the questionnaire was filled out by 10 fifth-year dental students and after one month, the questionnaire was filled out again by the same students, and the results were compared. The reproducibility of all questions was > 80%. The final questionnaire included 32 questions in three domains of demographic information and background, knowledge of dental students about the oral health of diabetic patients, and practice of dental students about the oral health of diabetic patients. The response to each knowledge and practice question was scored 0 (wrong answer) or 1 (correct answer).
The study was approved by the ethics committee of Tehran University of Medical Sciences. Coordinated with four dental schools in Tehran, the questionnaires were distributed in person among the senior students in four days, who were selected by convenience sampling. Students were informed that participation in this study was optional. And for providing privacy while answering the questionnaire, they were collected at the end of working hours. 138 students participated in the study.
After collecting the questionnaires, the data were analyzed using SPSS version 20. The frequency and percentage of the student's responses to each question in each of the knowledge and practice domains were calculated. Inferential analysis was carried out using the linear regression model.
Findings
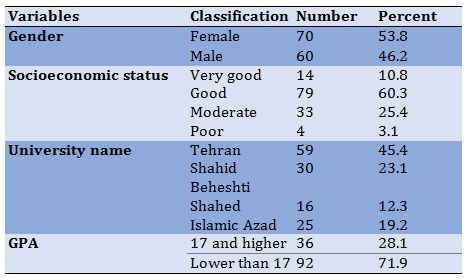
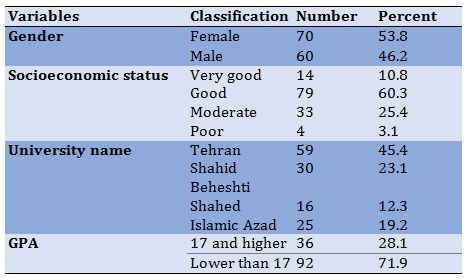
The response rate was 94%. The mean age of the participants was 24.6±2.47 years. Half of the students were females (n=70, 53%). The mean grade point average (GPA) score of the participants was 16.3±0.91 (range 14 to 19). Of all, 14 (10.8%) students declared that their socioeconomic status was very good, while 4 (3.1%) declared that they had a low socioeconomic status. Of all, 59 (45.4%) attended the dental school of Tehran University of Medical Sciences and 16 (12.3%) attended the dental school of Shahed University of Medical Sciences (Table 1).
Table 1) Demographic information of dental students participating in this study
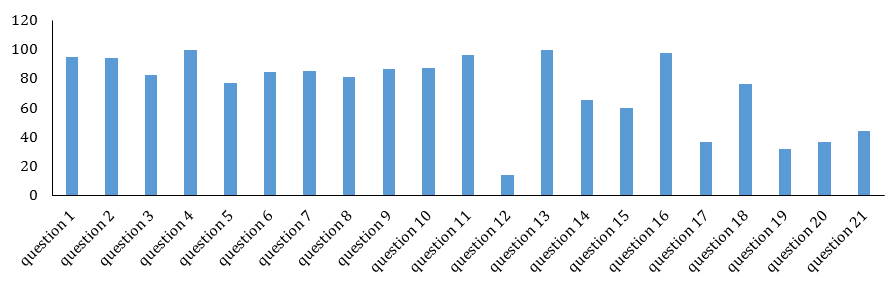
The mean knowledge score of students was 15.29±2.32 out of 21 (range 8 to 19). Questions 4 (patients with uncontrolled or poorly controlled DM often experience a more severe form of periodontitis) and 13 (delayed wound healing is an oral complication of poorly controlled DM) had the highest frequency of correct responses (yes response; n=129, 99.2%). Question 12 (gingival abscess is an oral complication of poorly controlled DM) had the lowest frequency of correct responses (n=18, 13.8%; Diagrams 1 and 2).
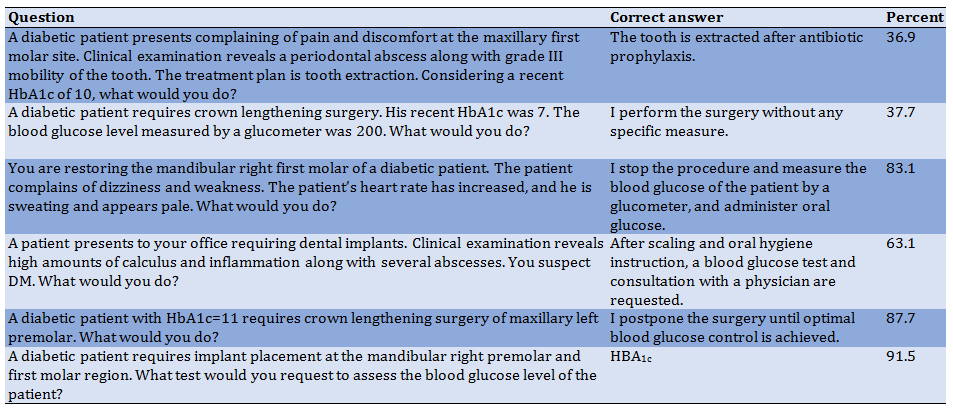
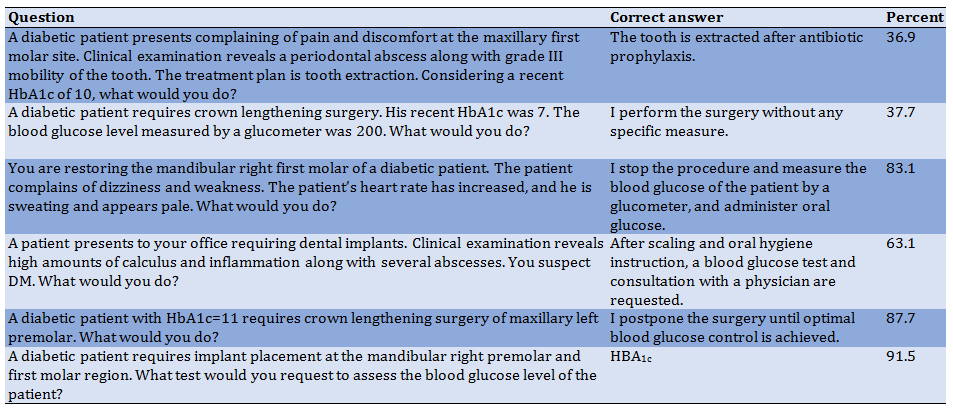
The mean practice score was 4±1.19 out of 6 (range 1 to 6). Question 27 (a diabetic patient seeks dental implant placement in the mandibular right premolar and first molar region. What test do you request to assess the blood glucose level of the patient?) had the highest frequency of correct answers (n=119, 91.5%) while question 22 (a diabetic patient presents complaining of pain and discomfort at the maxillary first molar site. Clinical examination reveals a periodontal abscess along with grade III mobility of the tooth. The treatment plan is tooth extraction. Considering a recent HbA1c of 10, what would you do?) had the lowest frequency of correct answers (n=48, 36.9%) (Table 2).
Diabetes mellitus (DM) is among the most common and costliest chronic diseases worldwide. The incidence of DM is on the rise due to lifestyle changes, urbanization, industrialization of communities, and increasing prevalence of obesity and sedentary lifestyle, as well as the improvement of the healthcare systems, which has increased life expectancy [1]. DM is one of the four non-communicable diseases that are intended to be eradicated by world leaders as stated in the 2011 Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases [2]. The Middle East and North Africa (MENA) have the highest prevalence of DM according to the International Diabetes Federation [3]. Iran is one of the 21 members of the International Diabetes Federation of the MENA region. A total of 537 million people worldwide are afflicted with DM; over 73 million of which reside in the MENA; this rate would reach 135.7 million by the year 2045. In 2022, there are 5,450,300 diabetic adult patients in Iran [4]. It is estimated that by the year 2035, the MENA region would rank second for the global rate of increase in the number of diabetic patients [3]. DM is the sixth most common cause of morbidity and mortality in the United States, and the estimated cost of medical care and disability for diabetic patients reaches 91.5 billion dollars annually.
DM has a wide range of long-term complications. It can lead to blindness, end-stage renal disease, and amputation of the extremities [5]. Its macrovascular complications include cardiac disease, cardiovascular diseases, and peripheral vein disease. Such consequences adversely affect the quality of life, and occupational efficiency of patients and impose a great financial burden on both the families and the community due to high healthcare costs. Therefore, early diagnosis and effective treatment of DM are strongly emphasized [6].
Several oral soft tissue and inflammatory conditions may be associated with DM; the most important of which include gingivitis and periodontitis [7]. Reduction of salivary flow, change in the composition of the saliva, and impairment of the sense of taste may also occur [8]. Oral bacterial and fungal infections have been reported in diabetic patients as well. Furthermore, some reports are available regarding oral mucosal lesions such as stomatitis, geographic tongue, benign migratory glossitis, traumatic ulcers, lichen planus, lichenoid reactions, and angular cheilitis in diabetic patients [9-12]. Moreover, delayed healing of mucosal ulcers, mucosal neurosensory disturbances, periapical diseases, dental caries, and tooth loss have been reported in diabetic patients [13]. Diabetic patients are at higher risk of oral mucosal lesions compared with healthy individuals [14]. Nonetheless, the public knowledge regarding the complications of DM is insufficient worldwide [15].
Periodontal disease is the sixth most common complication of DM. It is more common than other oral symptoms such as xerostomia and dental caries in diabetic patients [16]. A mutual relationship exists between DM and periodontal disease [17]. Periodontitis, the severe destructive form of periodontal disease, is a common complaint in diabetic patients. In patients with uncontrolled DM, the risk of development of periodontitis is 3 times higher than the rate in non-diabetic controls [17, 18]. Moreover, periodontitis has a faster and more aggressive development in diabetic patients compared with healthy individuals [17, 19, 20]. Poorly controlled and uncontrolled DM also increases the susceptibility of patients to oral opportunistic infections such as oral candidiasis and also plays a role in the development and aggravation of xerostomia, which can lead to dental caries, oral mucosal ulcers, and infection [8, 13, 21, 22]. Early detection and management of such oral symptoms may aid in the early diagnosis of DM and control of blood glucose levels.
Articles and textbooks have extensively explained how to properly manage diabetic patients in dentistry, with emphasis on knowledge - identifying signs and symptoms - and practice - changing treatment plans according to the patient's diabetes control conditions and playing an effective role in the management of glycemic control of these patients. Despite this broad agreement about guidelines for dental treatment of diabetic patients among dentists, their practice in terms of clinical performance is less than desirable [23].
Knowledge enhancement is the foundation of acquiring health-related habits. Schools and universities are the best places for the implementation of knowledge enhancement programs regarding a healthy lifestyle, healthy nutrition, and the significance of exercise. Some studies have assessed the clinical knowledge of medical students, physicians, and endocrinologists regarding DM [24-29]. Also, the public knowledge level regarding DM has been previously evaluated [30]. However, to the best of the authors’ knowledge, the knowledge level and practice of dental students regarding DM in Iran have not been investigated before. Thus, this study aimed to assess the knowledge and practice of senior dental students in Tehran regarding the oral health of diabetic patients.
Instrument and Methods
This cross-sectional study was conducted on senior dental students of four dental schools in Tehran, namely the School of Dentistry of Tehran University of Medical Sciences, the School of Dentistry of Shahid Beheshti University of Medical Sciences, the School of Dentistry of Shahed University of Medical Sciences, and the School of Dentistry of Islamic Azad University. Senior dental students of the abovementioned four dental schools were selected for participation in this study by convenience sampling. The minimum sample size was calculated to be 130 according to a previous study [31], assuming α=0.05, β=0.2, the number of independent variables to be 6, and R2=0.1 using the Multiple Regression Power Analysis feature of PASS 11 software.
A researcher-made questionnaire was designed by the researchers to assess the knowledge and practice of senior dental students regarding the oral health of diabetic patients by reviewing the relevant literature. The validity of the designed questionnaire was quantitatively assessed by a group of experts including two periodontists, two oral health and community dentistry specialists, two oral medicine specialists, and one epidemiologist. The necessary modifications were made to the questionnaire according to the opinion of the experts. To assess its reliability, the questionnaire was filled out by 10 fifth-year dental students and after one month, the questionnaire was filled out again by the same students, and the results were compared. The reproducibility of all questions was > 80%. The final questionnaire included 32 questions in three domains of demographic information and background, knowledge of dental students about the oral health of diabetic patients, and practice of dental students about the oral health of diabetic patients. The response to each knowledge and practice question was scored 0 (wrong answer) or 1 (correct answer).
The study was approved by the ethics committee of Tehran University of Medical Sciences. Coordinated with four dental schools in Tehran, the questionnaires were distributed in person among the senior students in four days, who were selected by convenience sampling. Students were informed that participation in this study was optional. And for providing privacy while answering the questionnaire, they were collected at the end of working hours. 138 students participated in the study.
After collecting the questionnaires, the data were analyzed using SPSS version 20. The frequency and percentage of the student's responses to each question in each of the knowledge and practice domains were calculated. Inferential analysis was carried out using the linear regression model.
Findings
The response rate was 94%. The mean age of the participants was 24.6±2.47 years. Half of the students were females (n=70, 53%). The mean grade point average (GPA) score of the participants was 16.3±0.91 (range 14 to 19). Of all, 14 (10.8%) students declared that their socioeconomic status was very good, while 4 (3.1%) declared that they had a low socioeconomic status. Of all, 59 (45.4%) attended the dental school of Tehran University of Medical Sciences and 16 (12.3%) attended the dental school of Shahed University of Medical Sciences (Table 1).
Table 1) Demographic information of dental students participating in this study
The mean knowledge score of students was 15.29±2.32 out of 21 (range 8 to 19). Questions 4 (patients with uncontrolled or poorly controlled DM often experience a more severe form of periodontitis) and 13 (delayed wound healing is an oral complication of poorly controlled DM) had the highest frequency of correct responses (yes response; n=129, 99.2%). Question 12 (gingival abscess is an oral complication of poorly controlled DM) had the lowest frequency of correct responses (n=18, 13.8%; Diagrams 1 and 2).
The mean practice score was 4±1.19 out of 6 (range 1 to 6). Question 27 (a diabetic patient seeks dental implant placement in the mandibular right premolar and first molar region. What test do you request to assess the blood glucose level of the patient?) had the highest frequency of correct answers (n=119, 91.5%) while question 22 (a diabetic patient presents complaining of pain and discomfort at the maxillary first molar site. Clinical examination reveals a periodontal abscess along with grade III mobility of the tooth. The treatment plan is tooth extraction. Considering a recent HbA1c of 10, what would you do?) had the lowest frequency of correct answers (n=48, 36.9%) (Table 2).
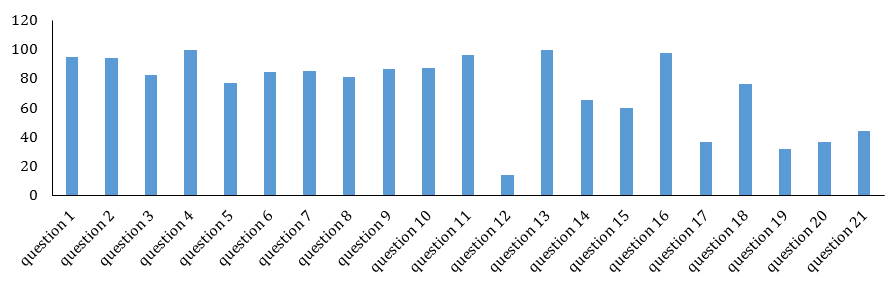
Diagram 1) Results of percent of dental students’ Knowledge regarding oral health of diabetic patients
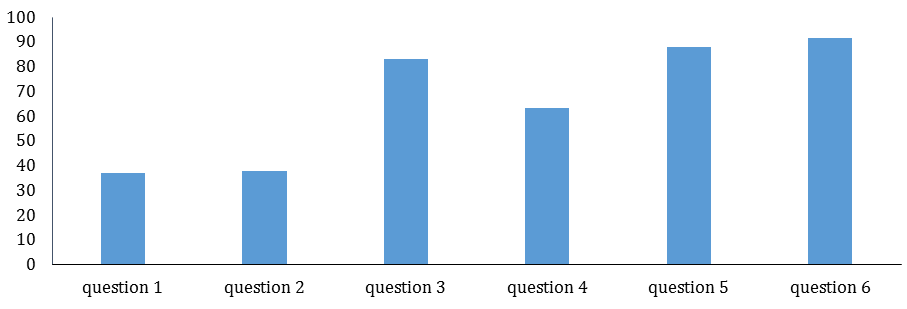
Diagram 2) Results of percent of dental students' practice regarding the oral health of diabetic patients
Table 2) Practice of dental students regarding the oral health of diabetic patients
The correlation test showed no significant correlation between the knowledge and practice of dental students (p>0.05). The regression test showed no association between the knowledge level of students and their age, gender, or socioeconomic status (p>0.05). However, the knowledge score of students had a significant correlation with their GPA score (p=0.00, β-0.312, B=0.782).
The regression test found no significant association between the practice of students and their gender or socioeconomic status (p>0.05). a significant correlation existed between the GPA of students and their practice (p=0.00, β=0.313, B=-0.409). The practice of students had a significant inverse association with their age (p=0.05, β=0.149, B=-0.072).
Discussion
This study assessed the knowledge and practice of senior dental students of four dental schools in Tehran regarding the oral health of diabetic patients. The results showed moderate knowledge and practice of students irrespective of some demographic factors such as gender and socioeconomic status. Also, their knowledge and practice were significantly correlated with their GPA score.
In the present study, the mean practice score was 4 out of 6, which was close to the rate reported by Friesen et al., [32] regarding the practice score of senior dental students (4.6 out of 7). In the current study, 94.6% of dental students were aware of the strong correlation between periodontal disease and systemic health. A total of 71% of dentists practicing in North Carolina in the study by Paquette et al., [33] and 82.5% of dental students in the study by Araújo et al., [34] in Brazil agreed with this statement.
In the present study, 93.8% of dental students were aware of the higher risk of diabetic patients for the development of periodontal disease. This finding was in agreement with the results of previous studies such that 89% of dental students in the study by Araújo et al., [34] in Brazil, 89% of dentists in the study by Paquette et al., [38] in North Carolina, 96.4% of dentists in the study by Al-Khabbaz et al., in Kuwait, and 70% of oral hygienists in the study by Bell et al., in North Carolina were aware of this fact [33-36].
Of all participants of the present study, 82.1% were aware of the fact that treatment of periodontal disease can aid in better control of blood glucose. This finding was in line with the results of Al-Khabbaz et al., (60.1%) [35], and Efurd et al. (82%) [37]. Also, 85.4% of dental students in this study knew those diabetic patients with poorly controlled blood glucose levels poorly respond to dental treatment, which was in accord with the findings of Efurd et al., [37] in Arkansas (64%). Of all, 86.9% of the dental students declared that xerostomia is an oral complication of poorly controlled DM, which was in agreement with the findings of Nivashini et al., [38] (64% of students were aware of this fact). In the present study, 65.4% of students agreed with the statement that poorly controlled DM increases the incidence of dental caries; 81.3% of dental students agreed with this statement. The majority of students (96.2%) in the present study believed that bacterial/fungal infections are among the oral complications of poorly controlled DM, which was in agreement with the results of Nivashini et al., [38] (93.3% of students were aware of this fact). In this study, 99.2% of dental students were aware of poor wound healing in patients with poorly controlled DM. However, only 55.3% of dental students were aware of this fact. Moreover, 76.2% of dental students in the present study knew about an oral mucosal burning sensation in patients with poorly controlled DM while this rate was 49.3%. This difference may be attributed to the difference in educational curricula of the two countries, and it appears that less attention has been paid to this topic in the educational curricula in India [38].
In the present study, 83.1% of dental students well detected the signs and symptoms of hypoglycemic shock and managed it. In the study by Araújo et al., in Brazil, 60% of dental students well detected the signs and symptoms of hypoglycemic shock, and 74.6% of dental students in the study by Nivashini et al. had optimal knowledge about the management of hypoglycemic shock, which was in agreement with the present results [34, 38].
In this study, 63.1% of dental students could diagnose an undetected diabetic patient based on oral manifestations and refer him to a physician. This rate was 61.2% in the study by Lin et al. [39].
In the present study, no correlation was noted between the knowledge of dental students and their practice regarding the oral health of diabetic patients. Similarly, Efurd et al. [37] reported that the knowledge level of dentists and oral hygienists regarding DM had no significant correlation with their practice, which was in agreement with the present results. It appears that the currently provided education regarding the oral health of diabetic patients cannot be put into practice, and the educational curricula require revision. It is suggested to allocate more sessions to the instruction of oral manifestations and complications of systemic diseases and assessment of cases [37].
In the present study, the practice of students had a significant inverse correlation with their age, such that with an increase in age, the practice of students deteriorated. Since all participants were senior dental students and 13.2% of them were between 26 and 40 years of age, they probably had different concerns (while being at the same educational level), which caused their discouragement about their practice.
Age had no significant correlation with the knowledge level of dental students regarding the oral health of diabetic patients in the present study, which was in line with the findings of Lin et al. However, Al-Khabbaz et al. found a significant correlation between the age of dentists and their knowledge. They explained that with an increase in age, dentists and physicians gained greater experience in the management of a higher number of diabetic patients, which resulted in their knowledge enhancement. Since the students in the present study were all from the same academic level and had equal work experience, a lack of a significant correlation between their age and knowledge level was expected [35, 39]. Also, gender had no significant correlation with knowledge and practice, which was in agreement with the results of Lin et al. [39].
No significant correlation was found between the socioeconomic status and knowledge or practice of dental students. However, Kunzel et al. [40] reported that dental clinicians with lower socioeconomic status had a more active role in the management of diabetic patients compared with dentists with moderate and high socioeconomic levels. They concluded that dentists with lower socioeconomic status visit a higher number of undetected diabetic patients. Since dental students were our target population in this study who had not started their practice, this difference between the two studies can be justified [40].
In the present study, a significant correlation was found between the GPA score and the knowledge and practice of dental students. Since the designed questionnaire assessed the knowledge level of students by questions similar to the questions in student exams, a significant correlation between GPA score and knowledge and practice score of students could be expected.
The response rate was 94% in this study, which was a strength. This rate was 49% (n=667) in the study by Paquette et al. [33].
The low participation rate of students attending the dental schools of Islamic Azad University and Shahid Beheshti University of Medical Sciences was a limitation of this study, which was due to their lower number of credits and their shorter attendance time at the university. Future studies can be conducted on students in the 11th term and should consider the limitations of students in university attendance. This study was conducted in only one city (Tehran) in 2018; thus, the results cannot be generalized to all senior dental students of Iran.
Conclusion
This study showed that the knowledge level and practice of senior dental students of Tehran regarding the correlation between periodontal disease and DM was moderate. Because the knowledge of students did not improve their practice, it appears that educational interventions and revision of dental curricula on this topic may improve their practice.
Acknowledgments: None declared.
Ethical Permissions: The study was approved by the ethics committee of Tehran University of Medical Sciences (IR.TUMS.DENTISTRY.REC.1397.185)
Conflicts of Interests: This study was derived from a thesis for a DDS degree in 2019 (code:6408) supported by the Tehran University of Medical Sciences.
Authors’ Contributions: Mollazadeh A (First Author), Introduction Writer/Methodologist /Main Researcher /Discussion Writer (40%); Mohebbi SZ (Second Author), Introduction Writer/ Methodologist/Main Researcher (25%); Kharazifard MJ (Third Author), Assistant Researcher/Statistical Analyst (10%); Rouzmeh N (Third Author), Methodologist/Main Researcher/Discussion Writer (25%)
Funding/Support: None declared.
Diagram 2) Results of percent of dental students' practice regarding the oral health of diabetic patients
Table 2) Practice of dental students regarding the oral health of diabetic patients
The correlation test showed no significant correlation between the knowledge and practice of dental students (p>0.05). The regression test showed no association between the knowledge level of students and their age, gender, or socioeconomic status (p>0.05). However, the knowledge score of students had a significant correlation with their GPA score (p=0.00, β-0.312, B=0.782).
The regression test found no significant association between the practice of students and their gender or socioeconomic status (p>0.05). a significant correlation existed between the GPA of students and their practice (p=0.00, β=0.313, B=-0.409). The practice of students had a significant inverse association with their age (p=0.05, β=0.149, B=-0.072).
Discussion
This study assessed the knowledge and practice of senior dental students of four dental schools in Tehran regarding the oral health of diabetic patients. The results showed moderate knowledge and practice of students irrespective of some demographic factors such as gender and socioeconomic status. Also, their knowledge and practice were significantly correlated with their GPA score.
In the present study, the mean practice score was 4 out of 6, which was close to the rate reported by Friesen et al., [32] regarding the practice score of senior dental students (4.6 out of 7). In the current study, 94.6% of dental students were aware of the strong correlation between periodontal disease and systemic health. A total of 71% of dentists practicing in North Carolina in the study by Paquette et al., [33] and 82.5% of dental students in the study by Araújo et al., [34] in Brazil agreed with this statement.
In the present study, 93.8% of dental students were aware of the higher risk of diabetic patients for the development of periodontal disease. This finding was in agreement with the results of previous studies such that 89% of dental students in the study by Araújo et al., [34] in Brazil, 89% of dentists in the study by Paquette et al., [38] in North Carolina, 96.4% of dentists in the study by Al-Khabbaz et al., in Kuwait, and 70% of oral hygienists in the study by Bell et al., in North Carolina were aware of this fact [33-36].
Of all participants of the present study, 82.1% were aware of the fact that treatment of periodontal disease can aid in better control of blood glucose. This finding was in line with the results of Al-Khabbaz et al., (60.1%) [35], and Efurd et al. (82%) [37]. Also, 85.4% of dental students in this study knew those diabetic patients with poorly controlled blood glucose levels poorly respond to dental treatment, which was in accord with the findings of Efurd et al., [37] in Arkansas (64%). Of all, 86.9% of the dental students declared that xerostomia is an oral complication of poorly controlled DM, which was in agreement with the findings of Nivashini et al., [38] (64% of students were aware of this fact). In the present study, 65.4% of students agreed with the statement that poorly controlled DM increases the incidence of dental caries; 81.3% of dental students agreed with this statement. The majority of students (96.2%) in the present study believed that bacterial/fungal infections are among the oral complications of poorly controlled DM, which was in agreement with the results of Nivashini et al., [38] (93.3% of students were aware of this fact). In this study, 99.2% of dental students were aware of poor wound healing in patients with poorly controlled DM. However, only 55.3% of dental students were aware of this fact. Moreover, 76.2% of dental students in the present study knew about an oral mucosal burning sensation in patients with poorly controlled DM while this rate was 49.3%. This difference may be attributed to the difference in educational curricula of the two countries, and it appears that less attention has been paid to this topic in the educational curricula in India [38].
In the present study, 83.1% of dental students well detected the signs and symptoms of hypoglycemic shock and managed it. In the study by Araújo et al., in Brazil, 60% of dental students well detected the signs and symptoms of hypoglycemic shock, and 74.6% of dental students in the study by Nivashini et al. had optimal knowledge about the management of hypoglycemic shock, which was in agreement with the present results [34, 38].
In this study, 63.1% of dental students could diagnose an undetected diabetic patient based on oral manifestations and refer him to a physician. This rate was 61.2% in the study by Lin et al. [39].
In the present study, no correlation was noted between the knowledge of dental students and their practice regarding the oral health of diabetic patients. Similarly, Efurd et al. [37] reported that the knowledge level of dentists and oral hygienists regarding DM had no significant correlation with their practice, which was in agreement with the present results. It appears that the currently provided education regarding the oral health of diabetic patients cannot be put into practice, and the educational curricula require revision. It is suggested to allocate more sessions to the instruction of oral manifestations and complications of systemic diseases and assessment of cases [37].
In the present study, the practice of students had a significant inverse correlation with their age, such that with an increase in age, the practice of students deteriorated. Since all participants were senior dental students and 13.2% of them were between 26 and 40 years of age, they probably had different concerns (while being at the same educational level), which caused their discouragement about their practice.
Age had no significant correlation with the knowledge level of dental students regarding the oral health of diabetic patients in the present study, which was in line with the findings of Lin et al. However, Al-Khabbaz et al. found a significant correlation between the age of dentists and their knowledge. They explained that with an increase in age, dentists and physicians gained greater experience in the management of a higher number of diabetic patients, which resulted in their knowledge enhancement. Since the students in the present study were all from the same academic level and had equal work experience, a lack of a significant correlation between their age and knowledge level was expected [35, 39]. Also, gender had no significant correlation with knowledge and practice, which was in agreement with the results of Lin et al. [39].
No significant correlation was found between the socioeconomic status and knowledge or practice of dental students. However, Kunzel et al. [40] reported that dental clinicians with lower socioeconomic status had a more active role in the management of diabetic patients compared with dentists with moderate and high socioeconomic levels. They concluded that dentists with lower socioeconomic status visit a higher number of undetected diabetic patients. Since dental students were our target population in this study who had not started their practice, this difference between the two studies can be justified [40].
In the present study, a significant correlation was found between the GPA score and the knowledge and practice of dental students. Since the designed questionnaire assessed the knowledge level of students by questions similar to the questions in student exams, a significant correlation between GPA score and knowledge and practice score of students could be expected.
The response rate was 94% in this study, which was a strength. This rate was 49% (n=667) in the study by Paquette et al. [33].
The low participation rate of students attending the dental schools of Islamic Azad University and Shahid Beheshti University of Medical Sciences was a limitation of this study, which was due to their lower number of credits and their shorter attendance time at the university. Future studies can be conducted on students in the 11th term and should consider the limitations of students in university attendance. This study was conducted in only one city (Tehran) in 2018; thus, the results cannot be generalized to all senior dental students of Iran.
Conclusion
This study showed that the knowledge level and practice of senior dental students of Tehran regarding the correlation between periodontal disease and DM was moderate. Because the knowledge of students did not improve their practice, it appears that educational interventions and revision of dental curricula on this topic may improve their practice.
Acknowledgments: None declared.
Ethical Permissions: The study was approved by the ethics committee of Tehran University of Medical Sciences (IR.TUMS.DENTISTRY.REC.1397.185)
Conflicts of Interests: This study was derived from a thesis for a DDS degree in 2019 (code:6408) supported by the Tehran University of Medical Sciences.
Authors’ Contributions: Mollazadeh A (First Author), Introduction Writer/Methodologist /Main Researcher /Discussion Writer (40%); Mohebbi SZ (Second Author), Introduction Writer/ Methodologist/Main Researcher (25%); Kharazifard MJ (Third Author), Assistant Researcher/Statistical Analyst (10%); Rouzmeh N (Third Author), Methodologist/Main Researcher/Discussion Writer (25%)
Funding/Support: None declared.
Article Type: Descriptive & Survey |
Subject:
Oral Health Education/Promotion
Received: 2021/08/19 | Accepted: 2022/04/12 | Published: 2022/06/15
Received: 2021/08/19 | Accepted: 2022/04/12 | Published: 2022/06/15
References
1. Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001 Dec;414(6865):782-7. [Link] [DOI:10.1038/414782a]
2. Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438-47. [Link] [DOI:10.1016/S0140-6736(11)60393-0]
3. Esteghamati A, Larijani B, Aghajani MH, Ghaemi F, Kermanchi J, Shahrami A, et al. Diabetes in Iran: prospective analysis from first nationwide diabetes report of national program for prevention and control of diabetes (NPPCD-2016). Sci Rep. 2017;7(1):13461. [Link] [DOI:10.1038/s41598-017-13379-z]
4. The International Diabetes Federation. IDF MENA members [Internet]. Unknown City: The International Diabetes Federation; 2022 [cited 2022 Apr 2]. Available from: https://idf.org/our-network/regions-members/middle-east-and-north-africa/members/35-iran.html [Link]
5. Harris MI, Eastman RC. Early detection of undiagnosed diabetes mellitus: a US perspective. Diabetes Metab Res Rev. 2000;16(4):230-6.
https://doi.org/10.1002/1520-7560(2000)9999:9999<::AID-DMRR122>3.0.CO;2-W [Link] [DOI:10.1002/1520-7560(2000)9999:99993.0.CO;2-W]
6. Moore PA, Orchavd T, Guggenheimer J, Weyant RJ. Diabetes and oral health promotion: a survey of disease prevention behaviors. J Am Dent Assoc. 2000;131(9):1333-41. [Link] [DOI:10.14219/jada.archive.2000.0388]
7. Baldwin E. Oral health. Lancet. 2009;373(9664):628-9. [Link] [DOI:10.1016/S0140-6736(09)60392-5]
8. Chávez EM, Borrell LN, Taylor GW, Ship JA. A longitudinal analysis of salivary flow in control subjects and older adults with type 2 diabetes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(2):166-73. [Link] [DOI:10.1067/moe.2001.112054]
9. Collin HL, Niskanen L, Uusitupa M, Töyry J, Collin P, Koivisto AM, et al. Oral symptoms and signs in elderly patients with type 2 diabetes mellitus: a focus on diabetic neuropathy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(3):299-305. [Link] [DOI:10.1067/moe.2000.107536]
10. Guggenheimer J, Moore PA, Rossie K, Myers D, Mongelluzzo MB, Block HM, et al. Insulin-dependent diabetes mellitus and oral soft tissue pathologies: I. Prevalence and characteristics of non-candidal lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(5):563-9. [Link] [DOI:10.1067/moe.2000.104476]
11. Guggenheimer J, Moore PA, Rossie K, Myers D, Mongelluzzo MB, Block HM, et al. Insulin-dependent diabetes mellitus and oral soft tissue pathologies. II. Prevalence and characteristics of Candida and candidal lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(5):570-6. [Link] [DOI:10.1067/moe.2000.104477]
12. Sandberg GE, Sundberg HE, Fjellstrom CA, Wikblad KF. Type 2 diabetes and oral health: a comparison between diabetic and non-diabetic subjects. Diabetes Res Clin Pract. 2000;50(1):27-34. [Link] [DOI:10.1016/S0168-8227(00)00159-5]
13. Lamster IB, Lalla E, Borgnakke WS, Taylor GW. The relationship between oral health and diabetes mellitus. J Am Dent Assoc. 2008;139:19S-24S. [Link] [DOI:10.14219/jada.archive.2008.0363]
14. Saini R, Al-Maweri SA, Saini D, Ismail NM, Ismail AR. Oral mucosal lesions in non oral habit diabetic patients and association of diabetes mellitus with oral precancerous lesions. Diabetes Res Clin Pract. 2010;89(3):320-6. [Link] [DOI:10.1016/j.diabres.2010.04.016]
15. Masood Mirza K, Khan AA, Ali MM, Chaudhry S. Oral health knowledge, attitude, and practices and sources of information for diabetic patients in Lahore, Pakistan. Diabetes Care. 2007;30(12):3046-7. [Link] [DOI:10.2337/dc07-0502]
16. Löe H. Periodontal disease: the sixth complication of diabetes mellitus. Diabetes care. 1993;16(1):329-34. [Link] [DOI:10.2337/diacare.16.1.329]
17. Mealey BL. Periodontal disease and diabetes: A two-way street. J Am Dent Assoc. 2006;137:S26-31. [Link] [DOI:10.14219/jada.archive.2006.0404]
18. Tsai C, Hayes C, Taylor GW. Glycemic control of type 2 diabetes and severe periodontal disease in the US adult population. Community Dent Oral. 2002;30(3):182-92. [Link] [DOI:10.1034/j.1600-0528.2002.300304.x]
19. Khader YS, Dauod AS, El-Qaderi SS, Alkafajei A, Batayha WQ. Periodontal status of diabetics compared with nondiabetics: a meta-analysis. J Diabetes Complicat. 2006;20(1):59-68. [Link] [DOI:10.1016/j.jdiacomp.2005.05.006]
20. Taylor GW, Borgnakke W. Periodontal disease: associations with diabetes, glycemic control and complications. Oral Dis. 2008;14(3):191-203. [Link] [DOI:10.1111/j.1601-0825.2008.01442.x]
21. Matthews DC. The relationship between diabetes and periodontal disease. J Can Dent Assoc. 2002;68(3):161-4. [Link]
22. Soell M, Hassan M, Miliauskaite A, Haikel Y, Selimovic D. The oral cavity of elderly patients in diabetes. Diabetes Metab. 2007;33:S10-S8. [Link] [DOI:10.1016/S1262-3636(07)80053-X]
23. Forbes K, Thomson WM, Kunzel C, Lalla E, Lamster IB. Management of patients with diabetes by general dentists in New Zealand. J Periodontol. 2008;79(8):1401-8. [Link] [DOI:10.1902/jop.2008.070640]
24. Al‐Habashneh R, Barghout N, Humbert L, Khader Y, Alwaeli H. Diabetes and oral health: doctors' knowledge, perception and practices. J Eval Clin Pract. 2010;16(5):976-80. [Link] [DOI:10.1111/j.1365-2753.2009.01245.x]
25. Jaiswal R, Shenoy N, Thomas B. Extent of awareness regarding periodontal disease in diabetic patients among medical interns. J Health Alli Sci NU. 2015;5(4):17-21. [Link] [DOI:10.1055/s-0040-1703928]
26. Mumtaz S, Ashfaq T, Siddiqui H. Knowledge of medical students regarding diabetes mellitus at Ziauddin University, Karachi. J Pak Med Assoc. 2009;59(3):163-6. [Link]
27. Poudel P, Griffiths R, Wong VW, Arora A, George A. Knowledge and practices of diabetes care providers in oral health care and their potential role in oral health promotion: a scoping review. Diabetes Res Clin Pract. 2017;130:266-77. [Link] [DOI:10.1016/j.diabres.2017.06.004]
28. Umeizudike KA, Iwuala SO, Ozoh OB, Ayanbadejo PO, Fasanmade OA. Association between periodontal diseases and systemic illnesses: A survey among internal medicine residents in Nigeria. Saudi Dent J. 2016;28(1):24-30. [Link] [DOI:10.1016/j.sdentj.2015.03.005]
29. Yuen HK, Onicescu G, Hill EG, Jenkins C. A survey of oral health education provided by certified diabetes educators. Diabetes Res Clin Pract. 2010;88(1):48-55. [Link] [DOI:10.1016/j.diabres.2009.12.015]
30. Aljoudi AS, Taha AZ. Knowledge of diabetes risk factors and preventive measures among attendees of a primary care center in eastern Saudi Arabia. Ann Saudi Med.. 2009;29(1):15-9. [Link] [DOI:10.4103/0256-4947.51813]
31. Khan N, Gomathi KG, Shehnaz SI, Muttappallymyalil J. Diabetes mellitus-related knowledge among university students in Ajman, United Arab Emirates. Sultan Qaboos Univ Med J. 2012;12(3):306. [Link] [DOI:10.12816/0003144]
32. Friesen LR, Walker MP, Kisling RE, Liu Y, Williams KB. Knowledge of risk factors and the periodontal disease-systemic link in dental students' clinical decisions. J Dent Educ. 2014;78(9):1244-51. [Link] [DOI:10.1002/j.0022-0337.2014.78.9.tb05795.x]
33. Paquette DW, Bell KP, Phillips C, Offenbacher S, Wilder RS. Dentists' knowledge and opinions of oral-systemic disease relationships: relevance to patient care and education. J Dent Educ. 2015;79(6):626-35. [Link] [DOI:10.1002/j.0022-0337.2015.79.6.tb05934.x]
34. Araújo PC, Garbín CA, Moimaz SA, Saliba NA, Arcieri RM. Perception and attitude about systemic health and periodontal disease among dentistry undergraduates. OHPD. 2013;11(4):383-8. [Link]
35. Al‐Khabbaz AK, Al‐Shammari KF, Al‐Saleh NA. Knowledge about the association between periodontal diseases and diabetes mellitus: contrasting dentists and physicians. J Periodontol. 2011;82(3):360-6. [Link] [DOI:10.1902/jop.2010.100372]
36. Bell KP, Phillips C, Paquette DW, Offenbacher S, Wilder RS. Dental hygienists' knowledge and opinions of oral-systemic connections: implications for education. J dent educ. 2012;76(6):682-94. [Link] [DOI:10.1002/j.0022-0337.2012.76.6.tb05302.x]
37. Efurd MG, Bray KK, Mitchell TV, Williams K. Comparing the risk identification and management behaviors between oral health providers for patients with diabetes. Am Dent Hygienists Assoc. 2012;86(2):130-40. [Link]
38. Nivashini G, Kumar M. Knowledge and awareness among undergraduate dental students regarding oral health of diabetes mellitus patients. Drug Invent Today. 2018;10(4). [Link]
39. Lin H, Zhang H, Yan Y, Liu D, Zhang R, Liu Y, et al. Knowledge, awareness, and behaviors of endocrinologists and dentists for the relationship between diabetes and periodontitis. Diabetes Res Clin Pract. 2014;106(3):428-34. [Link] [DOI:10.1016/j.diabres.2014.09.008]
40. Kunzel C, Lalla E, Lamster I. Dentists' management of the diabetic patient: contrasting generalists and specialists. Am J Public Health. 2007;97(4):725-30. [Link] [DOI:10.2105/AJPH.2006.086496]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |