Volume 9, Issue 3 (2021)
Health Educ Health Promot 2021, 9(3): 171-175 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ebadi A, Moayed M, Mirsadeghi A, Saeid Y. Evaluating Intensive Care Nurses' Clinical Competence in Eye Care; a Cross-Sectional Descriptive Study. Health Educ Health Promot 2021; 9 (3) :171-175
URL: http://hehp.modares.ac.ir/article-5-49343-en.html
URL: http://hehp.modares.ac.ir/article-5-49343-en.html
1- “Behavioral Science Research Center, Life style institute” and “Nursing Faculty”, Baqiyatallah University of Medical Sciences, Tehran, Iran
2- Trauma Research Center, Faculty of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- MSc of Nursing, Faculty of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran
4- Trauma Research Center, Faculty of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran , yasernurse84@yahoo.com
2- Trauma Research Center, Faculty of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- MSc of Nursing, Faculty of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran
4- Trauma Research Center, Faculty of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran , yasernurse84@yahoo.com
Full-Text [PDF 384 kb]
(1459 Downloads)
| Abstract (HTML) (1850 Views)
Full-Text: (848 Views)
Introduction
The ocular surface disease is common in the intensive care population. The ocular surface is normally protected by the ability to produce tears, blink, and close the eyes with rest or sleep. These mechanisms can be disrupted in intensive care patients, increasing the risk of developing [1]. The patients hospitalized in intensive care units (ICU) usually receive sedative-hypnotic medications that impair the protective mechanisms of the eyes, such as blinking and tear production [2, 3]. Accordingly, they are fairly prone to lagophthalmos (incomplete closure of the eyes) and subsequent eye disorders such as eye dryness, exposure to keratopathy, corneal abrasion, and infectious keratitis [4-6]. Accordingly, besides mechanical ventilation-induced chemosis, these patients are also greatly at risk for Ocular surface disease [6, 7]. The prevalence of eye disorders such as keratopathy, microbial keratitis, chemosis to range from 3–80% [8-11], dry eye syndrome 33.3%, eye infections 89.3% has been reported among ICU patients [12]. Eyecare is an important aspect of managing critically ill patients, as many of the mechanisms normally involved in protecting the eye from infection and injury are compromised. Nurses have a critical role in preventing and managing ICU patients' eye disorders [13, 14], and regular assessment of ICU patients' eyes can help the early diagnosis and applying the methods of preventing eye disorder [15]. Eyecare, a neglected area in critically ill patients, is an important component of holistic patient care in ICU; they mainly focus on managing life-threatening conditions and maintaining the functions of vital organs and hence pay little attention to eye care [4, 16, 17]. Therefore, nurses need to have considerable knowledge of and great competence in carefully assessing and correctly diagnosing patients' eye problems. However, research findings show that ICU nurses have limited knowledge and competencies in eye care [18]. In the study in two teaching hospitals on day 5, 32.2% of patients had dry eyes, and 13.8% of patients had developed corneal abrasion; these results indicated eye care was neglected and weak for ICU patients [19]. Some researchers reported that ICU staff did not have sufficient knowledge to provide eye care and that lack of knowledge, attitudes, and skills can be considered a barrier to providing eye care [20]. Another study illustrated that many participants had weak knowledge about patient eye care and regular eye visits and paid more attention to treatment than prevention [21].
Little is still known about nurses' eye care knowledge, attitude, and practice. Lack of eye care studies in critically ill patients is a common issue globally, especially in Iran. This study aimed to evaluate ICU nurses' clinical competence (Knowledge, Attitude, and Practice) in eye care.
Instrument & Methods
This secondary analysis study (of psychometric study) was conducted in 2015. The study setting was ten teaching hospitals located in Tehran, Shiraz, Qom, and Kerman cities located in Iran. Ten hospitals were selected by cluster sampling of 4 cities in Iran, 432 intensive care nurses were recruited by convenience sampling. The sample size was determined based on the standard criteria identifying a minimum sample size for factor analysis, which was 5-10 times more than the number of items calculated in the primary study for scale development. The inclusion criteria were having at least one year of work experience in ICU and holding a university degree in nursing.
Data collection was a two-part questionnaire including demographic characteristics (gender, age, university degree, passed specialized intensive care courses, having eye care guidelines in the ward etc.) and previously validated Eye Care Competence Inventory. Study data were collected by using a previously validated Eye Care Competence Inventory [22]. Eye Care Competence Inventory (ECCI) consists of 35 items in three domains: knowledge, attitude, and practice. The knowledge domain comprises 18 multiple-choice questions on nurses' knowledge of eye disorders, risk factors for eye disorders, and eye care. Right and wrong answers are scored 0 and 1, respectively. The attitude and practice domains consist of 7 and 10 items respectively on nurses' eye care attitude and practice scored on a 5point Likert scale (from 1 to 5). The possible total scores of these two domains are 7-35 and 8-40. For better judgment and understanding, the ECCI domains in our study ranged from 0 to 100. Accordingly, higher scores equated to greater knowledge and better attitude and practice (less: lower than 33.3, moderate: between 33.3-66.6, good: further than 66.7). The Kuder-Richardson coefficient of the knowledge domain and the Cronbach's alphas of the attitude and practice domains and the whole inventory was 0.76, 0.85, and 0.83. The Kuder-Richardson coefficient was used for evaluating the internal consistency of the knowledge domain because the items of this domain were scored dichotomously. On the other hand, the stability of the questionnaire was assessed by using the test-retest method. Accordingly, a sub-sample of 18 nurses invited to complete the questionnaire twice with a 15-day interval and calculated the Interclass Correlation Coefficient. The test-retest interclass correlation coefficient was good (ICC=0.69) [21].
The approval code was from Baqiyatallah University of Medical Science. Study participants were informed of the study aim. Participation in the study was completely voluntary. The researchers ensured the confidentiality of the study participants provided data. Before the questionnaire was distributed to the nurses in each ICU, a researcher associated with each ICU explained the purpose of the study and received verbal informed consent from nurses. Nurse participants completed the questionnaire in the ICU of their respective hospital between September 2015 and June 2015. The researchers distributed and collected the questionnaire.
Study data were analyzed by using the Statistical Package for Social Sciences (SPSS v. 18.0). Nurses' eye care knowledge, attitude, and practice scores were presented using descriptive measures such as mean and standard deviation. Primarily, the normality of the study variables was assessed by performing the Kolmogorov-Smirnov test. Consequently, the independent-samples t-test was used for between-group comparisons of knowledge, attitude, and practice scores regarding variables such as gender, presence of eye care guidelines in the ward, intensive care license, and passing the infection control course. Moreover, the Pearson product-moment correlation test was employed for examining the correlation between nurses' eye care competence, age, and work experience.
Findings
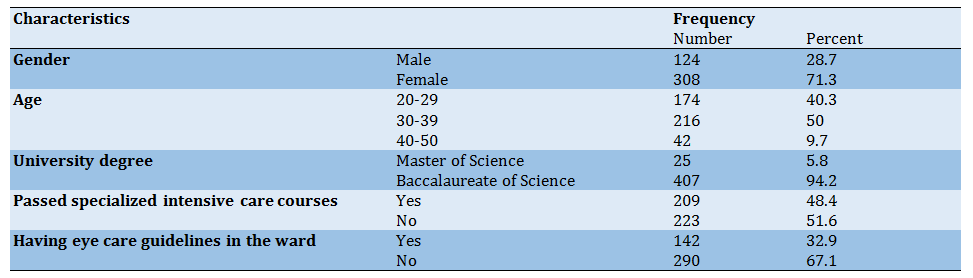
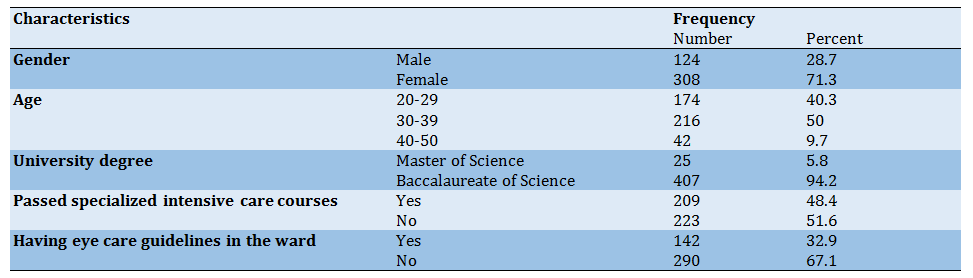
Only 432 intensive care nurses had filled out the questionnaires completely (Response Rate 93%). The mean±SD of nurses' age was 32.6±5.6 years participated in the study. Most of the study participants were female (71.3%) and held bachelor's degrees in nursing (94.2%). The study participants’ characteristics showed in Table 1.
Table 1) Selected participant demographic characteristics (n=432)
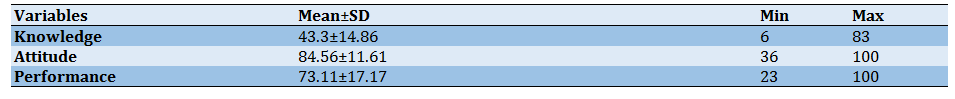
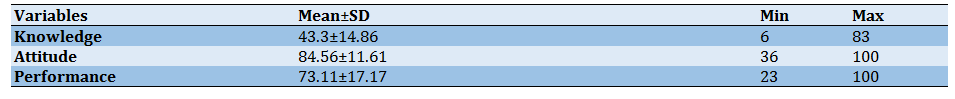
The mean±SD scores for eye care knowledge, attitude, and practice showed in Table 2. The independent-samples t-test revealed that female nurses had a better eye care practice than male nurses (p<0.05). However, male and female nurses did not differ significantly concerning eye care knowledge and attitude.
Table 2) The mean±SD of nurses' clinical competence scores (Range of Score 0 – 100 and N=432)
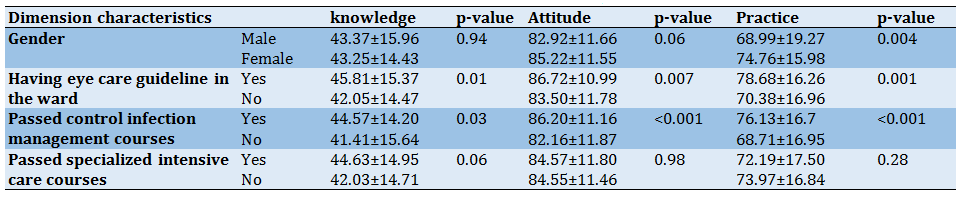
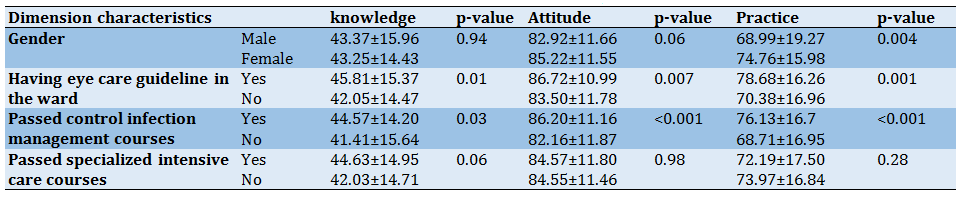
The nurses who had such guidelines in their ward acquired significantly higher eye care knowledge, attitude, and practice scores than those who did not have guidelines (p<0.05; Table 3).
Table 3) The mean±SD difference between domains of the ECCI and Socio-demographic characteristics
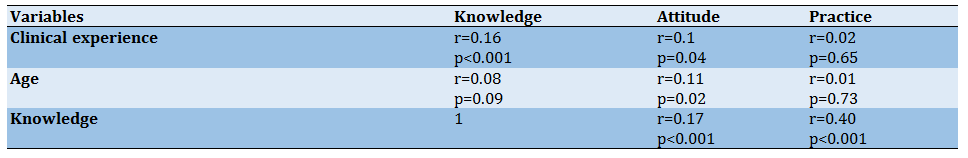
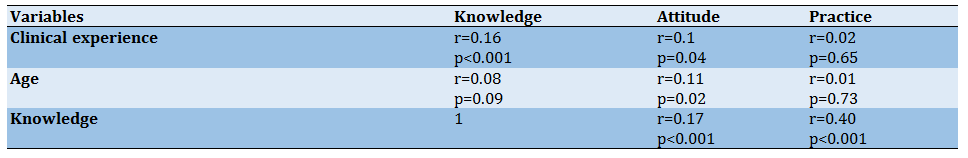
Nurses' work experience positively correlated with their eye care knowledge and attitude. There also was a significant positive correlation between nurses' age and their eye care attitude. Finally, knowledge had significant positive correlations with attitude and practice (p<0.001; Table 4).
Table 4) Correlation between of three domains of the ECCI and Socio-demographic characteristics
Discussion
We conducted this study to evaluate ICU nurses' clinical competence in eye care. Accordingly, we assessed ICU nurses' eye care knowledge, attitude, and practice. Our findings revealed that the study participants had limited eye care knowledge. Some of the studies were reported the same finding [12, 23, 24]. This can be attributed to ICU nurses' greater involvement with managing life-threatening conditions and maintaining the functions of vital organs and their subsequent little attention to eye care [4]. Despite these results, Fulbrook et al., [18], and Jansson et al. [25] illustrated that the nurses in their studies had good knowledge. This contradiction is probably because we were mainly concerned with evaluating ICU nurses' knowledge of intensive care in general and ventilator-associated pneumonia, respectively.
An interesting finding of the study was that our participating nurses had a positive attitude towards providing eye care despite having limited eye care knowledge. None of the previous studies dealt with nurses' eye care attitude to the best of our knowledge.
Another finding of the study was that while our participants had limited eye care knowledge, they followed a good eye care practice. This finding poses this challenging question: how can nurses, who have limited knowledge, follow a sound practice? To respond to this question probably, our nurses provided eye care more based on their clinical experiences and established routines than their professional knowledge. Therefore, eye care must be incorporated into critical care training programs for ICU nurses to support the delivery of quality patient care. Another reason behind this finding is that we used a self-report questionnaire that subjectively evaluated nurses' eye care practice.
This finding conflicts with the findings of Vyas, who reported that ICU nurses had poor eye care performance. This conflict between the two studies' findings is probably because we used a self-report questionnaire while Vyas evaluated nurses' practice by using an observational performance checklist [24]. Further studies must evaluate nurses' eye care practice by using both self-report questionnaires and observational performance checklists.
We also found that compared with male nurses, female nurses obtained significantly higher eye care practice scores. However, there was no statistically significant difference between male and female nurses' eye care knowledge and attitude. These findings conflict with Yousefi et al., which can be attributed to the difference in the studies' measurement tools and unequal gender distribution [25]. Study findings also revealed a significant positive correlation between nurses' work experience and their eye care knowledge and attitude. Other studies also reported the same finding [12, 18, 26]. However, this finding contradicts some of the research findings that no relationship between work experience and KAP eye care [24, 26, 27].
We also found that nurses' age did not significantly correlate with their eye care knowledge and practice. This finding is in line with the findings of the previous studies [26]. However, there was a significant positive correlation between nurses' age and their eye care attitude. This can be due to more clinical experience in older nurses, which leads to a positive attitude towards eye care in ICU patients. On the other hand, the younger nurses should be given appropriate training in eye care.
The study showed that nurses' eye care knowledge significantly correlated with their eye care attitude and practice. Other studies also reported the same finding [27, 28]. Moreover, nurses who had access to eye care guidelines in their ward acquired significantly higher eye care knowledge, attitude, and practice scores than their counterparts who did not have such guidelines. This finding is consistent with the findings of the previous studies [29, 30]. ICU nurses' greater involvement with managing life-threatening situations can be an obstacle for attending to less important aspects of care such as eye care. However, clear guidelines can remind nurses of the importance and the necessity of providing eye care.
We also found no significant differences between the eye care knowledge, attitude, and practice scores of nurses who had passed specialized intensive care courses and the nurses who had not passed such courses. Celik et al. [31] also reported the same finding. These courses probably mainly focus more on the assessment and management of life-threatening conditions than the other aspects of care such as eye care. Therefore, Eyecare education necessary for ICU nurses, especially inexperienced nurses in intensive care unit nursing, and provide continuing education on the latest eye care methods and information to experienced nurses. Accordingly, this study shows absent or insufficient eye care education for critically ill patients in ICU nursing training programs in Iran. So that, eye care should be incorporated into critical care education programs for ICU nurses to deliver quality patient care.
Finally, nurses who had passed control infection management courses obtained significantly higher eye care knowledge, attitude, and practice scores than those who had not taken such courses. Yousefi et al. also reported the same finding. This finding can be attributed to the stronger awareness and greater sensitivity of nurses who take these courses regarding the importance of infection management [26].
A self-report questionnaire was used for evaluating nurses' eye care practice. Self-report questionnaires provide a subjective assessment of practice. Accordingly, verifying the accuracy of self-report questionnaires by using observational checklists as well as employing observational checklists for eye care practice evaluation are recommended. Given its Likert-type scale, ECCI can develop observational checklists to evaluate nurses' eye care practice objectively.
Conclusion
The result showed that nurses' knowledge in eye care of ICU patients was moderate and attitude and practice, intensive care nurses' eye care were good. Given the direct correlation between nurses' eye care knowledge and their eye care attitude and practice, enhancing their knowledge would also positively influence their attitude and practice.
Acknowledgments: The authors grateful to the Faculty of Nursing and trauma research center, Baqiyatallah University of Medical Sciences and the authorities of hospitals and all the nurses working in these hospitals who kindly cooperated in conducting this research.
Ethical Permissions: IRB approval number: IR.BMSU.RECH.1392.26
Conflicts of Interests: We declare that we have no conflicts of interest.
Authors’ Contribution: Ebadi A. (First Author), Methodologist/Statistical Analyst (25%); Moayed M.S. (Second Author), Introduction Writer, Discussion Writer (25%); Mirsadeghi A. (Third Author), Introduction Writer (25%); Saeid Y. (Forth Author) Assistant Researcher (25%).
Funding/Support: No funding.
The ocular surface disease is common in the intensive care population. The ocular surface is normally protected by the ability to produce tears, blink, and close the eyes with rest or sleep. These mechanisms can be disrupted in intensive care patients, increasing the risk of developing [1]. The patients hospitalized in intensive care units (ICU) usually receive sedative-hypnotic medications that impair the protective mechanisms of the eyes, such as blinking and tear production [2, 3]. Accordingly, they are fairly prone to lagophthalmos (incomplete closure of the eyes) and subsequent eye disorders such as eye dryness, exposure to keratopathy, corneal abrasion, and infectious keratitis [4-6]. Accordingly, besides mechanical ventilation-induced chemosis, these patients are also greatly at risk for Ocular surface disease [6, 7]. The prevalence of eye disorders such as keratopathy, microbial keratitis, chemosis to range from 3–80% [8-11], dry eye syndrome 33.3%, eye infections 89.3% has been reported among ICU patients [12]. Eyecare is an important aspect of managing critically ill patients, as many of the mechanisms normally involved in protecting the eye from infection and injury are compromised. Nurses have a critical role in preventing and managing ICU patients' eye disorders [13, 14], and regular assessment of ICU patients' eyes can help the early diagnosis and applying the methods of preventing eye disorder [15]. Eyecare, a neglected area in critically ill patients, is an important component of holistic patient care in ICU; they mainly focus on managing life-threatening conditions and maintaining the functions of vital organs and hence pay little attention to eye care [4, 16, 17]. Therefore, nurses need to have considerable knowledge of and great competence in carefully assessing and correctly diagnosing patients' eye problems. However, research findings show that ICU nurses have limited knowledge and competencies in eye care [18]. In the study in two teaching hospitals on day 5, 32.2% of patients had dry eyes, and 13.8% of patients had developed corneal abrasion; these results indicated eye care was neglected and weak for ICU patients [19]. Some researchers reported that ICU staff did not have sufficient knowledge to provide eye care and that lack of knowledge, attitudes, and skills can be considered a barrier to providing eye care [20]. Another study illustrated that many participants had weak knowledge about patient eye care and regular eye visits and paid more attention to treatment than prevention [21].
Little is still known about nurses' eye care knowledge, attitude, and practice. Lack of eye care studies in critically ill patients is a common issue globally, especially in Iran. This study aimed to evaluate ICU nurses' clinical competence (Knowledge, Attitude, and Practice) in eye care.
Instrument & Methods
This secondary analysis study (of psychometric study) was conducted in 2015. The study setting was ten teaching hospitals located in Tehran, Shiraz, Qom, and Kerman cities located in Iran. Ten hospitals were selected by cluster sampling of 4 cities in Iran, 432 intensive care nurses were recruited by convenience sampling. The sample size was determined based on the standard criteria identifying a minimum sample size for factor analysis, which was 5-10 times more than the number of items calculated in the primary study for scale development. The inclusion criteria were having at least one year of work experience in ICU and holding a university degree in nursing.
Data collection was a two-part questionnaire including demographic characteristics (gender, age, university degree, passed specialized intensive care courses, having eye care guidelines in the ward etc.) and previously validated Eye Care Competence Inventory. Study data were collected by using a previously validated Eye Care Competence Inventory [22]. Eye Care Competence Inventory (ECCI) consists of 35 items in three domains: knowledge, attitude, and practice. The knowledge domain comprises 18 multiple-choice questions on nurses' knowledge of eye disorders, risk factors for eye disorders, and eye care. Right and wrong answers are scored 0 and 1, respectively. The attitude and practice domains consist of 7 and 10 items respectively on nurses' eye care attitude and practice scored on a 5point Likert scale (from 1 to 5). The possible total scores of these two domains are 7-35 and 8-40. For better judgment and understanding, the ECCI domains in our study ranged from 0 to 100. Accordingly, higher scores equated to greater knowledge and better attitude and practice (less: lower than 33.3, moderate: between 33.3-66.6, good: further than 66.7). The Kuder-Richardson coefficient of the knowledge domain and the Cronbach's alphas of the attitude and practice domains and the whole inventory was 0.76, 0.85, and 0.83. The Kuder-Richardson coefficient was used for evaluating the internal consistency of the knowledge domain because the items of this domain were scored dichotomously. On the other hand, the stability of the questionnaire was assessed by using the test-retest method. Accordingly, a sub-sample of 18 nurses invited to complete the questionnaire twice with a 15-day interval and calculated the Interclass Correlation Coefficient. The test-retest interclass correlation coefficient was good (ICC=0.69) [21].
The approval code was from Baqiyatallah University of Medical Science. Study participants were informed of the study aim. Participation in the study was completely voluntary. The researchers ensured the confidentiality of the study participants provided data. Before the questionnaire was distributed to the nurses in each ICU, a researcher associated with each ICU explained the purpose of the study and received verbal informed consent from nurses. Nurse participants completed the questionnaire in the ICU of their respective hospital between September 2015 and June 2015. The researchers distributed and collected the questionnaire.
Study data were analyzed by using the Statistical Package for Social Sciences (SPSS v. 18.0). Nurses' eye care knowledge, attitude, and practice scores were presented using descriptive measures such as mean and standard deviation. Primarily, the normality of the study variables was assessed by performing the Kolmogorov-Smirnov test. Consequently, the independent-samples t-test was used for between-group comparisons of knowledge, attitude, and practice scores regarding variables such as gender, presence of eye care guidelines in the ward, intensive care license, and passing the infection control course. Moreover, the Pearson product-moment correlation test was employed for examining the correlation between nurses' eye care competence, age, and work experience.
Findings
Only 432 intensive care nurses had filled out the questionnaires completely (Response Rate 93%). The mean±SD of nurses' age was 32.6±5.6 years participated in the study. Most of the study participants were female (71.3%) and held bachelor's degrees in nursing (94.2%). The study participants’ characteristics showed in Table 1.
Table 1) Selected participant demographic characteristics (n=432)
The mean±SD scores for eye care knowledge, attitude, and practice showed in Table 2. The independent-samples t-test revealed that female nurses had a better eye care practice than male nurses (p<0.05). However, male and female nurses did not differ significantly concerning eye care knowledge and attitude.
Table 2) The mean±SD of nurses' clinical competence scores (Range of Score 0 – 100 and N=432)
The nurses who had such guidelines in their ward acquired significantly higher eye care knowledge, attitude, and practice scores than those who did not have guidelines (p<0.05; Table 3).
Table 3) The mean±SD difference between domains of the ECCI and Socio-demographic characteristics
Nurses' work experience positively correlated with their eye care knowledge and attitude. There also was a significant positive correlation between nurses' age and their eye care attitude. Finally, knowledge had significant positive correlations with attitude and practice (p<0.001; Table 4).
Table 4) Correlation between of three domains of the ECCI and Socio-demographic characteristics
Discussion
We conducted this study to evaluate ICU nurses' clinical competence in eye care. Accordingly, we assessed ICU nurses' eye care knowledge, attitude, and practice. Our findings revealed that the study participants had limited eye care knowledge. Some of the studies were reported the same finding [12, 23, 24]. This can be attributed to ICU nurses' greater involvement with managing life-threatening conditions and maintaining the functions of vital organs and their subsequent little attention to eye care [4]. Despite these results, Fulbrook et al., [18], and Jansson et al. [25] illustrated that the nurses in their studies had good knowledge. This contradiction is probably because we were mainly concerned with evaluating ICU nurses' knowledge of intensive care in general and ventilator-associated pneumonia, respectively.
An interesting finding of the study was that our participating nurses had a positive attitude towards providing eye care despite having limited eye care knowledge. None of the previous studies dealt with nurses' eye care attitude to the best of our knowledge.
Another finding of the study was that while our participants had limited eye care knowledge, they followed a good eye care practice. This finding poses this challenging question: how can nurses, who have limited knowledge, follow a sound practice? To respond to this question probably, our nurses provided eye care more based on their clinical experiences and established routines than their professional knowledge. Therefore, eye care must be incorporated into critical care training programs for ICU nurses to support the delivery of quality patient care. Another reason behind this finding is that we used a self-report questionnaire that subjectively evaluated nurses' eye care practice.
This finding conflicts with the findings of Vyas, who reported that ICU nurses had poor eye care performance. This conflict between the two studies' findings is probably because we used a self-report questionnaire while Vyas evaluated nurses' practice by using an observational performance checklist [24]. Further studies must evaluate nurses' eye care practice by using both self-report questionnaires and observational performance checklists.
We also found that compared with male nurses, female nurses obtained significantly higher eye care practice scores. However, there was no statistically significant difference between male and female nurses' eye care knowledge and attitude. These findings conflict with Yousefi et al., which can be attributed to the difference in the studies' measurement tools and unequal gender distribution [25]. Study findings also revealed a significant positive correlation between nurses' work experience and their eye care knowledge and attitude. Other studies also reported the same finding [12, 18, 26]. However, this finding contradicts some of the research findings that no relationship between work experience and KAP eye care [24, 26, 27].
We also found that nurses' age did not significantly correlate with their eye care knowledge and practice. This finding is in line with the findings of the previous studies [26]. However, there was a significant positive correlation between nurses' age and their eye care attitude. This can be due to more clinical experience in older nurses, which leads to a positive attitude towards eye care in ICU patients. On the other hand, the younger nurses should be given appropriate training in eye care.
The study showed that nurses' eye care knowledge significantly correlated with their eye care attitude and practice. Other studies also reported the same finding [27, 28]. Moreover, nurses who had access to eye care guidelines in their ward acquired significantly higher eye care knowledge, attitude, and practice scores than their counterparts who did not have such guidelines. This finding is consistent with the findings of the previous studies [29, 30]. ICU nurses' greater involvement with managing life-threatening situations can be an obstacle for attending to less important aspects of care such as eye care. However, clear guidelines can remind nurses of the importance and the necessity of providing eye care.
We also found no significant differences between the eye care knowledge, attitude, and practice scores of nurses who had passed specialized intensive care courses and the nurses who had not passed such courses. Celik et al. [31] also reported the same finding. These courses probably mainly focus more on the assessment and management of life-threatening conditions than the other aspects of care such as eye care. Therefore, Eyecare education necessary for ICU nurses, especially inexperienced nurses in intensive care unit nursing, and provide continuing education on the latest eye care methods and information to experienced nurses. Accordingly, this study shows absent or insufficient eye care education for critically ill patients in ICU nursing training programs in Iran. So that, eye care should be incorporated into critical care education programs for ICU nurses to deliver quality patient care.
Finally, nurses who had passed control infection management courses obtained significantly higher eye care knowledge, attitude, and practice scores than those who had not taken such courses. Yousefi et al. also reported the same finding. This finding can be attributed to the stronger awareness and greater sensitivity of nurses who take these courses regarding the importance of infection management [26].
A self-report questionnaire was used for evaluating nurses' eye care practice. Self-report questionnaires provide a subjective assessment of practice. Accordingly, verifying the accuracy of self-report questionnaires by using observational checklists as well as employing observational checklists for eye care practice evaluation are recommended. Given its Likert-type scale, ECCI can develop observational checklists to evaluate nurses' eye care practice objectively.
Conclusion
The result showed that nurses' knowledge in eye care of ICU patients was moderate and attitude and practice, intensive care nurses' eye care were good. Given the direct correlation between nurses' eye care knowledge and their eye care attitude and practice, enhancing their knowledge would also positively influence their attitude and practice.
Acknowledgments: The authors grateful to the Faculty of Nursing and trauma research center, Baqiyatallah University of Medical Sciences and the authorities of hospitals and all the nurses working in these hospitals who kindly cooperated in conducting this research.
Ethical Permissions: IRB approval number: IR.BMSU.RECH.1392.26
Conflicts of Interests: We declare that we have no conflicts of interest.
Authors’ Contribution: Ebadi A. (First Author), Methodologist/Statistical Analyst (25%); Moayed M.S. (Second Author), Introduction Writer, Discussion Writer (25%); Mirsadeghi A. (Third Author), Introduction Writer (25%); Saeid Y. (Forth Author) Assistant Researcher (25%).
Funding/Support: No funding.
Article Type: Descriptive & Survey |
Subject:
Health Education and Health Behavior
Received: 2021/01/21 | Accepted: 2021/05/23 | Published: 2021/07/7
Received: 2021/01/21 | Accepted: 2021/05/23 | Published: 2021/07/7
References
1. Hearne BJ, Hearne EG, Montgomery H, Lightman SL. Eye care in the intensive care unit. J Intensive Care Soc. 2018;19(4):345-50. [Link] [DOI:10.1177/1751143718764529] [PMID] [PMCID]
2. Oliveira R, De Lima Fernandes APN, Botarelli FR, De Medeiros Araujo JN, Barreto VP, Vitor AF. Risk factors for injury in the cornea in critical patients in intensive care: An integrative review. J Res Fundam Care Online. 2016;8(2):4423-34. [Link] [DOI:10.9789/2175-5361.2016.v8i2.4423-4434]
3. Dawson D. Development of a new eye care guideline for critically ill patients. Intensive Crit Care Nurs. 2005;21(2):119-22. [Link] [DOI:10.1016/j.iccn.2005.01.004] [PMID]
4. Grixti A, Sadri M, Edgar J, Datta AV. Common ocular surface disorders in patients in intensive care units. Ocul Surf. 2012;10(1):26-42. [Link] [DOI:10.1016/j.jtos.2011.10.001] [PMID]
5. Mela EK, Drimtzias EG, Christofidou MK, Filos KS, Anastassiou ED, Gartaganis SP. Ocular surface bacterial colonisation in sedated intensive care unit patients. Anaesth Intensive Care. 2010;38(1):190-3. [Link] [DOI:10.1177/0310057X1003800129] [PMID]
6. Oncul H, Yektas A. Eye problems, eye care and ocular awareness in a level 3 intensive care unit. Turk J Intensive Care. 2019;18(2):13471. [Link] [DOI:10.4274/tybd.galenos.2019.13471]
7. Valizade Hasanloei MA, Motarjemizadeh G, Pakzad S, Asghari M. Exposure keratitis in mechanical ventilatory patients admitted to intensive care unit. J Med Sci Stud. 2018;29(6):421-7. [Persian] [Link]
8. Grixti A, Sadri M, Watts MT. Corneal protection during general anesthesia for nonocular surgery. Ocul Surf. 2013;11(2):109-18. [Link] [DOI:10.1016/j.jtos.2012.10.003] [PMID]
9. Weril-Alvarenga A, Eecole FF, Botoni FA, Mourao Oliveira JADM, Chianca TCM. Corneal injuries: Incidence and risk factors in the intensive care unit. Rev Lat Am Enfermaqem. 2011;19(5):1088-95. [Link] [DOI:10.1590/S0104-11692011000500005] [PMID]
10. Saritas TB, Bozkurt B, Simsek B, Cakmak Z, Ozdemir M, Yosunkaya A. Ocular surface disorders in intensive care unit patients. Sci World J. 2013;2013:182038. [Link] [DOI:10.1155/2013/182038] [PMID] [PMCID]
11. Narmawala W, Jani HC. Exposure keratopathy: Prophylaxis and impact of eye care education programme in ICU patients. J Clin Diagn Res. 2017;11(10):6-9. [Link] [DOI:10.7860/JCDR/2017/25906.10717]
12. Guler EK, Eser I, Fashafsheh IHD. Intensive care nurses' views and practices for eye care: An international comparison. Clin Nurs Res. 2017;26(4):504-24. [Link] [DOI:10.1177/1054773816631471] [PMID]
13. Liem LH. Assess knowledge and practice eye care for patients of intensive care unit nursing staff [dissertation]. Greeley: University of Northern Colorado; 2019. [Link]
14. So HM, Lee CCH, Leung AKH, Lim JMJA, Chan CSC, Yan WW. Comparing the effectiveness of polyethylene covers (Gladwrap) with lanolin (Duratears) eye ointment to prevent corneal abrasions in critically ill patients: A randomized controlled study. Int J Nurs Stud. 2008;45(11):1565-71. [Link] [DOI:10.1016/j.ijnurstu.2008.02.005] [PMID]
15. Babamohamadi H, Nobahar M, Razi J, Ghorbani R. Comparing vitamin A and moist chamber in preventing ocular surface disorders. Clin Nurs Res. 2018;27(6):714-29. [Link] [DOI:10.1177/1054773817695618] [PMID]
16. Wong J, Lan W, Ong LM, Tong L. Non-hormonal systemic medications and dry eye. Ocul Surf. 2011;9(4):212-26. [Link] [DOI:10.1016/S1542-0124(11)70034-9]
17. Marshall AP, Elliott R, Rolls K, Schacht S, Boyle M. Eye care in the critically ill: Clinical practice guideline. Aust Crit Care. 2008;21(2):97-109. [Link] [DOI:10.1016/j.aucc.2007.10.002] [PMID]
18. Fulbrook P, Albarran JW, Baktoft B, Sidebottom B. A survey of European intensive care nurses' knowledge levels. Int J Nurs Stud. 2012;49(2):191-200. [Link] [DOI:10.1016/j.ijnurstu.2011.06.001] [PMID]
19. Masoudi Alavi N, Sharifitabar Z, Shaeri M, Adib Hajbaghery M. An audit of eye dryness and corneal abrasion in ICU patients in Iran. Nurs Crit Care. 2014;19(2):73-7. [Link] [DOI:10.1111/nicc.12052] [PMID]
20. Momeni Mehrjardi Z, Mirzaei S, Gohari M, Hafezieh A, Nasiriani K. Effect of training eye care clinical guideline for ICU patients on clinical competence of eye care in nurses. Crit Care Res Pract. 2021;2021:6669538. [Link] [DOI:10.1155/2021/6669538] [PMID] [PMCID]
21. Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: Applications to assessment of adaptive behavior. Am J Ment Defic. 1981;86(2):127-37. [Link]
22. Ebadi A, Saeid Y, Ashrafi S, Taheri‐Kharameh Z. Development and psychometric evaluation of a questionnaire on nurses' clinical competence eye care in intensive care unit patients. Ners Crit Care. 2017;22(3):169-75. [Link] [DOI:10.1111/nicc.12113] [PMID]
23. Alghamdi MA, Ghaleb MA, Abdel Aal SE. Assessment of intensive care nurse knowledge and perception of eye care practice for unconscious and mechanically ventilated patients in intensive care units in Saudi Arabia. Res Rev J Nurs Health Sci. 2018;4(1):15-23. [Link]
24. Vyas S, Mahobia A, Bawankure S. Knowledge and practice patterns of Intensive Care Unit nurses towards eye care in Chhattisgarh state. Indian J Ophthalmol. 2018;66(9):1251-5. [Link] [DOI:10.4103/ijo.IJO_115_18] [PMID] [PMCID]
25. Yousefi H, Nahidian M, Sabouhi F. Reviewing the effects of an educational program about sepsis care on knowledge, attitude, and practice of nurses in intensive care units. Iran J Nurs Midwifery Res. 2012;17(2 Suppl1):91-5. [Link]
26. Jansson M, Ala-Kokko T, Ylipalosaari P, Syrjala H, Kyngas H. Critical care nurses' knowledge of, adherence to and barriers towards evidence-based guidelines for the prevention of ventilator-associated pneumonia-a survey study. Intensive Crit Care Nurs. 2013;29(4):216-27. [Link] [DOI:10.1016/j.iccn.2013.02.006] [PMID]
27. Eskander HG, Morsy WYM, Elfeky HAA. Intensive care nurses' knowledge & practices regarding Infection control standard precautions at a selected Egyptian cancer hospital. J Educ Pract. 2013;4(19):160-74. [Link]
28. Soh KL, Davidson PM, Leslie G, DiGiacomo M, Soh KG. Nurses' perceptions of standardised assessment and prevention of complications in an ICU. J Clin Nurs. 2013;22(5-6):856-65. [Link] [DOI:10.1111/jocn.12017] [PMID]
29. Azfar MF, Khan MF, Alzeer AH. Protocolized eye care prevents corneal complications in ventilated patients in a medical intensive care unit. Saudi J Anaesth. 2013;7(1):33-6. [Link] [DOI:10.4103/1658-354X.109805] [PMID] [PMCID]
30. Kam KYR, Haldar S, Papamichael E, Pearce KCS, Hayes M, Joshi N. Eye care in the critically ill: A national survey and protocol. J Intensive Care Soc. 2013;14(2):150-4. [Link] [DOI:10.1177/175114371301400213]
31. Celik S, Ugras GA, Durdu S, Kubas M, Aksoy G. Critical care nurses' knowledge about the care of deceased adult patients in an intensive care unit. Aust J Adv Nurs. 2008;26(1):53-8. [Link]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |