Volume 10, Issue 1 (2022)
Health Educ Health Promot 2022, 10(1): 23-31 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Isfahani P, Corani Bahador R, Peirovy S, Afshari M. Quality of Life among Cancer Patients in Iran. Health Educ Health Promot 2022; 10 (1) :23-31
URL: http://hehp.modares.ac.ir/article-5-52747-en.html
URL: http://hehp.modares.ac.ir/article-5-52747-en.html
1- Department of Health Services Management, School of Public Health, Zabol University of Medical Sciences, Zabol, Iran
2- Department of Epidemiology and biostatic, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran
3- Internal Medicine Department, School of Nursing and Allied Medical Sciences, Maragheh University of Medical Sciences, Maragheh, Iran
4- Department of Health Policy and Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran
2- Department of Epidemiology and biostatic, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran
3- Internal Medicine Department, School of Nursing and Allied Medical Sciences, Maragheh University of Medical Sciences, Maragheh, Iran
4- Department of Health Policy and Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 593 kb]
(910 Downloads)
| Abstract (HTML) (1453 Views)
Full-Text: (248 Views)
Introduction
One of the important public health problems in developing and developed countries is cancer [1]. Cancer consists of more than a hundred different diseases that affect all ethnic, racial, age, sex, economic, and social groups. According to the World Health Organization (WHO), the number of new cases of cancer increased from 10 million in 2000 to 15 million in 2020, with developing countries accounting for approximately 60 percent of the new cases. WHO also estimates that cancer-related deaths will increase from 9 million in 2015 to 11.4 million in 2030, with 7 percent of deaths occurring in low-and middle-income countries (LMICs). The annual incidence of cancer in Iran is about 70,000 cases and the annual number of cancer deaths is about 30,000. Given the increase in life expectancy and the growing elderly population in Iran, the incidence of cancer is expected to increase significantly in the coming decades [2].
Diagnosis with cancer was associated with pain, loss of function, and impending death, but today, with new treatments, it is considered a chronic disease in more than half of cases [3]. It affects all aspects of quality of life, including physical, psychological, functional, social, and economic well-being [4]. Cancer disrupts the patients’ social life, daily routines, and functions [5], making them more dependent on others and less capable of supporting others. These problems, coupled with prolonged hospitalization, frequent visits, various treatments, and high treatment costs, reduce the quality of life (QoL) of cancer patients [6]. Today, QoL has become an integral part of the evaluation criteria for cancer treatment [7].
QoL is evaluated in order to choose the optimum treatment and care for patients based on their health status and their physical, mental, and social well-being [8]. There are different definitions of QoL. For example, WHO defines QoL as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns.” [9]. Cancer affects patients' QoL to varying degrees. Problems that typically affect the QoL of cancer patients include diagnostic and therapeutic procedures, stress, pain, depression, the impact of cancer on social/family relationships, nutritional issues, and treatment-related complications [10, 11].
There have been several studies on the QoL of cancer patients in various regions of Iran. For example, the QoL of preschool children with cancer visiting a hospital in Shiraz city in 2012 was about 15.81±63.35 [12]. Moreover, in a 2009 study in Ramsar city, the QoL of cancer patients was reported to be about 31.2±8.6 [13].
However, these studies cannot provide a comprehensive view of this problem for the entire country. Integrating the results of validated studies in this area can provide better recommendations for policymakers and enable them to make evidence-based policies. Therefore, the purpose of this research was to conduct a meta-analysis of the QoL of cancer patients in Iran.
Information & Methods
This systematic review is a meta-analysis study and conducted in 2020. It followed the guidelines for preferred reporting items for systematic review and meta‑analysis (PRISMA) [14]. To identify relevant articles until December 20, 2020, researchers searched for articles published electronically in Persian databases including Scientific Information Database (SID) and Magiran as well as English databases including PubMed, Web of Science, Scopus, and Google Scholar. Persian and English keywords and a combination of these terms were used in searches. These keywords included Quality of Life, Cancer, Tumor, and Iran/Iranian along with AND/OR operators. Besides, the reference lists of published articles were examined to increase sensitivity and to find more relevant studies (Table 1). The search was initially conducted in December 2020 and then updated in August 2021, not resulting from any additional studies that faced the inclusion criteria. The articles that did not meet the following criteria were excluded: 1) studies that did not report the QoL of cancer patients; 2) letter to the editor, case-control, randomized controlled trials and qualitative studies 3) grey literature, books, and dissertations; 4) articles, documents, and reports published after December 20, 2020; 5) articles that examine the relationship between QoL and certain factors without determining the QoL of cancer patients; 6) studies that did not obtain the minimum score of 10; 7) studies published in any language other than Persian or English. On the other hand, all Persian and English cross‑sectional articles that obtained the critical score and that determined QoL among cancer patients in Iran were included.
The quality of the 30 included articles was assessed independently by two authors (first and last authors) using the 15-point instrument of Mitton et al. [15]. In this checklist, each item is given a score of 0 (not present or reported), 1 (present but low quality), 2 (present and midrange quality), or 3 (present and high quality). Disagreements were resolved through discussion or by consulting a third reviewer (first author) if necessary. Finally, only midrange and high-quality studies were included in this review and meta-analysis based on the instructions of the KTE empirical article quality rating sheet:
0 – not present or reported anywhere in the article
1 – present but low quality
2 – present and midrange quality
3 – present and high quality
________ 1. Literature Review: Directly related recent literature is reviewed and research gap (s) identified.
________ 2. Research Questions and Design: A priori research questions are stated, and hypotheses, a research purpose statement, and/or a general line of inquiry is outlined. A study design or research approach is articulated.
________ 3. Population and Sampling: The setting, target population, participants, and approach to sampling are outlined in detail.
________ 4. Data Collection and Capture: Key concepts/measures/variables are defined. A systematic approach to data collection is reported. Response or participation rate and/or completeness of information capture is reported.
________ 5. Analysis and Results Reporting: An approach to analysis and a plan to carry out that analysis is specified. Results are clear and comprehensive. Conclusions follow logically from the findings.
________ /15=Total Score
The initial search was done by the first and last authors. Then, an additional search was conducted by the third author. The data were extracted and evaluated by all authors. Finally, the final analysis was done by the first author. The duplicate articles were removed using Endnote x9 software. Extracted data included the title of the article, the first author, year of publication, average age, sample size, instrument, statistical population, methodology, location of study, and QoL, and an Excel 2016 spreadsheet was used for data entry. The initial search resulted in 5,686 articles. After excluding duplicates and irrelevant articles, 3,138 studies were selected for abstract examination. After reviewing the abstracts, 3,085 articles were removed. Also, 23 articles were removed after examining the full texts as they did not report the mean±SD values for the QoL of cancer patients. Finally, 30 studies [13, 16-44] were found eligible for inclusion in the meta-analysis (Diagram 1).
Data were analyzed using the Comprehensive Meta-Analysis (CMA) software version 2.2.064 (the US, Biostat Inc.). The heterogeneity of the studies was assessed using Cochran’s Q-test statistics and I2 test. Strong evidence of heterogeneity was observed (I2=99.94, p<0.05), and, thus, a random-effects model was used to synthesize their results. The funnel plot and Egger’s test were used to assess the likelihood of publication bias, and the results showed that publication bias was not statistically significant (p=0.055). Finally, the effect of variables that could be the potential sources of heterogeneity was examined using the meta-regression technique. Point estimates of QoL in cancer patients were calculated in forest plots at the 95% confidence interval, where the size of the box indicates the weight of each study and the lines on its sides represent the 95% CI.
Table 1) Search stages
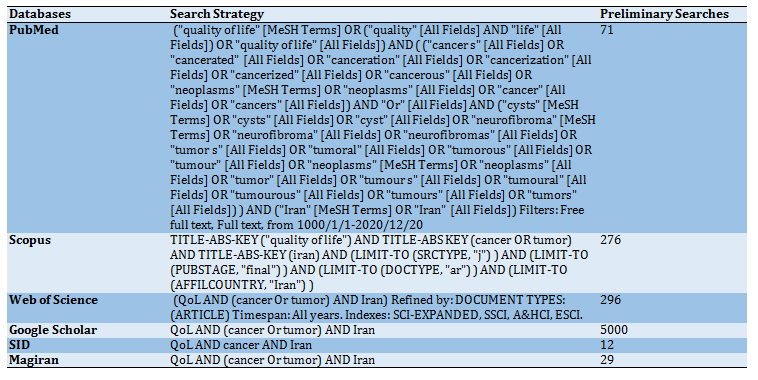
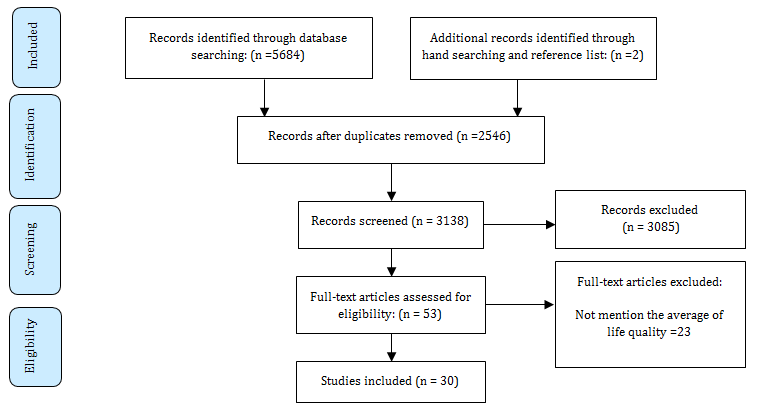
Diagram 1) PRISMA flow chart for study selection
Findings
Most of these studies were conducted in 2010 and 2011. More than half of these studies were published after 2009 (Diagram 2). Most studies were done in Tehran, Gilan, and Qazvin provinces (Diagram 3).
Based on the random-effects model, the average QoL of cancer patients was 50.83±3.07 (44.80-56.86; 95% CI). The highest QoL was observed in the city of Qazvin in 2012 at 103.07±1.61 (100.11-106.03: 95% CI) and the lowest QoL was observed in the city of Tehran in 2010 at 4.05±0.36 (3.35-4.75: 95% CI) (Table 2).
The results were summarized by sample size, studies quality, studied population, cancer type, questionnaire type, and geographic region (Table 3). The mean QoL of cancer patients was higher in the eastern region of Iran. Patients with genital cancer had a better QoL than those with other types of cancer. The mean QoL was higher in men and women than children. Moreover, studies with sample sizes greater than 100 reported higher mean values. Finally, studies with midrange quality reported higher mean values than those with higher quality. Higher QoL scores were reported using the McGill questionnaire than other instruments.
The results of evaluating heterogeneity indicated a high level of heterogeneity among the included studies (Q=48605.498; p=0.0001). Thus, a meta-regression model was used to identify the variables that could potentially cause heterogeneity. The results showed in Table 4 and Diagram 4 indicate that sample size, publication year, and average age contributed to the heterogeneity of studies on the QoL in Iranian cancer patients. The results revealed that the QoL of Iranian cancer patients has decreased by 2.48% each year. One year increase in patients’ age decreased QoL by 0.16. Moreover, the results showed that one unit increase in sample size has increased QoL by 0.17 in Iranian cancer patients.
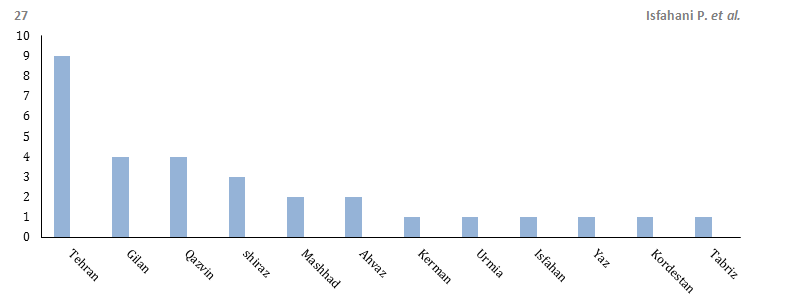
Diagram 3) Frequency distribution of studied QoL among cancer patients
Table 2) Results of forest plot for 31 studies
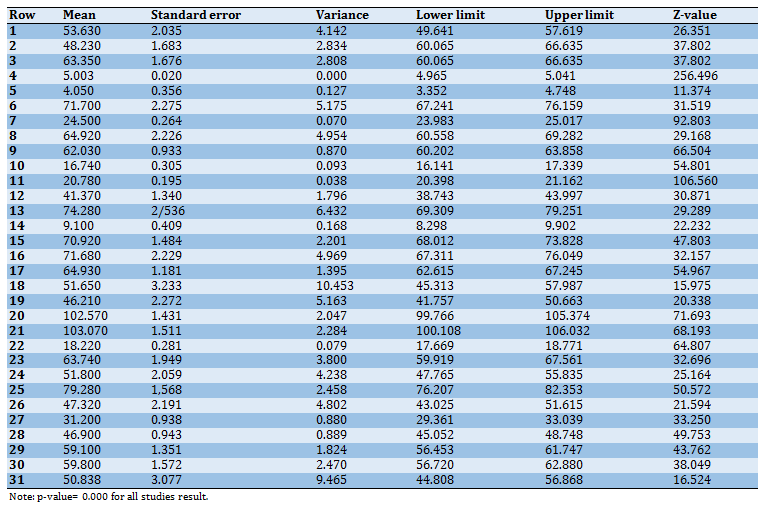
Table 3) Subgroup analyses of the included studies
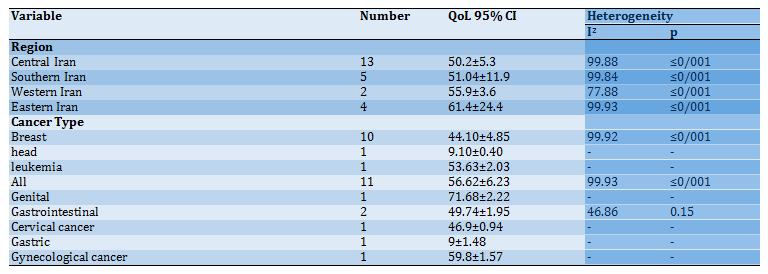
Continue of Table 3) Subgroup analyses of the included studies
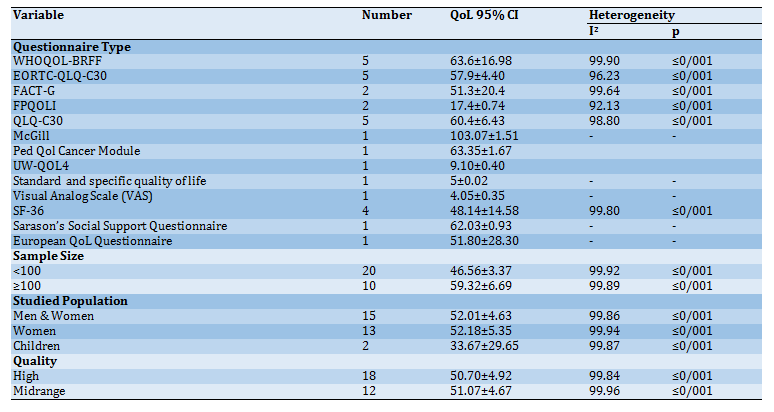
Table 4) Results of meta-regression
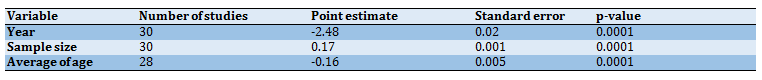
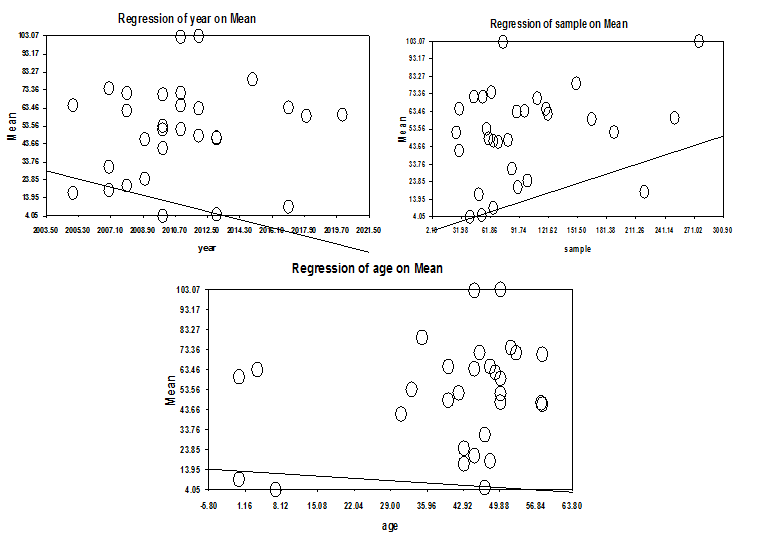
Diagram 4) Results of meta-regression
Discussion
The purpose of this study was to determine the QoL of cancer patients in Iran. By examining eight databases, 30 relevant articles were identified. The overall average QoL of Iranian cancer patients was 50.83±3.07. Several studies have examined the QoL of cancer patients worldwide. For example, the average QoL of cancer patients was reported to be 105±12.93 in cancer hospitals of Karnataka in 2017 [45] and 6.88±1.41 in Chennai women with cervical cancer [46]. The QoL of cancer patients varies. The difference in studies is because of the difference in culture, context, population, the conditions of this disease, and treatment process. Cancer can result in different types of changes in the life of cancer patients [47].
The present research showed that one unit increase in sample size increased the average QoL of cancer patients by 0.17. In other words, studies that use a small sample unintentionally create sampling bias and, as a result, cannot provide valuable information for health policymakers and managers. Therefore, studies on the QoL of cancer patients must use a representative sample and employ appropriate sampling techniques.
In the present study, the mean QoL score of cancer patients varied in different regions of Iran. That is, the mean QoL score of cancer patients was 43.4 in six studies in the northern region, 51.6 in one study in the western region, 49.6 in 11 studies in the central region was, 51.04 in five studies in the southern region, and 61.4 in four studies in the eastern region. Therefore, the average QoL of cancer patients was higher in eastern Iran compared to other regions of the country. However, the QoL of cancer patients has been investigated only in a limited number of Iran’s provinces. Therefore, these studies have not been extensive and this gap can be filled in future research.
In recent years, several studies have been conducted on the QoL of cancer patients. However, the results of these studies showed large dispersion and heterogeneity. Another key factor is the instrument t used to measure QoL among cancer patients. Given that there are a variety of instruments, the QoL of cancer patients has been measured differently. Therefore, differences between the results of the reviewed studies can be, in part, due to differences in the instrument used to measure this variable. In this article, the average QoL of cancer patients was higher when using the McGill questionnaire than other instruments. Overall, there is no comprehensive questionnaire for measuring the QoL of cancer patients, and future research can focus on developing one for Iranian patients.
A closer look at the average QoL of cancer patients in these studies showed that it has decreased in recent years. Recent escalation of sanctions against Iran and the lack of supportive organizations have imposed greater financial burden on Iranian people and, as a result, patients face more psychological and physical stress in providing for the cost of their treatment. Therefore, insurance organizations must increase their support for these patients. Moreover, considering the prevailing religious culture of the Iranian people, it seems that by developing a comprehensive care plan that includes spiritual well-being, interventions for treating depression and anxiety in these patients may prove to be more effective.
The results showed that average QoL was higher in men and women compared to children. However, this finding is not consistent with the results of Sarukhani’s study. Saroukhani et al. showed that average QoL of cancer patients was higher in women than men [48]. Besides, in this study, QoL was higher in patients with gynecological cancer than those with other types of cancer. Given that only one study was conducted on gynecological cancer, this finding must be interpreted with caution.
This study showed that with one year increase in the patients’ age, the average QoL decreased by 0.16, which is consistent with the results of other studies [49, 50]. However, the results of studies [51, 52] showed that QoL improves with age. This may be due to cultural differences and differences in sample size. Researchers believe that illness and loneliness in older men and women exacerbate their physical problems and affect their social relationships. As a result, these problems have an adverse effect on the QoL of older men and women.
One of the limitations of this study was the use of different instruments to assess QoL among cancer patients. It prevented us from collecting sufficient information about certain variables. Also, some studies related to the QoL of cancer patients are not published in scientific journals, which may produce biased results.
Conclusion
The results of this study indicated that the average quality of life of cancer patients in Iran was moderate. Therefore, it is necessary for health managers and policymakers in Iran to take more serious measures to improve the quality of life of these patients.
Acknowledgments: -
Ethical Permissions: -
Conflicts of Interests: -
Authors’ Contributions: Isfahani P. (First Author), Introduction Writer/Main Researcher/Discussion Writer (50%); Corani Bahador R. (Second Author), Methodologist/Assistant Researcher (20%); Peirovy S. (Third Author), Statistical Analyst (20%); Afshari M. (Forth Author), Assistant Researcher (10%)
Funding/Support: -
One of the important public health problems in developing and developed countries is cancer [1]. Cancer consists of more than a hundred different diseases that affect all ethnic, racial, age, sex, economic, and social groups. According to the World Health Organization (WHO), the number of new cases of cancer increased from 10 million in 2000 to 15 million in 2020, with developing countries accounting for approximately 60 percent of the new cases. WHO also estimates that cancer-related deaths will increase from 9 million in 2015 to 11.4 million in 2030, with 7 percent of deaths occurring in low-and middle-income countries (LMICs). The annual incidence of cancer in Iran is about 70,000 cases and the annual number of cancer deaths is about 30,000. Given the increase in life expectancy and the growing elderly population in Iran, the incidence of cancer is expected to increase significantly in the coming decades [2].
Diagnosis with cancer was associated with pain, loss of function, and impending death, but today, with new treatments, it is considered a chronic disease in more than half of cases [3]. It affects all aspects of quality of life, including physical, psychological, functional, social, and economic well-being [4]. Cancer disrupts the patients’ social life, daily routines, and functions [5], making them more dependent on others and less capable of supporting others. These problems, coupled with prolonged hospitalization, frequent visits, various treatments, and high treatment costs, reduce the quality of life (QoL) of cancer patients [6]. Today, QoL has become an integral part of the evaluation criteria for cancer treatment [7].
QoL is evaluated in order to choose the optimum treatment and care for patients based on their health status and their physical, mental, and social well-being [8]. There are different definitions of QoL. For example, WHO defines QoL as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns.” [9]. Cancer affects patients' QoL to varying degrees. Problems that typically affect the QoL of cancer patients include diagnostic and therapeutic procedures, stress, pain, depression, the impact of cancer on social/family relationships, nutritional issues, and treatment-related complications [10, 11].
There have been several studies on the QoL of cancer patients in various regions of Iran. For example, the QoL of preschool children with cancer visiting a hospital in Shiraz city in 2012 was about 15.81±63.35 [12]. Moreover, in a 2009 study in Ramsar city, the QoL of cancer patients was reported to be about 31.2±8.6 [13].
However, these studies cannot provide a comprehensive view of this problem for the entire country. Integrating the results of validated studies in this area can provide better recommendations for policymakers and enable them to make evidence-based policies. Therefore, the purpose of this research was to conduct a meta-analysis of the QoL of cancer patients in Iran.
Information & Methods
This systematic review is a meta-analysis study and conducted in 2020. It followed the guidelines for preferred reporting items for systematic review and meta‑analysis (PRISMA) [14]. To identify relevant articles until December 20, 2020, researchers searched for articles published electronically in Persian databases including Scientific Information Database (SID) and Magiran as well as English databases including PubMed, Web of Science, Scopus, and Google Scholar. Persian and English keywords and a combination of these terms were used in searches. These keywords included Quality of Life, Cancer, Tumor, and Iran/Iranian along with AND/OR operators. Besides, the reference lists of published articles were examined to increase sensitivity and to find more relevant studies (Table 1). The search was initially conducted in December 2020 and then updated in August 2021, not resulting from any additional studies that faced the inclusion criteria. The articles that did not meet the following criteria were excluded: 1) studies that did not report the QoL of cancer patients; 2) letter to the editor, case-control, randomized controlled trials and qualitative studies 3) grey literature, books, and dissertations; 4) articles, documents, and reports published after December 20, 2020; 5) articles that examine the relationship between QoL and certain factors without determining the QoL of cancer patients; 6) studies that did not obtain the minimum score of 10; 7) studies published in any language other than Persian or English. On the other hand, all Persian and English cross‑sectional articles that obtained the critical score and that determined QoL among cancer patients in Iran were included.
The quality of the 30 included articles was assessed independently by two authors (first and last authors) using the 15-point instrument of Mitton et al. [15]. In this checklist, each item is given a score of 0 (not present or reported), 1 (present but low quality), 2 (present and midrange quality), or 3 (present and high quality). Disagreements were resolved through discussion or by consulting a third reviewer (first author) if necessary. Finally, only midrange and high-quality studies were included in this review and meta-analysis based on the instructions of the KTE empirical article quality rating sheet:
0 – not present or reported anywhere in the article
1 – present but low quality
2 – present and midrange quality
3 – present and high quality
________ 1. Literature Review: Directly related recent literature is reviewed and research gap (s) identified.
________ 2. Research Questions and Design: A priori research questions are stated, and hypotheses, a research purpose statement, and/or a general line of inquiry is outlined. A study design or research approach is articulated.
________ 3. Population and Sampling: The setting, target population, participants, and approach to sampling are outlined in detail.
________ 4. Data Collection and Capture: Key concepts/measures/variables are defined. A systematic approach to data collection is reported. Response or participation rate and/or completeness of information capture is reported.
________ 5. Analysis and Results Reporting: An approach to analysis and a plan to carry out that analysis is specified. Results are clear and comprehensive. Conclusions follow logically from the findings.
________ /15=Total Score
The initial search was done by the first and last authors. Then, an additional search was conducted by the third author. The data were extracted and evaluated by all authors. Finally, the final analysis was done by the first author. The duplicate articles were removed using Endnote x9 software. Extracted data included the title of the article, the first author, year of publication, average age, sample size, instrument, statistical population, methodology, location of study, and QoL, and an Excel 2016 spreadsheet was used for data entry. The initial search resulted in 5,686 articles. After excluding duplicates and irrelevant articles, 3,138 studies were selected for abstract examination. After reviewing the abstracts, 3,085 articles were removed. Also, 23 articles were removed after examining the full texts as they did not report the mean±SD values for the QoL of cancer patients. Finally, 30 studies [13, 16-44] were found eligible for inclusion in the meta-analysis (Diagram 1).
Data were analyzed using the Comprehensive Meta-Analysis (CMA) software version 2.2.064 (the US, Biostat Inc.). The heterogeneity of the studies was assessed using Cochran’s Q-test statistics and I2 test. Strong evidence of heterogeneity was observed (I2=99.94, p<0.05), and, thus, a random-effects model was used to synthesize their results. The funnel plot and Egger’s test were used to assess the likelihood of publication bias, and the results showed that publication bias was not statistically significant (p=0.055). Finally, the effect of variables that could be the potential sources of heterogeneity was examined using the meta-regression technique. Point estimates of QoL in cancer patients were calculated in forest plots at the 95% confidence interval, where the size of the box indicates the weight of each study and the lines on its sides represent the 95% CI.
Table 1) Search stages
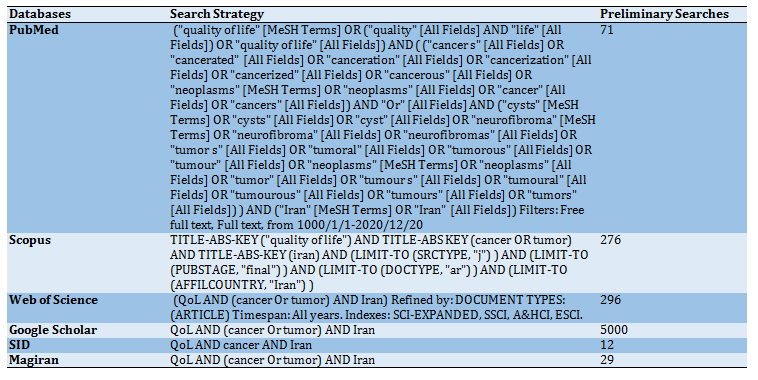
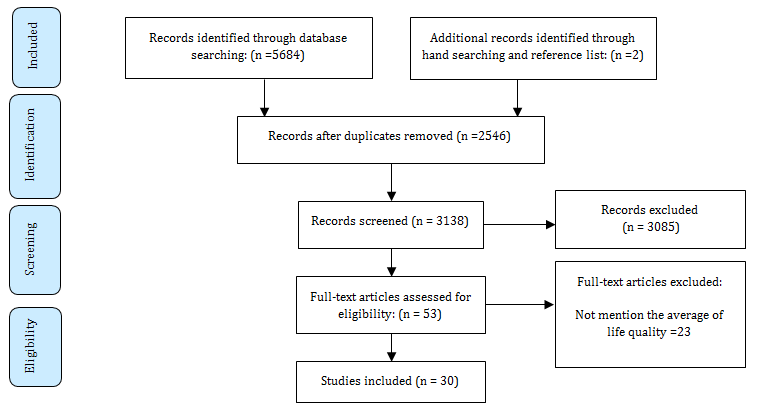
Diagram 1) PRISMA flow chart for study selection
Findings
Most of these studies were conducted in 2010 and 2011. More than half of these studies were published after 2009 (Diagram 2). Most studies were done in Tehran, Gilan, and Qazvin provinces (Diagram 3).
Based on the random-effects model, the average QoL of cancer patients was 50.83±3.07 (44.80-56.86; 95% CI). The highest QoL was observed in the city of Qazvin in 2012 at 103.07±1.61 (100.11-106.03: 95% CI) and the lowest QoL was observed in the city of Tehran in 2010 at 4.05±0.36 (3.35-4.75: 95% CI) (Table 2).
The results were summarized by sample size, studies quality, studied population, cancer type, questionnaire type, and geographic region (Table 3). The mean QoL of cancer patients was higher in the eastern region of Iran. Patients with genital cancer had a better QoL than those with other types of cancer. The mean QoL was higher in men and women than children. Moreover, studies with sample sizes greater than 100 reported higher mean values. Finally, studies with midrange quality reported higher mean values than those with higher quality. Higher QoL scores were reported using the McGill questionnaire than other instruments.
The results of evaluating heterogeneity indicated a high level of heterogeneity among the included studies (Q=48605.498; p=0.0001). Thus, a meta-regression model was used to identify the variables that could potentially cause heterogeneity. The results showed in Table 4 and Diagram 4 indicate that sample size, publication year, and average age contributed to the heterogeneity of studies on the QoL in Iranian cancer patients. The results revealed that the QoL of Iranian cancer patients has decreased by 2.48% each year. One year increase in patients’ age decreased QoL by 0.16. Moreover, the results showed that one unit increase in sample size has increased QoL by 0.17 in Iranian cancer patients.
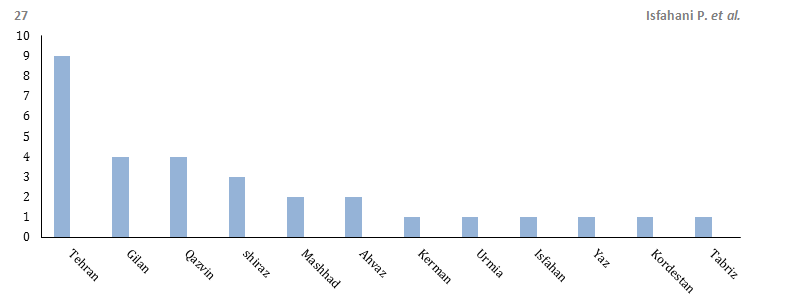
Diagram 3) Frequency distribution of studied QoL among cancer patients
Table 2) Results of forest plot for 31 studies
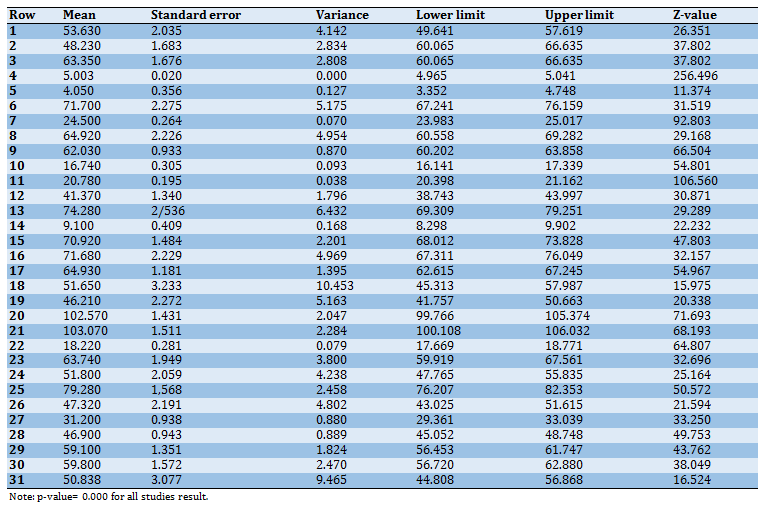
Table 3) Subgroup analyses of the included studies
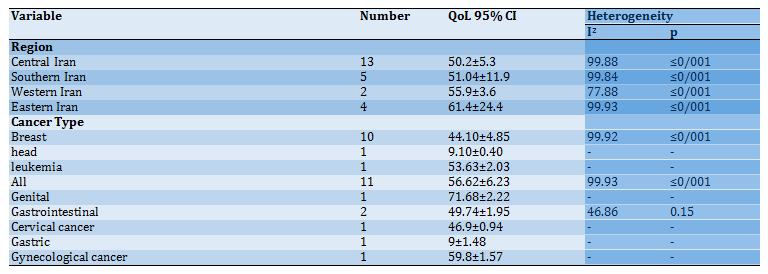
Continue of Table 3) Subgroup analyses of the included studies
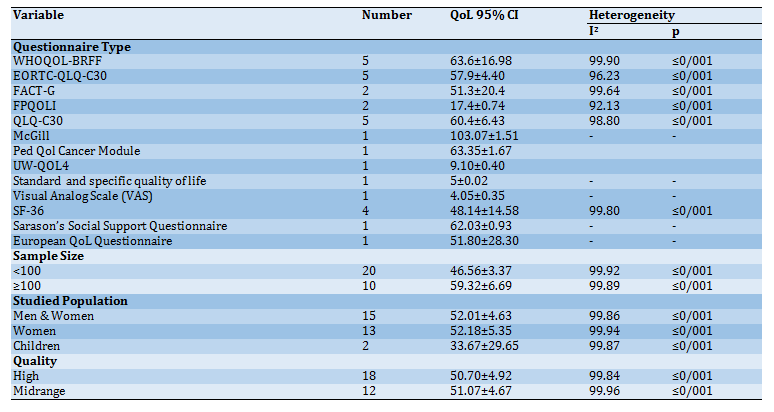
Table 4) Results of meta-regression
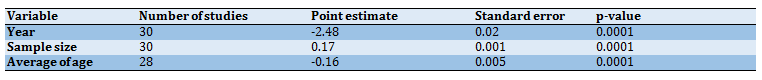
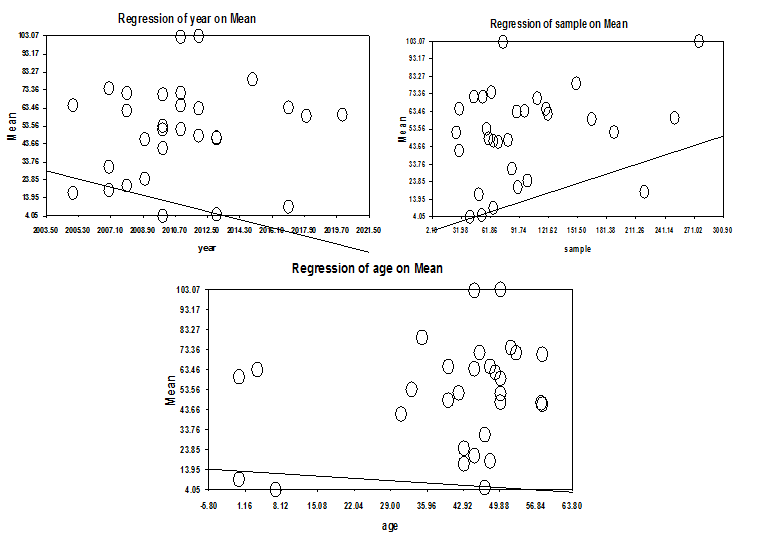
Diagram 4) Results of meta-regression
Discussion
The purpose of this study was to determine the QoL of cancer patients in Iran. By examining eight databases, 30 relevant articles were identified. The overall average QoL of Iranian cancer patients was 50.83±3.07. Several studies have examined the QoL of cancer patients worldwide. For example, the average QoL of cancer patients was reported to be 105±12.93 in cancer hospitals of Karnataka in 2017 [45] and 6.88±1.41 in Chennai women with cervical cancer [46]. The QoL of cancer patients varies. The difference in studies is because of the difference in culture, context, population, the conditions of this disease, and treatment process. Cancer can result in different types of changes in the life of cancer patients [47].
The present research showed that one unit increase in sample size increased the average QoL of cancer patients by 0.17. In other words, studies that use a small sample unintentionally create sampling bias and, as a result, cannot provide valuable information for health policymakers and managers. Therefore, studies on the QoL of cancer patients must use a representative sample and employ appropriate sampling techniques.
In the present study, the mean QoL score of cancer patients varied in different regions of Iran. That is, the mean QoL score of cancer patients was 43.4 in six studies in the northern region, 51.6 in one study in the western region, 49.6 in 11 studies in the central region was, 51.04 in five studies in the southern region, and 61.4 in four studies in the eastern region. Therefore, the average QoL of cancer patients was higher in eastern Iran compared to other regions of the country. However, the QoL of cancer patients has been investigated only in a limited number of Iran’s provinces. Therefore, these studies have not been extensive and this gap can be filled in future research.
In recent years, several studies have been conducted on the QoL of cancer patients. However, the results of these studies showed large dispersion and heterogeneity. Another key factor is the instrument t used to measure QoL among cancer patients. Given that there are a variety of instruments, the QoL of cancer patients has been measured differently. Therefore, differences between the results of the reviewed studies can be, in part, due to differences in the instrument used to measure this variable. In this article, the average QoL of cancer patients was higher when using the McGill questionnaire than other instruments. Overall, there is no comprehensive questionnaire for measuring the QoL of cancer patients, and future research can focus on developing one for Iranian patients.
A closer look at the average QoL of cancer patients in these studies showed that it has decreased in recent years. Recent escalation of sanctions against Iran and the lack of supportive organizations have imposed greater financial burden on Iranian people and, as a result, patients face more psychological and physical stress in providing for the cost of their treatment. Therefore, insurance organizations must increase their support for these patients. Moreover, considering the prevailing religious culture of the Iranian people, it seems that by developing a comprehensive care plan that includes spiritual well-being, interventions for treating depression and anxiety in these patients may prove to be more effective.
The results showed that average QoL was higher in men and women compared to children. However, this finding is not consistent with the results of Sarukhani’s study. Saroukhani et al. showed that average QoL of cancer patients was higher in women than men [48]. Besides, in this study, QoL was higher in patients with gynecological cancer than those with other types of cancer. Given that only one study was conducted on gynecological cancer, this finding must be interpreted with caution.
This study showed that with one year increase in the patients’ age, the average QoL decreased by 0.16, which is consistent with the results of other studies [49, 50]. However, the results of studies [51, 52] showed that QoL improves with age. This may be due to cultural differences and differences in sample size. Researchers believe that illness and loneliness in older men and women exacerbate their physical problems and affect their social relationships. As a result, these problems have an adverse effect on the QoL of older men and women.
One of the limitations of this study was the use of different instruments to assess QoL among cancer patients. It prevented us from collecting sufficient information about certain variables. Also, some studies related to the QoL of cancer patients are not published in scientific journals, which may produce biased results.
Conclusion
The results of this study indicated that the average quality of life of cancer patients in Iran was moderate. Therefore, it is necessary for health managers and policymakers in Iran to take more serious measures to improve the quality of life of these patients.
Acknowledgments: -
Ethical Permissions: -
Conflicts of Interests: -
Authors’ Contributions: Isfahani P. (First Author), Introduction Writer/Main Researcher/Discussion Writer (50%); Corani Bahador R. (Second Author), Methodologist/Assistant Researcher (20%); Peirovy S. (Third Author), Statistical Analyst (20%); Afshari M. (Forth Author), Assistant Researcher (10%)
Funding/Support: -
Article Type: Systematic Review |
Subject:
Quality of Life
Received: 2021/05/22 | Accepted: 2021/08/29 | Published: 2021/01/24
Received: 2021/05/22 | Accepted: 2021/08/29 | Published: 2021/01/24
References
1. Jitender S, Mahajan R, Rathore V, Choudhary R. Quality of life of cancer patients. J Exp Ther Oncol. 2018;12(3):217-21. [Link]
2. Nassehi A, Abbaszadeh A, Borhani F, Arab M, Samareh Fekri M, Jafari M. Effect of two educational models based on compliance and empowerment on the quality of life of patients with asthma. J Nurs Educ. 2013;2:1-7. [Persian] [Link]
3. Compbel HS, Phaneuf MR, Deane K. Cancer peer support programs- do they work?. Patient Educ Couns. 2004;55(1):3-15. [Link] [DOI:10.1016/j.pec.2003.10.001] [PMID]
4. Courtens AM, Stevens FC, Crebolder HF, Philipsen H. Longitudinal study and quality of life and social support in cancer patients. Cancer Nurs. 1996;19(3):162-9. [Link] [DOI:10.1097/00002820-199606000-00002] [PMID]
5. Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychol. 1996;15(2):135-48. [Link] [DOI:10.1037/0278-6133.15.2.135]
6. Shell GA, Kirs CH. Psychosocial issues, outcomes, and quality of life. In: Otto SE, editor. Oncology Nursing. 4th Edition. St. Louis: Mosby a Aharcourt Health Sciences Company; 2001. pp. 948-70. [Link]
7. Lee SJ, Earle CC, Weeks JC. Outcomes research in oncology: history, conceptual framework, and trends in the literature. J Natl Cancer Inst. 2000;92(3):195-204. [Link] [DOI:10.1093/jnci/92.3.195] [PMID]
8. Leininger M. Quality form a transcultural nursing perspective. Nurs Sci Q. 1994;7:22-28. [Link] [DOI:10.1177/089431849400700109] [PMID]
9. Park K. Park's Textbook of preventive and social medicine. 23rd Edition. Banarsidas Bhanot Publishers; 2015. [Link]
10. Safaee A, Zeighami B, Tabatabaee H, Moghimi Dehkordi B. Quality of life and related factors in breast cancer patients under chemotherapy. Iran J Epidemiol. 2008;3(3&4):61-6. [Persian] [Link] [DOI:10.4103/0019-509X.44066] [PMID]
11. Shakeri J, Abdoli N, Paianda M, Chareh-Ga G. The frequency distribution of depression among patients with breast cancer in Kermanshah u.m.s chemotherapy centers in 2007. J Med Council Islamic Repub Iran. 2009;27:324-8. [Persian] [Link]
12. Rahimi S, Fadakar Soghe R, Tabri R, Kazemnezhad Leili E. Related factors with quality of life among preschool chil-dren with cancer. J Holist Nurs Midwifery. 2014;24(1):30-9. [Persian] [Link]
13. Ghaffari F, Fotokian Z, Karimi M, Keihanian Sh, Karimi HE. The relationship between anemia-related fatigue and quality of life in cancer patients. J Inflamm Dis. 2009;13(1):34-41. [Persian] [Link]
14. Moher DL, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‑analyses: the PRISMA statement. BMJ. 2009;339:b2535 [Link] [DOI:10.1136/bmj.b2535] [PMID] [PMCID]
15. Mitton C, Adair CE, McKenzie E, Patten SB, Waye Perry B. Knowledge transfer and exchange: review and synthesis of the literature. Milbank Q. 2007;85(4):729-68. [Link] [DOI:10.1111/j.1468-0009.2007.00506.x] [PMID] [PMCID]
16. Jelodari S, Sodagar S, Bahrami Hidaji M, Tajeri B. Orientation of life, quality of life and perceived social support in people with acute lymphocytic and acute myeloid leukemia. Health Psychol. 2019;8(29):7-24. [Persian] [Link]
17. Haghighat S. The effect of Reflexology on quality of life of breast cancer patients during chemotherapy. Iran J Breast Dis. 2013;6:23-34. [Persian] [Link]
18. Rahimi S, Fadakar Soghe K, Tabari R, Kazem Nejad Lili E. Relationship between mother's general health status with quality of life of child with cancer. J HAYAT. 2013;19(2):93-108. [Persian] [Link]
19. Sharifi M, Baghaii R, Mohammadpour Y, Mikaili P, Sheikhi N. The effect of chemotherapy on functional scales of quality of life of patient with breast cancer. J Breast Disease Iran. 2013;6:26-34. [Persian] [Link]
20. Farrokhnia M, Shahidi S, Fathabadi J. The impact of cognitive interventions in reducing intensity of pain and distress, and improving quality of life of children with cancer. Basic Clin Cancer Res. 2013;5:16-22. [Link]
21. Azh N. Effects of training on the care and treatment of breast cancer commonly referred to Kosar hospital ecology in 1391-1390. Iran J Breast Dis. 2012;5(2&3):60-70. [Persian] [Link]
22. Shoakazemi M, Mehravar Momeni J. The relationship between quality of life and hope of life in cancer patients after surgery. Iran J Breast Dis. 2009;2(2&3):20-7. [Persian] [Link]
23. Safaei A, Dehkordi Moghimi B, Tbatabaei SHR. Reliability and validity of the QLQ-C30 questionnaire in cancer patients. J Bring Knowl. 2007;12(2):79-87. [Persian] [Link]
24. Mohammadi SZ, Houshmand P, Djafari F, Esmaily H, Kooshyar MM. The relationship between anemia and severity of fatigue and quality of life in cancer patients undergoing chemotherapy. J Med Sci Islamic Azad Univ. 2010;20(4):265-72. pe [Link]
25. Fazel AZ, Tirgari B, Mokhber N, Koushyar MM, Esmaily H. The effect of mastectomy on mood and quality of life in breast cancer patients. J Shahid Sadoughi Univ Med Sci Health Serv. 2008;16:28-36. [Persian] [Link]
26. Mardani Hamule M, Shahraki Vahed A. Investigate the relationship between mental health and quality of life in cancer patients. J Res Hamedan Univ Med Sci Health Ther Serv. 2009;16:79-87. [Persian] [Link]
27. Hamid N, Ahmadian A, Akbari Shaye Y. Effectiveness of cognitive behavior therapy based on religious believes on hope and Quality in the patients suffering from breast cancer. Med J Hormozgan. 2012;16(3):213-21. [Persian] [Link]
28. Karami O, Felahatpishe F, Jahani Hashemi H, Byraghdar N. Quality of patients with cancer in Qazvin. J Inflamm Dis. 2011;14(3):80-6. [Link]
29. Zamanzadeh M, Asgari S, Moosazadeh M, Moslemi D, Torabi M. Assessment of quality of life in patients with head and neck cancers. J Mazandaran Univ Med Sci. 2018;27(158):132-42. [Persian] [Link]
30. Momeni M, Ghanbari Khanghah A, Joukar F, Kazem Nezhad Leili E. Predictive Factors of quality of life in patients with colorectal cancer. J Holist Nurs Midwifery. 2012;22(1):44-53. [Persian] [Link]
31. Rezaei R, Saatsaz S, Haji Hosseini F, Sharifnia S, Nazari R. Quality of life in gynecologic cancer patients before and after chemotherapy. J Babol Univ Med Sci. 2011;13(4):78-84. [Persian] [Link]
32. Estakhri Z, Tajikzadeh F, Kazemi SA. Comparison of the role of religious beliefs in hopefulness and quality of life among cancer and non-cancer patients. J Relig Health. 2017;4(2):1-11. [Persian] [Link]
33. Esmailnasab N, Taymoori P, Darabi F. Comparison of quality of life 3 and 9 months after surgery in patients with gastrointestinal cancer. Stud Med Sci. 2013.24(4):226-34. [Persian] [Link]
34. Pakpour A, Panahi D, Yekaninejad S, Norozi S. Assessment of quality of life in patient with esophagus cancer. Health Monit. 2010;8(4):371-8. [Persian] [Link]
35. Bahrami N, Moradi M, Soleimani M, Kalantari Z, Hosseini F. Death anxiety and its relationship with quality of life in women with cancer. Iran J Nursing. 2013;26(82):51-61. [Persian] [Link]
36. Bahrami B, Bahrami A, Mashhadi A, Kareshki H. The role of cognitive emotion-regulation strategies in the quality of life of cancer patients. Med J Mashhad Univ Med Sci. 2015;58(2):69-501. [Persian] [Link]
37. Heiydari S, Salahshorian A, Rafie F, Hoseini F. Correlation of perceived social support and size of social network with quality of life dimension in cancer patients. FEYZ. 2008;12(2):15-22. [Persian] [Link]
38. Sadoughi M, Mehrzad V, Mohammad Salehi Z. The relationship between psychological capital and quality of life among patients with breast cancer. Razi J Med Sci. 2017;4(156):111-9. [Persian] [Link] [DOI:10.46886/IJARP/v4-i1/2602]
39. Saffari M, Zeidi IM, Pakpour AH. Role of religious beliefs in quality of life patients with cancer. Hakim Res J. 2012;15(3):243-50. [Link]
40. Safari M, Azizi Zadeh Forozy M, Tirgari B, Jahanim Y. Relationship between quality of life and spiritual needs of cancer patients. J Cultivar Med. 2016;25(3):199-212. [Persian] [Link]
41. Alaghband M, Servat F, Zarepour F. Investigation of the relationship between quality of life and life expectancy in patients with breast cancer. J TOLOO-E-BEHDASHT. 2016;15(2):175-85. [Persian] [Link]
42. Torkzahrani S, Rastegari L, Khodakarami N, Akbarzadeh-Baghian A, Alizadeh K. Quality and its related factors among Iranian cervical cancer survivors. Iran Red Crescent Med J. 2013;15(4):320-3. [Link] [DOI:10.5812/ircmj.4410] [PMID] [PMCID]
43. Sehati Shafaee F, Mirghafourvand M, Harischi S, Esfahani A, Amirzehni J. Self-confidence and Quality of life in women undergoing treatment for breast cancer. Asian Pac J Cancer Prev. 2018;19(3):733-40. [Link]
44. Shirali E, Yarandi F, Ghaemi M, Montazeri A. Quality of life in patients with gynecological cancers: a web-based study. Asian PacJ Cancer Prev. 2020;21(7):1969. [Link] [DOI:10.31557/APJCP.2020.21.7.1969] [PMID] [PMCID]
45. Nayak MG, George A, Vidyasagar MS, Mathew S, Nayak S, Nayak BS, et al. Quality of life among cancer patients. Indian J Palliat Care. 2017;23(4):445-50. [Link] [DOI:10.4103/IJPC.IJPC_82_17] [PMID] [PMCID]
46. Hemavathy V, Julius A. A study to assess the quality of life among women with cervical cancer in selected hospitals at Chennai. Int J Pharm Bio Sci. 2016;7(4):722-4. [Link] [DOI:10.22376/ijpbs.2016.7.4.b722-724]
47. Kumari R, Kaur J, Kajal M. A review on quality of life in cancer patients: an Indian scenario. Int J Cur Res Rev. 2017;9(15):45-8. [Link]
48. Saroukhani D, Omidi K, Norouzi R, Zali H, Sayehmiri K, Forozeshfard M. The quality of life in cancer patients in Iran: a systematic review by using meta-analysis. KOOMESH. 2016;18(1):1-2. [Persian] [Link]
49. Ohsumi S, Shimozuma K, Morita S, Hara F, Takabatake D, Takashima S, et al. Factors associated with health-related quality-of-life in breast cancer survivors: influence of the type of surgery. Jpn J Clin Oncol. 2009;39(8):491-6. [Link] [DOI:10.1093/jjco/hyp060] [PMID]
50. Ganz PA, Guadagnoli E, Landrum MB, Lash T L, Rakowski W, Silliman Rebecca A. Breast cancer in older women: QUALITY and psychosocial adjustment in the15 months after diagnosis. J Clin Oncol. 2003;21(21):4027-33. [Link] [DOI:10.1200/JCO.2003.08.097] [PMID]
51. Smith AW, Alfano CM, Reeve BB, Irwin ML, Bernstein L, Baumgartner K, et al. Race/ethnicity, physical activity, and quality of life in breast cancer survivors. Cancer Epidemiol Biomark Prev. 2009;18(2):656-63. [Link] [DOI:10.1158/1055-9965.EPI-08-0352] [PMID] [PMCID]
52. Redhwan AA, Md Idris MN, Zaleha MI, Robert C, Fuad I, Sami RA. Quality of life among women with breast cancer from universiti kebangsaan malaysia medical centre, malaysia. Malaysian J Community Health. 2008;14(2):46-55. [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





