Volume 9, Issue 1 (2021)
Health Educ Health Promot 2021, 9(1): 49-54 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rabiei N, Gholami Fesharaki M, Rowzati M. Antihypertensive Medications in Hypertension Control in Male Industrial Employees: a Retrospective Cohort Study. Health Educ Health Promot 2021; 9 (1) :49-54
URL: http://hehp.modares.ac.ir/article-5-48809-en.html
URL: http://hehp.modares.ac.ir/article-5-48809-en.html
1- Biostatistics Department, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Islamic Republic of Iran
2- Biostatistics Department, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Islamic Republic of Iran , mohammad.gholami@modares.ac.ir
3- Occupational Health Center, Mobarakeh Steel Company, Isfahan, Iran
2- Biostatistics Department, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Islamic Republic of Iran , mohammad.gholami@modares.ac.ir
3- Occupational Health Center, Mobarakeh Steel Company, Isfahan, Iran
Full-Text [PDF 471 kb]
(890 Downloads)
| Abstract (HTML) (1570 Views)
Full-Text: (293 Views)
Introduction
Hypertension is one of the most important public issues and treatable risk factors for cardiovascular disease (CVD) [1]. Hypertension is the leading cause of cardiovascular disease and premature death worldwide [2]. According to the world health organization report, hypertension (13%), tobacco consumption (9%), high blood glucose (6%), physical inactivity (6%), and overweight and obesity (5%) are responsible for mortality throughout the world [3]. Hypertension prevalence is 52.0% and 44.3% in Iranian men and women, respectively [4]. Over the last few decades, hypertension treatment has improved, and the incidence of mortality due to stroke and coronary heart disease (CHD) decreased but remains uncontrolled in all societies [5, 6]. Monotherapy or some combinations of diuretics, angiotensin-converting enzyme inhibitors, calcium antagonists, beta-blockers, and angiotensin receptor blockers are satisfactory for starting and preserving anti-hypertensive treatment [7].
Hypertension is one of the most important challenges to human health in both developed and developing countries. Hypertension is common, but it can be detected and treated [8]. The high prevalence of hypertension and the serious effects on the body's organs have made it a major health challenge in all communities, and control of that became so important for minimizing the outcomes of this illness [9]. Even though preventing and treating of this illness is attention and offered some detected approaches for treating of that [10], (such as availability more than 100 types of different medicines of hypertension that efficiency of all of them are proved) but the reported statistics in this field is frustrating [11]. The success rate for control of hypertension in the USA is reported only 27%, and in England, France and Germany is less than 27% [12]. Also, analyzing of clinical characteristics of patients by COVID-19 proved that 20-30% of all of these patients and 58.3% of patients in the intensive care unit (ICU) are patients with hypertension and the reason of 60.9% of mortality of COVID-19 patients is hypertension [13].
Approaches about selecting medicine and choosing the best decisions for different subgroups are changed over time, and it is variable in different countries, and experts cannot choose the best medicine [14]. Some primary medicine for control hypertension is Thiazide-diuretics, Calcium channel blockers (CCB), Angiotensin-Converting Enzyme Inhibitors (ACE), angiotensin receptor blockers (ARB) [15]. In addition to the direct effect of medicine in reducing hypertension, some other factors are effective on hypertension; Such as BMI increasing [16, 17], age increasing [17], shift work [18], and facing high noises in the workplace [19].
Due to the incapability of physicians to control hypertension in patient populations in their clinics (less than 30%), alternative medical care such as workplace interventions has been suggested [1]. Some intervention programs like "Stop Hypertension in Mobarakeh Steel Company" (SHIMSCO) study [2] reported hypertension reduction after the intervention.
Given the importance of controlling hypertension, this research was done to study the effect of anti-hypertensive drugs on changing blood pressure, Body Mass Index (BMI), and Framingham Risk Score (FRS).
Instrument and Methods
This retrospective cohort study (from January 2014 to January 2018) was done on workers who work in MSCO. They were chosen using the census method by referring to their medical records, initially, by referring to 7892 medical records registered in the occupational health center of MSCO, all those who were diagnosed with hypertension in 2014 and were taking medication to control their BP at the beginning of the study considered as a case group and the others person who were health during study period considered as a control group. The inclusion criteria were as follows (i) being male, (ii) being official or contract employment, (iii) at least two years of services, (iv) age between 20 and 60. Workers unwilling to participate in the study or high missing information in medical records were excluded. The full details of sample selection were presented in Diagram 1.
The FRS is a gender-specific algorithm used to estimate the 10-year risk of cardiovascular in individuals. This Score estimates the probability that a person will develop cardiovascular disease within a specified amount of time, usually 10 to 30 years. They also indicate who is the most likely to benefit from prevention [22]. The formulation of this index is presented in Bazyar et al.'s study [20].
This research was approved by the Medical Ethics Committee of Tarbiat Modares University. Demographic data, including age, work experience, educational level, besides variables such as SBP, DPB, BMI, and FRS, were measured in each participant. The blood pressure of both arms was measured by three general practitioners using a calibrated portable or wall-mounted Baumometer sphygmomanometer Kompak Model-260 mm Hg (WA Baum, Copiague, NY).
Continuous variables are described with mean±SE, and discrete variables are presented with numbers and percentages. An independent t-test was used to compare SBP, DBP, BMI, FRS between two groups in 2014. For evaluating the effect of time on changing SBP, DBP, BMI, FRS within and between two groups the multilevel modeling [23] was used. Data were analyzed by R 3.2.1 software and package "NLME". p-values less than 0.05 were considered significant.
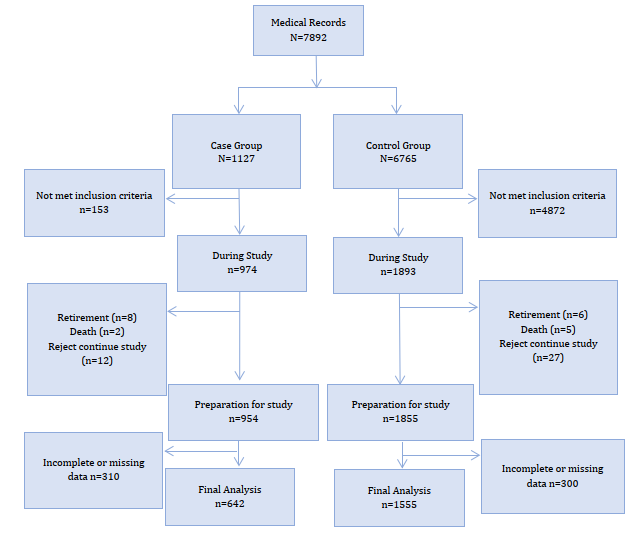
Diagram 1) Follow up study
Findings
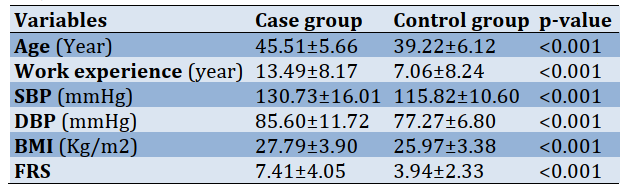
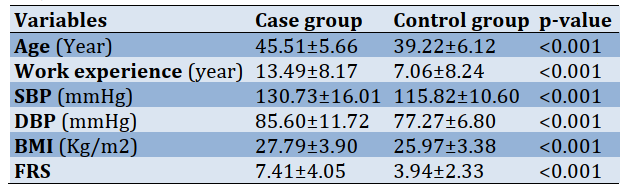
The demographic data showed in table 1.
Table 1) The mean±SE variables in two group in 2014 (n= 2197)
For evaluating the effect of time on changing SBP, DBP, BMI, FRS within and between two groups, variables like age, work experience, besides baseline variables like SBP, DBP, BMI, and FRS, were controlled using multilevel modeling.
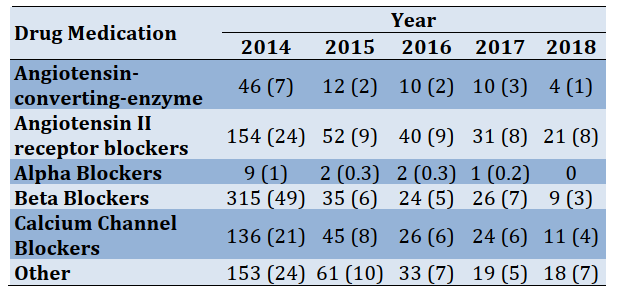
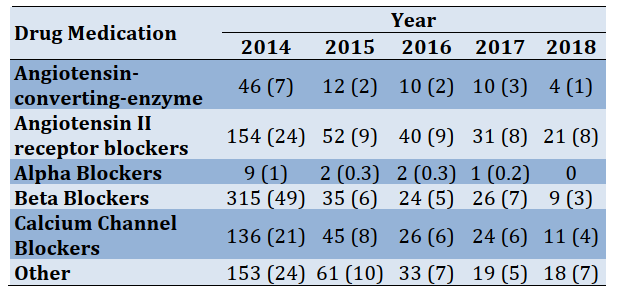
In Table 2, the frequency of anti-hypertensive medication during five years study was presented. The adherence to the use of anti-hypertensive drugs in the first year of study was a maximum of 49%, but this rate decreased to less than 10% in the second to fifth years of study.
Table 2) Frequency of anti-hypertensive medication during the study (the numbers in parentheses are in percent)
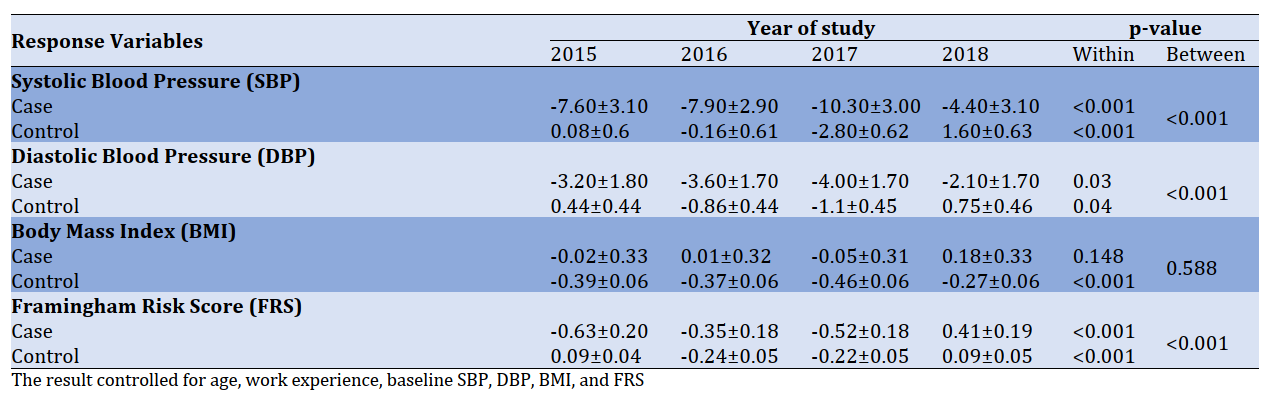
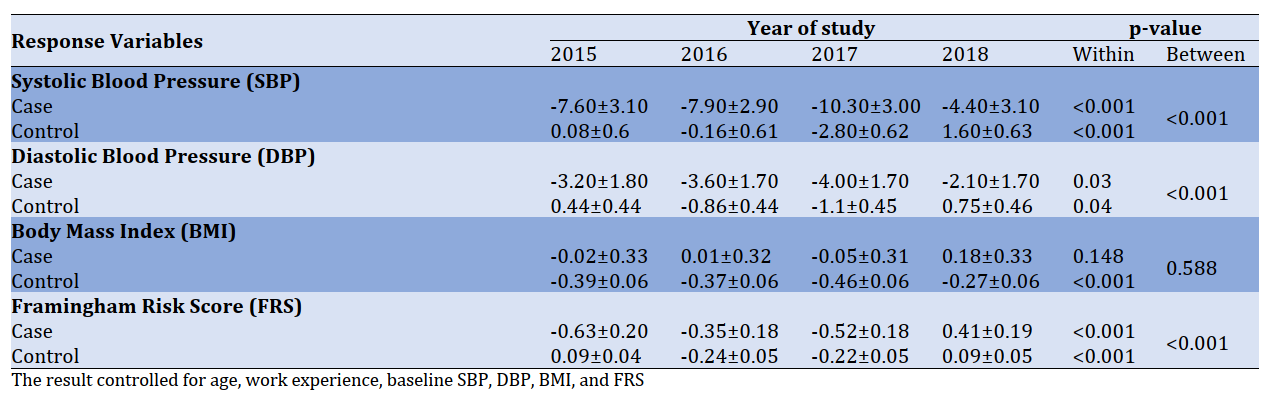
The trend of change of variable during 5 years follows up compared with anti-hypertension drug presented in Diagram 2 besides the change of SBP, DBP, BMI, and FRS during time and comparison between two groups with controlling unequal baseline variables using multilevel analysis presented in Table 3.
The results of this study showed that changes in SBP, DBP, and FRS during 2014 to 2018 in the case group compared to the control group had a significant decrease (p<0.001), but this decrease was not significant for the BMI (p=0.588).
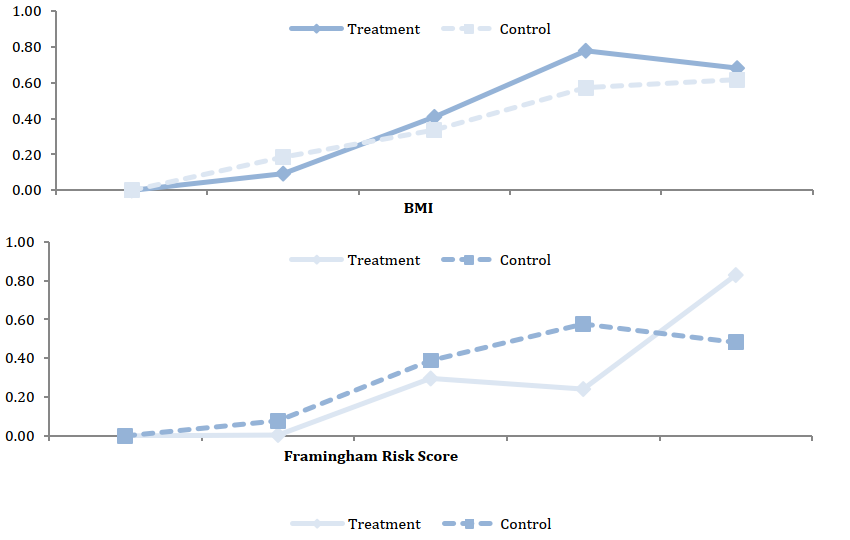
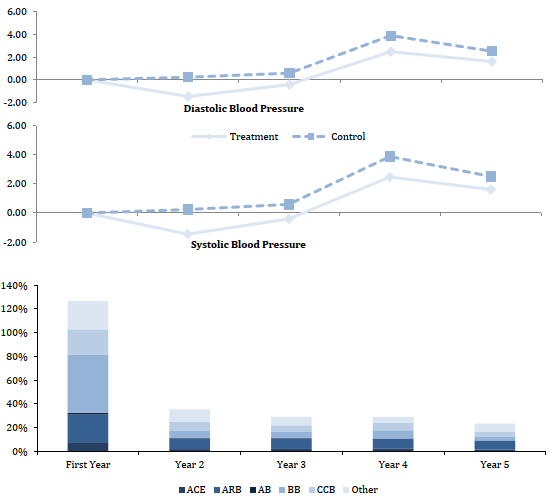
Diagram 2) The trend of DP, SBP, DBP, FRS, and BMI during 5 years (2014-2018) follow up. DP: Drug Prevalence, SBP: Systolic Blood Pressure, DBP: Diastolic Blood Pressure, FRS: Framingham Risk Score, BMI: Body Mass Index, ACE: Angiotensin-converting-enzyme, ARB: Angiotensin II receptor
Table 3) βchange±SE of SBP, DBP, BMI, and FRS during time and comparison between two groups with controlling unequal baseline variables using multilevel analysis
Hypertension is one of the most important public issues and treatable risk factors for cardiovascular disease (CVD) [1]. Hypertension is the leading cause of cardiovascular disease and premature death worldwide [2]. According to the world health organization report, hypertension (13%), tobacco consumption (9%), high blood glucose (6%), physical inactivity (6%), and overweight and obesity (5%) are responsible for mortality throughout the world [3]. Hypertension prevalence is 52.0% and 44.3% in Iranian men and women, respectively [4]. Over the last few decades, hypertension treatment has improved, and the incidence of mortality due to stroke and coronary heart disease (CHD) decreased but remains uncontrolled in all societies [5, 6]. Monotherapy or some combinations of diuretics, angiotensin-converting enzyme inhibitors, calcium antagonists, beta-blockers, and angiotensin receptor blockers are satisfactory for starting and preserving anti-hypertensive treatment [7].
Hypertension is one of the most important challenges to human health in both developed and developing countries. Hypertension is common, but it can be detected and treated [8]. The high prevalence of hypertension and the serious effects on the body's organs have made it a major health challenge in all communities, and control of that became so important for minimizing the outcomes of this illness [9]. Even though preventing and treating of this illness is attention and offered some detected approaches for treating of that [10], (such as availability more than 100 types of different medicines of hypertension that efficiency of all of them are proved) but the reported statistics in this field is frustrating [11]. The success rate for control of hypertension in the USA is reported only 27%, and in England, France and Germany is less than 27% [12]. Also, analyzing of clinical characteristics of patients by COVID-19 proved that 20-30% of all of these patients and 58.3% of patients in the intensive care unit (ICU) are patients with hypertension and the reason of 60.9% of mortality of COVID-19 patients is hypertension [13].
Approaches about selecting medicine and choosing the best decisions for different subgroups are changed over time, and it is variable in different countries, and experts cannot choose the best medicine [14]. Some primary medicine for control hypertension is Thiazide-diuretics, Calcium channel blockers (CCB), Angiotensin-Converting Enzyme Inhibitors (ACE), angiotensin receptor blockers (ARB) [15]. In addition to the direct effect of medicine in reducing hypertension, some other factors are effective on hypertension; Such as BMI increasing [16, 17], age increasing [17], shift work [18], and facing high noises in the workplace [19].
Due to the incapability of physicians to control hypertension in patient populations in their clinics (less than 30%), alternative medical care such as workplace interventions has been suggested [1]. Some intervention programs like "Stop Hypertension in Mobarakeh Steel Company" (SHIMSCO) study [2] reported hypertension reduction after the intervention.
Given the importance of controlling hypertension, this research was done to study the effect of anti-hypertensive drugs on changing blood pressure, Body Mass Index (BMI), and Framingham Risk Score (FRS).
Instrument and Methods
This retrospective cohort study (from January 2014 to January 2018) was done on workers who work in MSCO. They were chosen using the census method by referring to their medical records, initially, by referring to 7892 medical records registered in the occupational health center of MSCO, all those who were diagnosed with hypertension in 2014 and were taking medication to control their BP at the beginning of the study considered as a case group and the others person who were health during study period considered as a control group. The inclusion criteria were as follows (i) being male, (ii) being official or contract employment, (iii) at least two years of services, (iv) age between 20 and 60. Workers unwilling to participate in the study or high missing information in medical records were excluded. The full details of sample selection were presented in Diagram 1.
The FRS is a gender-specific algorithm used to estimate the 10-year risk of cardiovascular in individuals. This Score estimates the probability that a person will develop cardiovascular disease within a specified amount of time, usually 10 to 30 years. They also indicate who is the most likely to benefit from prevention [22]. The formulation of this index is presented in Bazyar et al.'s study [20].
This research was approved by the Medical Ethics Committee of Tarbiat Modares University. Demographic data, including age, work experience, educational level, besides variables such as SBP, DPB, BMI, and FRS, were measured in each participant. The blood pressure of both arms was measured by three general practitioners using a calibrated portable or wall-mounted Baumometer sphygmomanometer Kompak Model-260 mm Hg (WA Baum, Copiague, NY).
Continuous variables are described with mean±SE, and discrete variables are presented with numbers and percentages. An independent t-test was used to compare SBP, DBP, BMI, FRS between two groups in 2014. For evaluating the effect of time on changing SBP, DBP, BMI, FRS within and between two groups the multilevel modeling [23] was used. Data were analyzed by R 3.2.1 software and package "NLME". p-values less than 0.05 were considered significant.
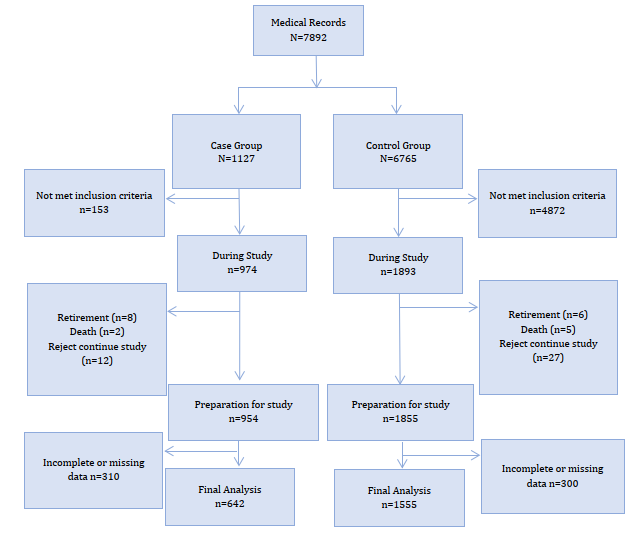
Diagram 1) Follow up study
Findings
The demographic data showed in table 1.
Table 1) The mean±SE variables in two group in 2014 (n= 2197)
For evaluating the effect of time on changing SBP, DBP, BMI, FRS within and between two groups, variables like age, work experience, besides baseline variables like SBP, DBP, BMI, and FRS, were controlled using multilevel modeling.
In Table 2, the frequency of anti-hypertensive medication during five years study was presented. The adherence to the use of anti-hypertensive drugs in the first year of study was a maximum of 49%, but this rate decreased to less than 10% in the second to fifth years of study.
Table 2) Frequency of anti-hypertensive medication during the study (the numbers in parentheses are in percent)
The trend of change of variable during 5 years follows up compared with anti-hypertension drug presented in Diagram 2 besides the change of SBP, DBP, BMI, and FRS during time and comparison between two groups with controlling unequal baseline variables using multilevel analysis presented in Table 3.
The results of this study showed that changes in SBP, DBP, and FRS during 2014 to 2018 in the case group compared to the control group had a significant decrease (p<0.001), but this decrease was not significant for the BMI (p=0.588).
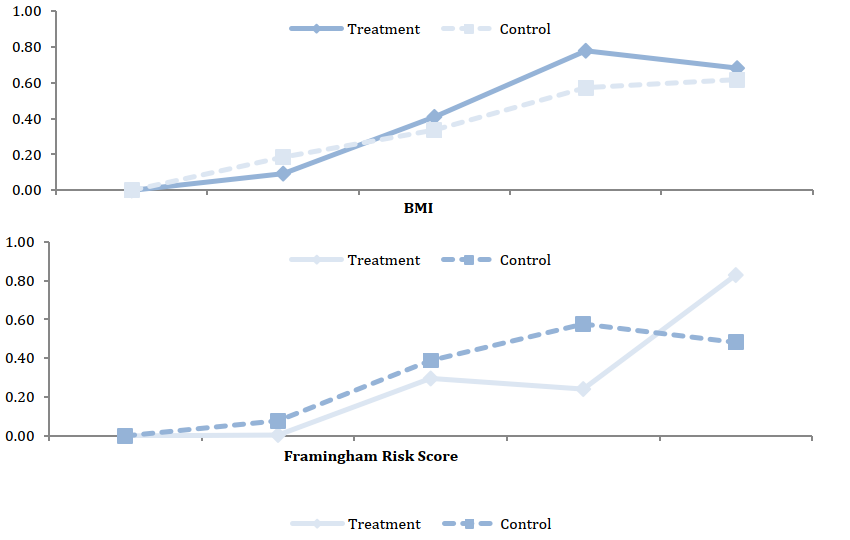
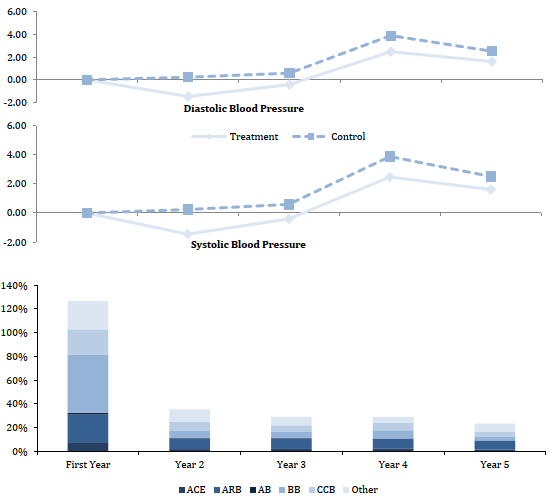
Diagram 2) The trend of DP, SBP, DBP, FRS, and BMI during 5 years (2014-2018) follow up. DP: Drug Prevalence, SBP: Systolic Blood Pressure, DBP: Diastolic Blood Pressure, FRS: Framingham Risk Score, BMI: Body Mass Index, ACE: Angiotensin-converting-enzyme, ARB: Angiotensin II receptor
Table 3) βchange±SE of SBP, DBP, BMI, and FRS during time and comparison between two groups with controlling unequal baseline variables using multilevel analysis
Discussion
Hypertension is one of the most important challenges to human health in both developed and developing countries. Hypertension is common, but it can be detected and treated [12]. The high prevalence of hypertension and the serious effects on the body's organs has made it a major health challenge in all communities, and control of that became so important for minimizing the outcomes of this illness [13]. Even though preventing and treating of this illness is attention and offered some detected approaches for treating of that [14], (such as availability more than 100 types of different medicines of hypertension that efficiency of all of them are proved) but the reported statistics in this field is frustrating [15]. The success rate for control of hypertension in the USA is reported only 27%, and in England, France and Germany is less than 27% [16]. Also, analyzing of clinical characteristics of patients by COVID-19 proved that 20-30 % of all of these patients and 58.3 % of patients in the intensive care unit (ICU) are patients with hypertension, and 60.9 % of mortality of COVID-19 patients is hypertension [17].
Approaches about selecting medicine and choosing the best decision for different subgroups are changed over time, and it is variable in different countries, and experts cannot choose the best medicine [18]. Some primary medicine for control hypertension is Thiazide-diuretics, Calcium channel blockers (CCB), Angiotensin-Converting Enzyme Inhibitors (ACE), angiotensin receptor blockers (ARB) [19]. In addition to the direct effect of medicine in reducing hypertension, some other factors are effective on hypertension; Such as BMI increasing [20, 21], age increasing [21], shift work [22], and facing high noises in the workplace [23].
This study showed that consumption of anti-hypertensive drugs and the execution of self-care programs lead to control hypertension. In this situation, after reducing monitoring authorities on this project, reducing self-care leads to increasing hypertension. It has a similar trend to the control group. It should be notice that the effect of reducing self-care in the graph of BMI is shown clearly. More results have shown that consumption of medicine to control hypertension is reduced in second to fifth years. It should be noticed that insufficient self-care is an important challenge for the patient with chronic illnesses especially patients with hypertension and by not obeying these treating programs, these patients will have serious outcomes such as extending these illnesses and need to immediate cares and hospitalize. Some outcomes such as brain stroke, Atherosclerosis, a heart attack will threaten them. Medical reports show that failure in hypertension control is not obeying the treatment team's comments [24]. In many surveys, consumption of medicines is so important and results showed that self-care in hypertension by the patient is inappreciable [16, 25-28]. So the execution of self-care programs and persistence in consumption of hypertension medicine are two of the most important basic cases of control hypertension that patients should notice.
One of the most important strengths of this is the high volume of the studied society which led to better matching of the control and case groups—strengths of this study that it was longitudinal. Participants were under long-term care, and during the follow-up period, the individuals having hypertension were identified, and medication interventions were made, which assist the physician in finding the effective medication for the patient. According to the factors affecting hypertension, there are other confounding factors that we did not pay attention to or lack of information in the model. For example, the variables such as quality of life, family history of high blood pressure, history of illness except for hypertension like diabetes.
Conclusion
The workplace Intervention Project is effective in controlling hypertension, and there must be continuity in its implementation. Furthermore, amending lifestyle and diet are recommended along with consumption of anti-hypertensive medications.
Acknowledgments: We gratefully acknowledge the Tarbiat Modares University for Financial support, and the authors wish to thank all the personnel of Mobarakeh steel company for their cooperation throughout the study.
Ethical Permissions: This research was approved by the Medical Ethics Committee of Tarbiat Modares University (IR.TMU.REC.1396.589).
Conflicts of Interests: Authors have no conflict of interests.
Authors' Contribution: Rabiei N. (First author), Introduction author/Assistant researcher/Statistical analyst (40%); Gholami Fesharaki M. (Second author), Original researcher/Discussion author (40%); Rowzati M. (Third author), Methodologist/Discussion author (20%).
Funding/Sources: Tarbiat Modares University.
Hypertension is one of the most important challenges to human health in both developed and developing countries. Hypertension is common, but it can be detected and treated [12]. The high prevalence of hypertension and the serious effects on the body's organs has made it a major health challenge in all communities, and control of that became so important for minimizing the outcomes of this illness [13]. Even though preventing and treating of this illness is attention and offered some detected approaches for treating of that [14], (such as availability more than 100 types of different medicines of hypertension that efficiency of all of them are proved) but the reported statistics in this field is frustrating [15]. The success rate for control of hypertension in the USA is reported only 27%, and in England, France and Germany is less than 27% [16]. Also, analyzing of clinical characteristics of patients by COVID-19 proved that 20-30 % of all of these patients and 58.3 % of patients in the intensive care unit (ICU) are patients with hypertension, and 60.9 % of mortality of COVID-19 patients is hypertension [17].
Approaches about selecting medicine and choosing the best decision for different subgroups are changed over time, and it is variable in different countries, and experts cannot choose the best medicine [18]. Some primary medicine for control hypertension is Thiazide-diuretics, Calcium channel blockers (CCB), Angiotensin-Converting Enzyme Inhibitors (ACE), angiotensin receptor blockers (ARB) [19]. In addition to the direct effect of medicine in reducing hypertension, some other factors are effective on hypertension; Such as BMI increasing [20, 21], age increasing [21], shift work [22], and facing high noises in the workplace [23].
This study showed that consumption of anti-hypertensive drugs and the execution of self-care programs lead to control hypertension. In this situation, after reducing monitoring authorities on this project, reducing self-care leads to increasing hypertension. It has a similar trend to the control group. It should be notice that the effect of reducing self-care in the graph of BMI is shown clearly. More results have shown that consumption of medicine to control hypertension is reduced in second to fifth years. It should be noticed that insufficient self-care is an important challenge for the patient with chronic illnesses especially patients with hypertension and by not obeying these treating programs, these patients will have serious outcomes such as extending these illnesses and need to immediate cares and hospitalize. Some outcomes such as brain stroke, Atherosclerosis, a heart attack will threaten them. Medical reports show that failure in hypertension control is not obeying the treatment team's comments [24]. In many surveys, consumption of medicines is so important and results showed that self-care in hypertension by the patient is inappreciable [16, 25-28]. So the execution of self-care programs and persistence in consumption of hypertension medicine are two of the most important basic cases of control hypertension that patients should notice.
One of the most important strengths of this is the high volume of the studied society which led to better matching of the control and case groups—strengths of this study that it was longitudinal. Participants were under long-term care, and during the follow-up period, the individuals having hypertension were identified, and medication interventions were made, which assist the physician in finding the effective medication for the patient. According to the factors affecting hypertension, there are other confounding factors that we did not pay attention to or lack of information in the model. For example, the variables such as quality of life, family history of high blood pressure, history of illness except for hypertension like diabetes.
Conclusion
The workplace Intervention Project is effective in controlling hypertension, and there must be continuity in its implementation. Furthermore, amending lifestyle and diet are recommended along with consumption of anti-hypertensive medications.
Acknowledgments: We gratefully acknowledge the Tarbiat Modares University for Financial support, and the authors wish to thank all the personnel of Mobarakeh steel company for their cooperation throughout the study.
Ethical Permissions: This research was approved by the Medical Ethics Committee of Tarbiat Modares University (IR.TMU.REC.1396.589).
Conflicts of Interests: Authors have no conflict of interests.
Authors' Contribution: Rabiei N. (First author), Introduction author/Assistant researcher/Statistical analyst (40%); Gholami Fesharaki M. (Second author), Original researcher/Discussion author (40%); Rowzati M. (Third author), Methodologist/Discussion author (20%).
Funding/Sources: Tarbiat Modares University.
Article Type: Original Research |
Subject:
Healthy Life Style
Received: 2020/12/1 | Accepted: 2021/02/2 | Published: 2021/05/10
Received: 2020/12/1 | Accepted: 2021/02/2 | Published: 2021/05/10
References
1. Strain WD, Paldánius PM. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc Diabetol. 2018;17(1):57. [Link] [DOI:10.1186/s12933-018-0703-2] [PMID] [PMCID]
2. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223-37. [Link] [DOI:10.1038/s41581-019-0244-2] [PMID] [PMCID]
3. World Health Organization. Global health risks: Mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009 [Link]
4. Hosseini M, Yaseri M, Asady H, Musa AE, Koohpayehzadeh J, Rafei A, et al. Prevalence of high blood pressure in Iranian adults based on the 2017 ACC/AHA guideline. Med J Islam Repub Iran. 2019;33(1):151-7. [Link] [DOI:10.47176/mjiri.33.26]
5. Sarrafzadegan N, Mohammmadifard N. Cardiovascular disease in Iran in the last 40 years: Prevalence, mortality, morbidity, challenges and strategies for cardiovascular prevention. Arch Iran Med. 2019;22(4):204-10. [Link]
6. Katibeh M, Sanjari Moghaddam A, Yaseri M, Neupane D, Kallestrup P, Ahmadieh H. Hypertension and associated factors in the Islamic Republic of Iran: a population-based study. East Mediterr Health J. 2020;26(3):301-11. [Link] [DOI:10.26719/emhj.19.042] [PMID]
7. Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). 2013;31(7):1281-357. [Link] [DOI:10.1097/01.hjh.0000431740.32696.cc] [PMID]
8. Laar AK, Adler AJ, Kotoh AM, Legido-Quigley H, Lange IL, Perel P, et al. Health system challenges to hypertension and related non-communicable diseases prevention and treatment: Perspectives from Ghanaian stakeholders. BMC Health Serv Res. 2019;19:693. [Link] [DOI:10.1186/s12913-019-4571-6] [PMID] [PMCID]
9. Maftoon F, Farzadi F, Aeenparast A, Montazeri A, Mohammad K, Pileroudi S, et al. Evaluation of National Program on Prevention and Control of Hypertension: The Study Protocol. Adv Biores. 2016;7(3):15-20. [Link]
10. Lee HY, Shin J, Kim GH, Park S, Ihm SH, Kim HC, et al. 2018 Korean society of hypertension guidelines for the management of hypertension: Part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019;25:20. [Link] [DOI:10.1186/s40885-019-0124-x] [PMID] [PMCID]
11. Dhar L, Dantas J, Ali M. A systematic review of factors influencing medication adherence to hypertension treatment in developing countries. Open J Epidemiol. 2017;7(3):211-50. [Link] [DOI:10.4236/ojepi.2017.73018]
12. Baghianimoghadam M, Aivazi S, Mzloomy SS, Baghianimoghadam B. Factors in relation with self-regulation of hypertension, based on the model of goal directed behavior in Yazd city. J Med Life. 2011;4(1):30-5. [Link]
13. Li G, Hu R, Zhang X. Antihypertensive treatment with ACEI/ARB of patients with COVID-19 complicated by hypertension. Hypertens Res. 2020;1-3. [Link] [DOI:10.1038/s41440-020-0433-1] [PMID] [PMCID]
14. Klarenbach SW, McAlister FA, Johansen H, Tu K, Hazel M, Walker R, et al. Identification of factors driving differences in cost effectiveness of first-line pharmacological therapy for uncomplicated hypertension. Can J Cardiol. 2010;26(5):e158-63. [Link] [DOI:10.1016/S0828-282X(10)70383-4]
15. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-20. [Link] [DOI:10.1001/jama.2013.284427] [PMID]
16. Fattahi F, Kashkouli Behrouzi M, Zarrati M. Relation of body mass index, abdominal obesity, some nutritional habits and hypertension in 25-65 year old population of Tehran. KOOMESH. 2011;12(39):229-35. [Persian] [Link]
17. Gholami Fesharaki M, Rozati M, Tanhai AH. The longitudinal study of the relationship between work shift and blood pressure in workers of Mobarakeh Steel Company of Isfahan in 2007-2009. J Arak Uni Med Sci. 2011;13(4):68-74. [Persian] [Link]
18. Golabadi M, Dehghan F, Safakhah F, Attarchi MS. Assessment of effect of shift work on blood pressure in workers of a rubber manufacturing company. Razi J Med Sci. 2012;18(91):7-14. [Persian] [Link]
19. Rahimpour F, Jarahi L, Rafeemanesh E, Eghbali S. The effect of noise on blood pressure in the steel industry workers. Med J Mashhad Univ Med Sci. 2016;59(2):106-13. [Persian] [Link]
20. Bazyar F, Gholami-Fesharaki M, Rowzati M. The relationship between shift work and Framingham risk score: A five-year prospective cohort study. ARYA Atheroscler. 2017;13(6):288-94. [Link]
21. Khosravi A, Rowzati M, Gharipour M, Gholami Fesharaki M, Shirani Sh, Shahrokhi Sh, et al. Hypertension control in industrial employees: findings from SHIMSCO study. ARYA Atheroscler. 2012;7(4):191-6. [Link]
22. Echouffo-Tcheugui JB, Batty GD, Kivimäki M, Kengne AP. Risk models to predict hypertension: A systematic review. PLoS One. 2013;8(7):e67370. [Link] [DOI:10.1371/journal.pone.0067370] [PMID] [PMCID]
23. Gholami Fesharaki M, Kazemnejad A, Zayeri F, Sanati J, Akbari H. Historical cohort study on the factors affecting blood pressure in workers of polyacryl Iran corporation using bayesian multilevel modeling with skew T distribution. Iran Red Crescent Med J. 2013;15(5):418-23. [Link] [DOI:10.5812/ircmj.10930] [PMID] [PMCID]
24. Chia YC, Ching SM. Prevalence and predictors of resistant hypertension in a primary care setting: A cross-sectional study. BMC Fami Pract. 2014;15:131. [Link] [DOI:10.1186/1471-2296-15-131] [PMID] [PMCID]
25. Rezvan S, Besharati M, Khodadadpoor M, Matlabi M, Fathi A, Salimi A, et al. Self-care assessment of patients with hypertension in Qom city in 2016 (Iran). Qom Univ Med Sci J. 2018;12(4):72-80. [Persian] [Link] [DOI:10.29252/qums.12.4.72]
26. Newell M, Modeste N, Hopp Marshak H, Wilson C. Health beliefs and the prevention of hypertension in a black population living in London. Ethn Dis. 2009;19(1):35-41. [Link]
27. Fuladvandi M, Safarpour H, Malekyan L, Moayedi S, Askaryzadeh Mahani M, Salimi E. The survey of self-regulation behaviors and related factors in elderly with hypertension in the south-east of Iran. Sci Res. 2017;9(4):592. [Link] [DOI:10.4236/health.2017.94042]
28. Hazavehei MM, Dashti S, Moeini B, Faradmal J, Shahrabadi R, Yazdi AH. Factors related to self-care behaviors in hypertensive individuals based on Health Belief Model. KOOMESH. 2015;17(1):37-44. [Link]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |