Volume 9, Issue 1 (2021)
Health Educ Health Promot 2021, 9(1): 19-24 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Babadi F, Bazmi A, Araban M. Association between the Fear Induced by the COVID-19 and the Level of Depression, Anxiety, and Stress among Dental Students: A Cross-sectional Study. Health Educ Health Promot 2021; 9 (1) :19-24
URL: http://hehp.modares.ac.ir/article-5-47644-en.html
URL: http://hehp.modares.ac.ir/article-5-47644-en.html
1- Department of Oral and Maxillofacial Medicine, School of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2- Student Research Committee, School of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
3- “Department of Health Education and Promotion, School of Health”, and “Social determinants of Health Research Centre” Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran , arabanm@ajums.ac.ir
2- Student Research Committee, School of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
3- “Department of Health Education and Promotion, School of Health”, and “Social determinants of Health Research Centre” Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran , arabanm@ajums.ac.ir
Keywords: COVID-19 [MeSH], Stress [MeSH], Anxiety [MeSH], Depression [MeSH], Fear [MeSH], dental students [MeSH]
Full-Text [PDF 458 kb]
(1111 Downloads)
| Abstract (HTML) (2014 Views)
Full-Text: (539 Views)
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease first recognized in Wuhan (Hubei Province, China) in late 2019 [1]. The origin of COVID-19 was a new genetically modified virus from the coronavirus family called SARS-CoV-2, which was referred to as COVID-19 [1]. The pandemic has spread throughout Asia, Europe, Australia, United States, and Africa [2]. COVID-19 is recognized as a global threat to human health [3]. The disease is transmitted to humans through intermediate hosts such as bats [4]. However, there is still much more to know about the actual route of transmission [5]. COVID-19 causes severe respiratory infections in humans and is usually transmitted through person-to-person contact via hands, saliva, nasal secretions, droplets, and contact with contaminated surfaces.
The average incubation period for COVID-19 is varied from 4 to 14 days [6]. The most common clinical manifestations of COVID-19 are cough, fever, and dyspnea. Similarly, the loss of taste and/or smell and diarrhea are recognized as the symptoms of COVID-19 [7]. Pathogenic mechanisms of the virus, the extent of the outbreak, and the high mortality level of COVID-19 may influence the mental health of individuals at different layers of society, including patients, health care personnel, families, children, and students [8-10]. The disease may be associated with anxiety, depression, and stress [2]. Dentists have always been at the forefront of the spread of pathogens, especially in dental emergency clinics. So, the anxiety and fear of infection due to the COVID-19 pandemic among the dentists may be increased, especially in the dental offices [11]. Dentists are exposed to aerosols, droplets, and droplet/aerosol particles emitted during mouth breathing, so they are at high risk for serious infection from patients and can potentially spread the disease to family and other patients. Therefore, it is natural for dentists to experience a level of fear in the context of the COVID-19 pandemic [6, 12, 13]. University students are also susceptible to psychological symptoms during the COVID-19 outbreak. In the early phase of the COVID-19 outbreak, the closure of universities was one of the first and fundamental confinement measures [14]. The results of a study conducted on more than 7,000 students in China during the COVID-19 outbreak showed that about 24.9% of students experienced anxiety, of which about 9% had severe anxiety [15]. Since dental students are dealing with aerosol-generating procedures, they may be negatively affected by the fear of being infected by COVID-19 [16]. Fear is a natural and adaptive response to threat and danger, but when threat is continuous and ambiguous like the COVID-19 pandemic, fear can become chronic and overwhelming, i.e., leading to major health problems and enduring challenges for disease control [17]. The COVID-19 outbreak has greatly changed people's daily lives and global public health [18]. The present study aimed to evaluate the association between fear induced by the COVID-19 epidemic and the scores of stress and anxiety in dental students, which can be dynamic in planning and developing mental health strategies.
Instrument and Methods
This cross-sectional study was conducted in June 2020. A text message (SMS) was sent to all 420 dental students of Ahvaz Jundishapur University of Medical Sciences (AJUMS), southwest of Iran, to participate in the study. The SMS was sent via WhatsApp to the groups where the students' contact list was available. Since the time of study coincided with the midterm exams, at the request of students, the message was sent again to students who had not responded to the questionnaire during the first ten days, and the questionnaire was online for three weeks. The questionnaire was set so that the participants answer all questions; otherwise, they would not receive a confirmation message. The questionnaire was designed at URL: https://survey.porsline.ir. The questionnaire link (URL: https://survey.porsline.ir/8FsQfkv) was provided to all students via social networks (WhatsApp, Instagram) for two weeks. Students were informed through Student Representative Council (SRC) and SMS, and they were asked, if desired, to complete and send the questionnaire. At the request of the students, the questionnaire was extended for another week, and in total, the questionnaire was made available to students online for three weeks.
A three-part questionnaire was developed for data collection. The validity of the questionnaire was confirmed by content validity ratio (CVR) and content validity index (CVI) equal to 1, and the reliability of the questionnaire was confirmed with Cronbach's alpha=0.91 (range: 0.78–0.91).
The first part of the questionnaire included the background and demographic information, including age, gender, year of entry, residence status (dormitory/parents), medical history, monthly income (excellent/good, moderate, poor), underlying disease (Yes/No), grade point average (GPA), access to personal protective equipment (good, medium, inadequate), social support (good, medium, inadequate), feeling the media pressure caused by COVID-19 (low-medium-high), hand hygiene compliance (always/often/rarely/never), compliance with social distancing (always/often/rarely/never), and compliance with wearing face masks (always/ often/ rarely/ never).
The second part of the questionnaire consisted of the standard scale for measuring mental health (Depression, Anxiety, Stress: DASS-21), designed to focus on questionnaire measures of depression, anxiety, and stress. The reliability of the questionnaire was desirable; Cronbach's alpha=0.77. The questionnaire consisted of 3 components; each of the three scales contained seven items, divided into subscales with similar content. The final score of each item was obtained by summing the scores of each subscale. Response options were on a 4-point Likert scale (0=Did not apply to me at all – NEVER, 1=Applied to me to some degree, or some of the time – SOMETIMES, 2=Applied to me to a considerable degree, or a good part of the time – OFTEN, 3=Applied to me very much, or most of the time-ALMOST ALWAYS). The scoring method for each question was ranged from zero (does not apply to me at all) to 3 (absolutely applies to me), and the score of each subscale varied from 0 to 21. The higher score indicated the higher levels of generalized distress. The interpretation of scores was as follows: 0–9=normal in the depression subscale; 0-7=normal in the anxiety subscale; 0-14=normal in the stress subscale. This scale was previously validated in the previous study [19].
The third part of the questionnaire consisted of items related to the fear of the COVID-19 scale. This standard scale consisted of a seven-item scale, robust psychometric properties, and validated in a previous study [20]. The participants pointed out their level of agreement with the statements via a five-item Likert-type scale. Likert-scale questionnaire responses were as follows: 1=strongly disagree, 2=disagree, 3=either disagree or agree, 4=agree, 5=strongly agree. The minimum possible score for each question was one, and the maximum was 5. The total scale score was obtained by summing the scores of each question (from 7 to 35). The higher the score, the greater the fear of the COVID-19.
The total number of students in the dental school was 420. This questionnaire was given to all students. Finally, 229 (54.5%) students completed and sent the questionnaire. The sample size was calculated based on the rule of thumb theory of 3-10 participants per question [21]. Considering the 28 –item questionnaire, a sample of 220-230 was estimated to be necessarily anticipating a 10 percent dropout.
Shapiro-Wilk test was used to evaluate the normality of the data. ANCOVA analysis was used to analyze the effect of underlying variables on stress, anxiety, depression, and fear scores, and the MANCOVA analysis was used to measure the simultaneous effect of underlying variables by adjusting the effect of other variables. The post-hoc LSD test was used to compare the significance of variables. The significance level was set at α = .05. Data were analyzed using the IBM SPSS Version 22.0 (IBM Corp, Armonk, NY, USA).
The study procedure was approved by the Ethics Committee of AJUMS (Ethics Code: IR. AJUMS. REC. 1393. 323). Participation in the study was optional, and participants were assured that personal information would remain confidential. Informed consent was obtained from the participants.
Findings
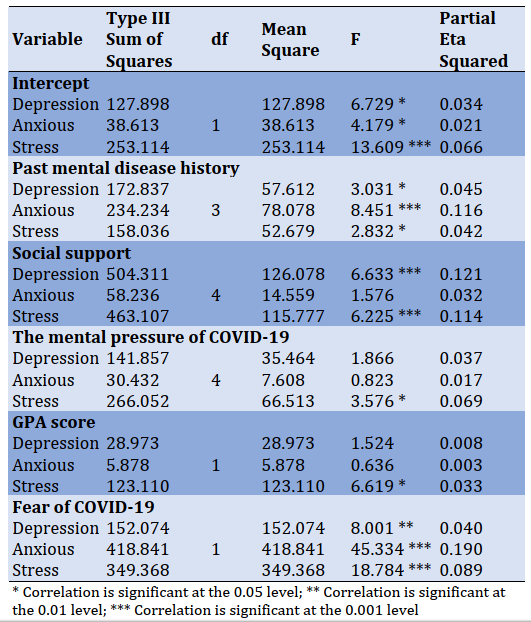
Out of 420 dental students, 229 participated in the study. The response rate was about 54.5%. Of the 229 students, 122 (53.3%) were female, and 107 (46.7%) were male. The mean age of the subjects was 22.9±3.31 years, and the minimum and maximum ages were 18 and 39 years, respectively. The highest frequency was related to single people, which included 207 (90.4%) students. 42% lived with the family, and 45% lived in dormitories. 23% of participants had a prior personal history of the disease. About 70% of participants had a good income level, and 20% had a lower income level than they need (Table 1). 88% of students did not have underlying health conditions. 43% of students were average, and 41% were in a good level of access to personal protective equipment. 30% of students were in average level, and 44% were in a good level of social support. In terms of COVID-19-induced media pressure, 19% were at the weak level, 37% at the medium level, and 25% were high.
Table 1) Background characteristics of the study population
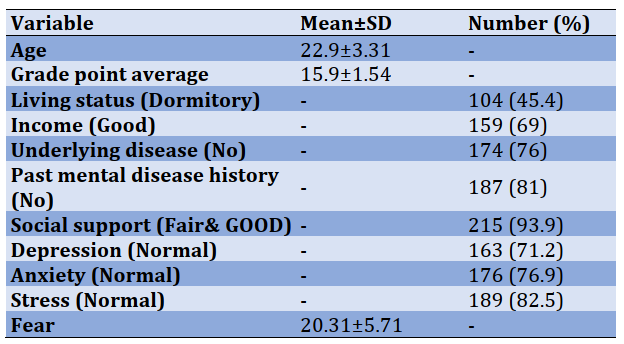
Table 2) Frequency of depression, anxiety, and stress scores among dental students
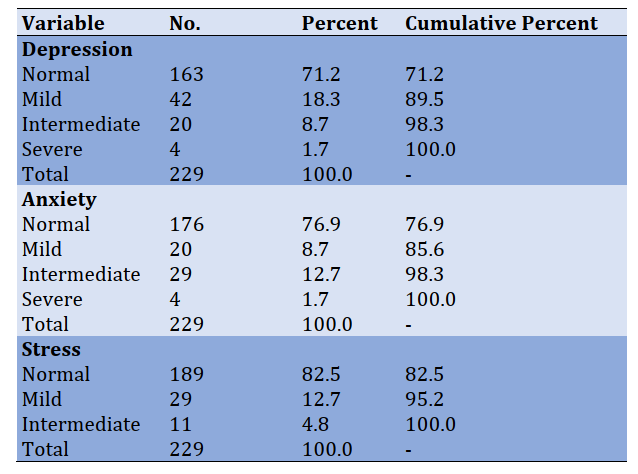
82% of students were mentally healthy, 1% were severely anxious, 1% were severely depressed, and 4.8% were severely stressed. The majority of
students had normal levels of depression (71.2%), stress (76.9%), and anxiety (82.5%; Table 2).
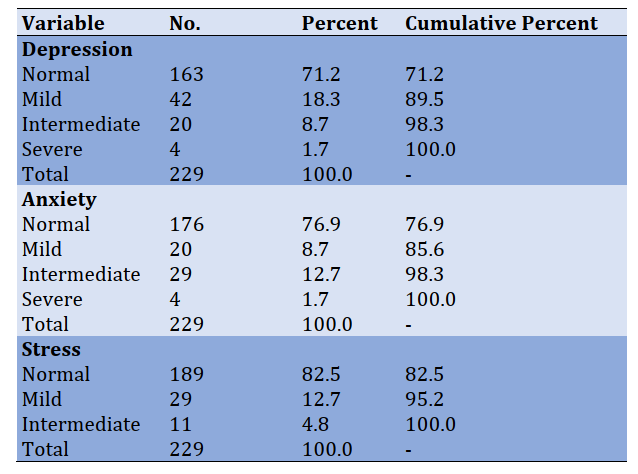
The results of the ANCOVA test regarding the analysis of the related factors of students anxiety status showed that history of mental health problems (anxiety scores were significantly higher when a person had a past clinical history (score=9.37) than when they had no clinical history (score=8.8), access to personal protective equipment (the highest level of anxiety was in poor access to personal protective equipment, and the lowest level of anxiety was in good (8.18) and fair (8.96) access to personal protective equipment, i.e., a significant difference was found between the two levels of good and fair at the level of 0.05 in the anxiety score), and COVID-19-induced media pressure (the highest level of anxiety was related to high media pressure from COVID-19 and the lowest level was related to low media pressure from COVID-19, poor media pressure=7.29, high media=11.39) had a significant effect on the level of anxiety. Other variables, including (residence, marital status, underlying disease, social support, age, and grade point average) did not significantly affect anxiety levels (Table 3).
The results of the ANCOVA test regarding the analysis of the related factors of students depression status showed that the history of mental health problems, social support, and COVID-19-induced media pressure had a significant effect on the level of depression (the highest rate of depression was related to the high contagion rate of COVID-19, Poor=9.86, Good=12.83). Other variables, including (gender, residence, marital status, history of underlying disease, and access to personal protective equipment, age, and grade point average) did not significantly affect the level of depression (Table 3).
The results of the ANCOVA test regarding the analysis of the related factors of students stress status showed that the history of mental health problems ( people with the history of disease were living more in fear of COVID-19, Yes=7.87, No=8.32), social support (the highest level of stress was related to the poor level of social support and the lowest level of stress was found at the good level of social support, Poor=16.86, Good=11.08), COVID-19-induced media pressure (the highest level of anxiety was related to high media pressure from COVID-19 and the lowest level was related to low media pressure from COVID-19, poor=9.27, High=17.49), and grade point average (GPA) had a significant effect on the level of stress. Other variables, including gender, residence, marital status, year of entry, underlying disease, history of the disease, access to personal protective equipment, and age, did not significantly affect the level of anxiety (Table 3).
Table 3) Correlation of anxiety, depression, and stress among dental students (Significant level=0.001)
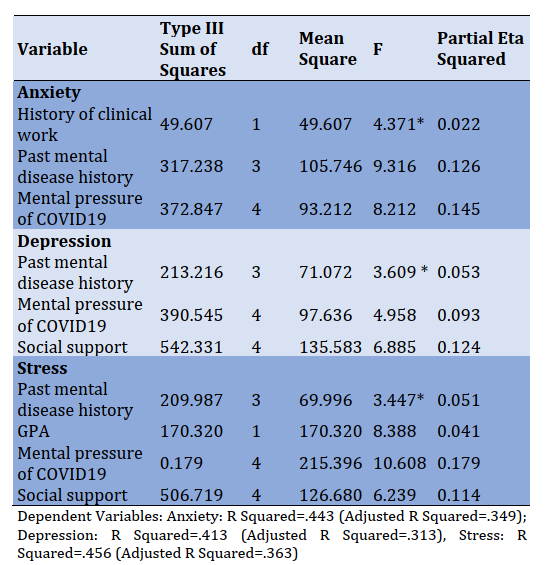
Table 4) Tests of between-subjects effects
The results of the MANCOVA test regarding the analysis of the related factors of student's fear of COVID-19 scale showed that underlying disease, the COVID-19-induced media pressure, and age had a significant effect on the level of fear of COVID-19. Other variables, including gender, residence, marital status, year of entry, history of disease, mental health problems, social support, access to personal protective equipment, and grade point average, did not significantly affect the level of fear of COVID-19
(Table 4). Furthermore, despite other research variables, the level of fear caused by the barrage of COVID-19 significantly affected the anxiety, depression, and stress scores, simultaneously (Table 4).
Discussion
The present study aimed to evaluate the association between fear induced by the COVID-19 epidemic and stress and anxiety scores among dental students. Studies have shown that public health crisis spurs fear, stress, and anxiety on students [22, 23]. The present study examined the association between mental health aspects and fear of the COVID-19 pandemic among dental students. The results showed that 29% of students during the COVID-19 outbreak had symptoms of anxiety, depression, and stress, and these statuses were associated with fear of COVID-19. A study conducted in China showed that 24.9% of college students experienced anxiety due to the COVID-19 outbreak, which was consistent with the results of the present study [15].
The present study also showed that the students' anxiety was associated with clinical work experience, access to personal protective equipment, and media pressure induced by COVID-19. Moreover, students with no clinical experience were more likely to experience fear. The reason could be explained due to poor perception of the real environment and magnification of risk perception.
At the moment of sampling, the COVID-19 pandemic was vastly spreading, so the sense of insufficient access to the equipment caused anxiety and stress in students, which was consistent with the results of the previous studies [8]. It has also been reported that the mass coverage media about the COVID-19 pandemic and personal protective equipment shortage, including masks, also cause fear and psychological reactions [24].
In this study, the history of mental health problems, social support, and COVID-19-induced media pressure significantly affected the level of depression and stress scores. It has been reported that people with underlying problems are more vulnerable to mental health problems [25]. Quarantine and lockdown reduce access with friends and relatives, leading to changes in communication behaviors and, consequently, mental health status disparities [26]. Likewise, as mentioned earlier, the COVID-19-induced media pressure, the sense of lack of social support, and feeling of loneliness due to quarantine can affect students' depression and stress scores.
Similarly, regarding the effects of COVID-19 on stress, GPA was associated with the level of stress among dental students, i.e., students with higher GPA may be more capable of managing stress than other students, or with more study, they may feel less stressed. Students' daily tasks consideration is also important to cope with mental health problems [27].
In this study, the history of underlying disease, the COVID-19-induced media pressure, and age significantly affected the degree of fear of COVID-19. Not having a history of underlying disease contributes to a higher level of fear of covid-19. Martens et al. [17] reported that the greater perceived overall health, the lower fear of covid-19, which was not consistent with the present study results. Different population background characteristics might justify the difference. Additionally, perceived media pressure contributed to fear of COVID-19. An earlier study showed that perceived media pressure contributed to fear of COVID-19 among students in Gaza Strip [28]. These might reflect the perceived susceptibility to covid-19 among this sub-group of the population.
It is reported that the elderly and people with underlying disease are most at risk of COVID-19. So, older adults and those with underlying diseases are more likely to fear COVID-19 [29].
In the present study, the level of fear caused by COVID-19 had a significant effect on the anxiety, depression, and stress scores, simultaneously. Ahorsu et al. suggested that fear was positively correlated with stress and depression [20].
Fear of disease causes psychological reactions and threatens mental health, and this factor exacerbates the disease and even causes the disease stigmatized, and as a result, it becomes more difficult to control and prevent the disease. So, developing promising fear-reduction strategies can be used as a method for mental health promotion.
Considering the importance of students' physical and mental health in providing dental services, this study can be effective in raising awareness of the mental health status of dental students. Moreover, it can provide new opportunities for intra-university policies to reduce students' fears and improve the quality of dental services. Also, explaining new safety policies to provide dental equipment and needs in full compliance with health protocols is effective for students' fear reduction.
In this study, due to the study's cross-sectional nature, the causal relationship between the variables was not possible. Cohort studies are recommended to determine the relationship between mental health during the COVID-19 pandemic. According to the sampling method, the results cannot be generalized to all dental students.
Conclusion
Fear of disease causes a psychological reaction and threatens mental health and might make coping with the disease more difficult; promising fear-reduction strategies are recommended during the COVID-19 pandemic mental health for dental students. Therefore, targeting and tailoring health education programs are recommended to improve dental students' mental health during the pandemic.
Acknowledgments: We appreciate all the students who helped us to conduct this project.
Ethical Permissions: The present study (U-99109) was conducted with the approval of the ethical committee of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran (Ethics Code: IR.AJUMS.REC.1399.323).
Conflict of Interests: The authors declare no competing interest.
Authors' Contributions: Babadi F. (First author), Introduction author/Methodologist/Original researcher (40%); Bazmi A. (Second author), Introduction author/
Assistant researcher (15%); Araban M. (Third author), Methodologist/Original researcher/Statistical analyst/
Discussion author (45%).
Funding/Sources: Financial support was provided by the Vive-Chancellor for Research at Ahvaz Jundishapur University of Medical Sciences grant number U-99109.
Coronavirus disease 2019 (COVID-19) is an infectious disease first recognized in Wuhan (Hubei Province, China) in late 2019 [1]. The origin of COVID-19 was a new genetically modified virus from the coronavirus family called SARS-CoV-2, which was referred to as COVID-19 [1]. The pandemic has spread throughout Asia, Europe, Australia, United States, and Africa [2]. COVID-19 is recognized as a global threat to human health [3]. The disease is transmitted to humans through intermediate hosts such as bats [4]. However, there is still much more to know about the actual route of transmission [5]. COVID-19 causes severe respiratory infections in humans and is usually transmitted through person-to-person contact via hands, saliva, nasal secretions, droplets, and contact with contaminated surfaces.
The average incubation period for COVID-19 is varied from 4 to 14 days [6]. The most common clinical manifestations of COVID-19 are cough, fever, and dyspnea. Similarly, the loss of taste and/or smell and diarrhea are recognized as the symptoms of COVID-19 [7]. Pathogenic mechanisms of the virus, the extent of the outbreak, and the high mortality level of COVID-19 may influence the mental health of individuals at different layers of society, including patients, health care personnel, families, children, and students [8-10]. The disease may be associated with anxiety, depression, and stress [2]. Dentists have always been at the forefront of the spread of pathogens, especially in dental emergency clinics. So, the anxiety and fear of infection due to the COVID-19 pandemic among the dentists may be increased, especially in the dental offices [11]. Dentists are exposed to aerosols, droplets, and droplet/aerosol particles emitted during mouth breathing, so they are at high risk for serious infection from patients and can potentially spread the disease to family and other patients. Therefore, it is natural for dentists to experience a level of fear in the context of the COVID-19 pandemic [6, 12, 13]. University students are also susceptible to psychological symptoms during the COVID-19 outbreak. In the early phase of the COVID-19 outbreak, the closure of universities was one of the first and fundamental confinement measures [14]. The results of a study conducted on more than 7,000 students in China during the COVID-19 outbreak showed that about 24.9% of students experienced anxiety, of which about 9% had severe anxiety [15]. Since dental students are dealing with aerosol-generating procedures, they may be negatively affected by the fear of being infected by COVID-19 [16]. Fear is a natural and adaptive response to threat and danger, but when threat is continuous and ambiguous like the COVID-19 pandemic, fear can become chronic and overwhelming, i.e., leading to major health problems and enduring challenges for disease control [17]. The COVID-19 outbreak has greatly changed people's daily lives and global public health [18]. The present study aimed to evaluate the association between fear induced by the COVID-19 epidemic and the scores of stress and anxiety in dental students, which can be dynamic in planning and developing mental health strategies.
Instrument and Methods
This cross-sectional study was conducted in June 2020. A text message (SMS) was sent to all 420 dental students of Ahvaz Jundishapur University of Medical Sciences (AJUMS), southwest of Iran, to participate in the study. The SMS was sent via WhatsApp to the groups where the students' contact list was available. Since the time of study coincided with the midterm exams, at the request of students, the message was sent again to students who had not responded to the questionnaire during the first ten days, and the questionnaire was online for three weeks. The questionnaire was set so that the participants answer all questions; otherwise, they would not receive a confirmation message. The questionnaire was designed at URL: https://survey.porsline.ir. The questionnaire link (URL: https://survey.porsline.ir/8FsQfkv) was provided to all students via social networks (WhatsApp, Instagram) for two weeks. Students were informed through Student Representative Council (SRC) and SMS, and they were asked, if desired, to complete and send the questionnaire. At the request of the students, the questionnaire was extended for another week, and in total, the questionnaire was made available to students online for three weeks.
A three-part questionnaire was developed for data collection. The validity of the questionnaire was confirmed by content validity ratio (CVR) and content validity index (CVI) equal to 1, and the reliability of the questionnaire was confirmed with Cronbach's alpha=0.91 (range: 0.78–0.91).
The first part of the questionnaire included the background and demographic information, including age, gender, year of entry, residence status (dormitory/parents), medical history, monthly income (excellent/good, moderate, poor), underlying disease (Yes/No), grade point average (GPA), access to personal protective equipment (good, medium, inadequate), social support (good, medium, inadequate), feeling the media pressure caused by COVID-19 (low-medium-high), hand hygiene compliance (always/often/rarely/never), compliance with social distancing (always/often/rarely/never), and compliance with wearing face masks (always/ often/ rarely/ never).
The second part of the questionnaire consisted of the standard scale for measuring mental health (Depression, Anxiety, Stress: DASS-21), designed to focus on questionnaire measures of depression, anxiety, and stress. The reliability of the questionnaire was desirable; Cronbach's alpha=0.77. The questionnaire consisted of 3 components; each of the three scales contained seven items, divided into subscales with similar content. The final score of each item was obtained by summing the scores of each subscale. Response options were on a 4-point Likert scale (0=Did not apply to me at all – NEVER, 1=Applied to me to some degree, or some of the time – SOMETIMES, 2=Applied to me to a considerable degree, or a good part of the time – OFTEN, 3=Applied to me very much, or most of the time-ALMOST ALWAYS). The scoring method for each question was ranged from zero (does not apply to me at all) to 3 (absolutely applies to me), and the score of each subscale varied from 0 to 21. The higher score indicated the higher levels of generalized distress. The interpretation of scores was as follows: 0–9=normal in the depression subscale; 0-7=normal in the anxiety subscale; 0-14=normal in the stress subscale. This scale was previously validated in the previous study [19].
The third part of the questionnaire consisted of items related to the fear of the COVID-19 scale. This standard scale consisted of a seven-item scale, robust psychometric properties, and validated in a previous study [20]. The participants pointed out their level of agreement with the statements via a five-item Likert-type scale. Likert-scale questionnaire responses were as follows: 1=strongly disagree, 2=disagree, 3=either disagree or agree, 4=agree, 5=strongly agree. The minimum possible score for each question was one, and the maximum was 5. The total scale score was obtained by summing the scores of each question (from 7 to 35). The higher the score, the greater the fear of the COVID-19.
The total number of students in the dental school was 420. This questionnaire was given to all students. Finally, 229 (54.5%) students completed and sent the questionnaire. The sample size was calculated based on the rule of thumb theory of 3-10 participants per question [21]. Considering the 28 –item questionnaire, a sample of 220-230 was estimated to be necessarily anticipating a 10 percent dropout.
Shapiro-Wilk test was used to evaluate the normality of the data. ANCOVA analysis was used to analyze the effect of underlying variables on stress, anxiety, depression, and fear scores, and the MANCOVA analysis was used to measure the simultaneous effect of underlying variables by adjusting the effect of other variables. The post-hoc LSD test was used to compare the significance of variables. The significance level was set at α = .05. Data were analyzed using the IBM SPSS Version 22.0 (IBM Corp, Armonk, NY, USA).
The study procedure was approved by the Ethics Committee of AJUMS (Ethics Code: IR. AJUMS. REC. 1393. 323). Participation in the study was optional, and participants were assured that personal information would remain confidential. Informed consent was obtained from the participants.
Findings
Out of 420 dental students, 229 participated in the study. The response rate was about 54.5%. Of the 229 students, 122 (53.3%) were female, and 107 (46.7%) were male. The mean age of the subjects was 22.9±3.31 years, and the minimum and maximum ages were 18 and 39 years, respectively. The highest frequency was related to single people, which included 207 (90.4%) students. 42% lived with the family, and 45% lived in dormitories. 23% of participants had a prior personal history of the disease. About 70% of participants had a good income level, and 20% had a lower income level than they need (Table 1). 88% of students did not have underlying health conditions. 43% of students were average, and 41% were in a good level of access to personal protective equipment. 30% of students were in average level, and 44% were in a good level of social support. In terms of COVID-19-induced media pressure, 19% were at the weak level, 37% at the medium level, and 25% were high.
Table 1) Background characteristics of the study population
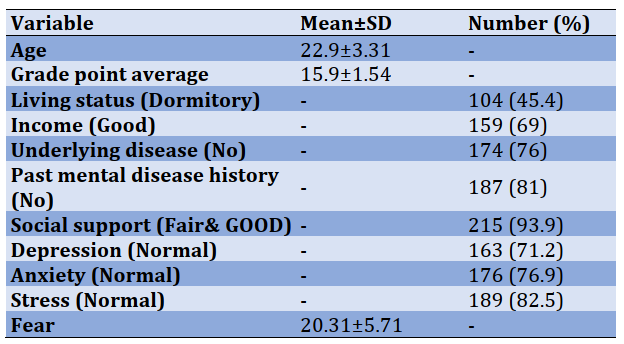
Table 2) Frequency of depression, anxiety, and stress scores among dental students
82% of students were mentally healthy, 1% were severely anxious, 1% were severely depressed, and 4.8% were severely stressed. The majority of
students had normal levels of depression (71.2%), stress (76.9%), and anxiety (82.5%; Table 2).
The results of the ANCOVA test regarding the analysis of the related factors of students anxiety status showed that history of mental health problems (anxiety scores were significantly higher when a person had a past clinical history (score=9.37) than when they had no clinical history (score=8.8), access to personal protective equipment (the highest level of anxiety was in poor access to personal protective equipment, and the lowest level of anxiety was in good (8.18) and fair (8.96) access to personal protective equipment, i.e., a significant difference was found between the two levels of good and fair at the level of 0.05 in the anxiety score), and COVID-19-induced media pressure (the highest level of anxiety was related to high media pressure from COVID-19 and the lowest level was related to low media pressure from COVID-19, poor media pressure=7.29, high media=11.39) had a significant effect on the level of anxiety. Other variables, including (residence, marital status, underlying disease, social support, age, and grade point average) did not significantly affect anxiety levels (Table 3).
The results of the ANCOVA test regarding the analysis of the related factors of students depression status showed that the history of mental health problems, social support, and COVID-19-induced media pressure had a significant effect on the level of depression (the highest rate of depression was related to the high contagion rate of COVID-19, Poor=9.86, Good=12.83). Other variables, including (gender, residence, marital status, history of underlying disease, and access to personal protective equipment, age, and grade point average) did not significantly affect the level of depression (Table 3).
The results of the ANCOVA test regarding the analysis of the related factors of students stress status showed that the history of mental health problems ( people with the history of disease were living more in fear of COVID-19, Yes=7.87, No=8.32), social support (the highest level of stress was related to the poor level of social support and the lowest level of stress was found at the good level of social support, Poor=16.86, Good=11.08), COVID-19-induced media pressure (the highest level of anxiety was related to high media pressure from COVID-19 and the lowest level was related to low media pressure from COVID-19, poor=9.27, High=17.49), and grade point average (GPA) had a significant effect on the level of stress. Other variables, including gender, residence, marital status, year of entry, underlying disease, history of the disease, access to personal protective equipment, and age, did not significantly affect the level of anxiety (Table 3).
Table 3) Correlation of anxiety, depression, and stress among dental students (Significant level=0.001)
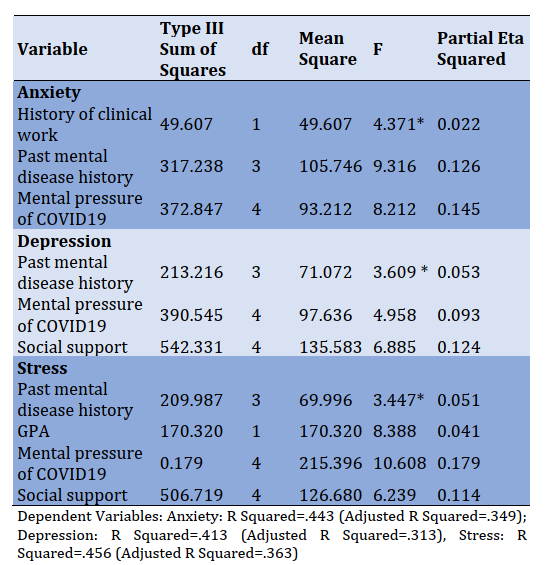
Table 4) Tests of between-subjects effects
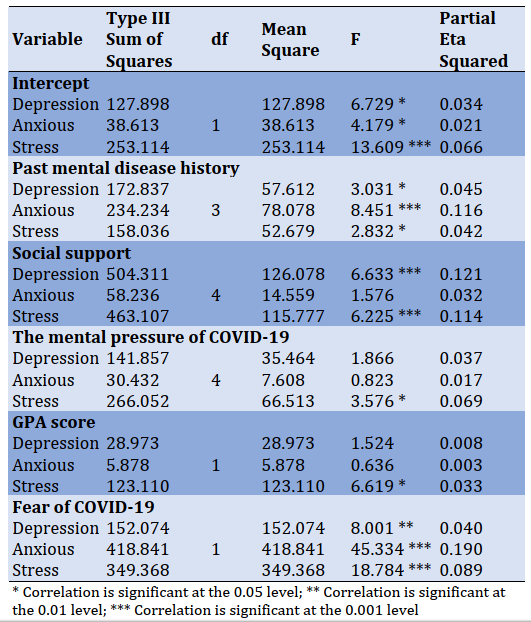
The results of the MANCOVA test regarding the analysis of the related factors of student's fear of COVID-19 scale showed that underlying disease, the COVID-19-induced media pressure, and age had a significant effect on the level of fear of COVID-19. Other variables, including gender, residence, marital status, year of entry, history of disease, mental health problems, social support, access to personal protective equipment, and grade point average, did not significantly affect the level of fear of COVID-19
(Table 4). Furthermore, despite other research variables, the level of fear caused by the barrage of COVID-19 significantly affected the anxiety, depression, and stress scores, simultaneously (Table 4).
Discussion
The present study aimed to evaluate the association between fear induced by the COVID-19 epidemic and stress and anxiety scores among dental students. Studies have shown that public health crisis spurs fear, stress, and anxiety on students [22, 23]. The present study examined the association between mental health aspects and fear of the COVID-19 pandemic among dental students. The results showed that 29% of students during the COVID-19 outbreak had symptoms of anxiety, depression, and stress, and these statuses were associated with fear of COVID-19. A study conducted in China showed that 24.9% of college students experienced anxiety due to the COVID-19 outbreak, which was consistent with the results of the present study [15].
The present study also showed that the students' anxiety was associated with clinical work experience, access to personal protective equipment, and media pressure induced by COVID-19. Moreover, students with no clinical experience were more likely to experience fear. The reason could be explained due to poor perception of the real environment and magnification of risk perception.
At the moment of sampling, the COVID-19 pandemic was vastly spreading, so the sense of insufficient access to the equipment caused anxiety and stress in students, which was consistent with the results of the previous studies [8]. It has also been reported that the mass coverage media about the COVID-19 pandemic and personal protective equipment shortage, including masks, also cause fear and psychological reactions [24].
In this study, the history of mental health problems, social support, and COVID-19-induced media pressure significantly affected the level of depression and stress scores. It has been reported that people with underlying problems are more vulnerable to mental health problems [25]. Quarantine and lockdown reduce access with friends and relatives, leading to changes in communication behaviors and, consequently, mental health status disparities [26]. Likewise, as mentioned earlier, the COVID-19-induced media pressure, the sense of lack of social support, and feeling of loneliness due to quarantine can affect students' depression and stress scores.
Similarly, regarding the effects of COVID-19 on stress, GPA was associated with the level of stress among dental students, i.e., students with higher GPA may be more capable of managing stress than other students, or with more study, they may feel less stressed. Students' daily tasks consideration is also important to cope with mental health problems [27].
In this study, the history of underlying disease, the COVID-19-induced media pressure, and age significantly affected the degree of fear of COVID-19. Not having a history of underlying disease contributes to a higher level of fear of covid-19. Martens et al. [17] reported that the greater perceived overall health, the lower fear of covid-19, which was not consistent with the present study results. Different population background characteristics might justify the difference. Additionally, perceived media pressure contributed to fear of COVID-19. An earlier study showed that perceived media pressure contributed to fear of COVID-19 among students in Gaza Strip [28]. These might reflect the perceived susceptibility to covid-19 among this sub-group of the population.
It is reported that the elderly and people with underlying disease are most at risk of COVID-19. So, older adults and those with underlying diseases are more likely to fear COVID-19 [29].
In the present study, the level of fear caused by COVID-19 had a significant effect on the anxiety, depression, and stress scores, simultaneously. Ahorsu et al. suggested that fear was positively correlated with stress and depression [20].
Fear of disease causes psychological reactions and threatens mental health, and this factor exacerbates the disease and even causes the disease stigmatized, and as a result, it becomes more difficult to control and prevent the disease. So, developing promising fear-reduction strategies can be used as a method for mental health promotion.
Considering the importance of students' physical and mental health in providing dental services, this study can be effective in raising awareness of the mental health status of dental students. Moreover, it can provide new opportunities for intra-university policies to reduce students' fears and improve the quality of dental services. Also, explaining new safety policies to provide dental equipment and needs in full compliance with health protocols is effective for students' fear reduction.
In this study, due to the study's cross-sectional nature, the causal relationship between the variables was not possible. Cohort studies are recommended to determine the relationship between mental health during the COVID-19 pandemic. According to the sampling method, the results cannot be generalized to all dental students.
Conclusion
Fear of disease causes a psychological reaction and threatens mental health and might make coping with the disease more difficult; promising fear-reduction strategies are recommended during the COVID-19 pandemic mental health for dental students. Therefore, targeting and tailoring health education programs are recommended to improve dental students' mental health during the pandemic.
Acknowledgments: We appreciate all the students who helped us to conduct this project.
Ethical Permissions: The present study (U-99109) was conducted with the approval of the ethical committee of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran (Ethics Code: IR.AJUMS.REC.1399.323).
Conflict of Interests: The authors declare no competing interest.
Authors' Contributions: Babadi F. (First author), Introduction author/Methodologist/Original researcher (40%); Bazmi A. (Second author), Introduction author/
Assistant researcher (15%); Araban M. (Third author), Methodologist/Original researcher/Statistical analyst/
Discussion author (45%).
Funding/Sources: Financial support was provided by the Vive-Chancellor for Research at Ahvaz Jundishapur University of Medical Sciences grant number U-99109.
Article Type: Original Research |
Subject:
Oral Health Education/Promotion
Received: 2020/11/14 | Accepted: 2021/01/11 | Published: 2021/05/8
Received: 2020/11/14 | Accepted: 2021/01/11 | Published: 2021/05/8
References
1. Zhu H, Wei L, Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy. 2020;5(1):1-3. [Link] [DOI:10.1186/s41256-020-00135-6] [PMID] [PMCID]
2. Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124. [Link] [DOI:10.1016/j.sleep.2020.04.019] [PMID] [PMCID]
3. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470-3. [Link] [DOI:10.1016/S0140-6736(20)30185-9]
4. Paules CI, Marston HD, Fauci AS. Coronavirus infections-more than just the common cold. Jama. 2020;323(8):707-8. [Link] [DOI:10.1001/jama.2020.0757] [PMID]
5. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. [Link] [DOI:10.1016/S0140-6736(20)30183-5]
6. Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS, et al. Fear and practice modifications among dentists to combat novel Coronavirus Disease (COVID-19) outbreak. Int J Environ Res Public Health. 2020;17(8):2821. [Link] [DOI:10.3390/ijerph17082821] [PMID] [PMCID]
7. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. New Engl J Med. 2020;382(18):1708-20. [Link] [DOI:10.1056/NEJMoa2002032] [PMID] [PMCID]
8. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet. 2020;395(10224):e37-8. [Link] [DOI:10.1016/S0140-6736(20)30309-3]
9. Ryu S, Chun BC, Korean Society of Epidemiology 2019-nCoV Task Force Team. An interim review of the epidemiological characteristics of 2019 novel coronavirus. Epidemiol Health. 2020;42:e2020006. [Link] [DOI:10.4178/epih.e2020006] [PMID] [PMCID]
10. Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15-6. [Link] [DOI:10.1016/S2215-0366(20)30078-X]
11. Saquib Mulla D, Shaju S, Bathija S, Poothulil N. Prevalence of anxiety and fear in living with COVID-19 virus from the perspective of practicing dentists: A short study. Int J Appl Dent Sci. 2020;6(3):19-22. [Link]
12. Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus disease 19 (COVID-19): Implications for clinical dental care. J Endod. 2020;46(5):584-95. [Link] [DOI:10.1016/j.joen.2020.03.008] [PMID] [PMCID]
13. Bescos R, Casas-Agustench P, Belfield L, Brookes Z, Gabaldón T. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(9):1113. [Link] [DOI:10.1177/0022034520932149] [PMID]
14. Shahyad S, Mohammadi MT. Psychological impacts of Covid-19 outbreak on mental health status of society individuals: A narrative review. J Mil Med. 2020;22(2):184-92. [Persian] [Link]
15. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. [Link] [DOI:10.1016/j.psychres.2020.112934] [PMID] [PMCID]
16. Alzahrani SB, Alrusayes AA, Aldossary MS. Impact of COVID-19 pandemic on dental education, research, and students. Int J Health Sci Res. 2020;10(6):207-12. [Persian] [Link]
17. Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J Anxiety Disord. 2020;74:102258. [Link] [DOI:10.1016/j.janxdis.2020.102258] [PMID] [PMCID]
18. Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. depression, anxiety and stress during covid-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(11):4065. [Link] [DOI:10.3390/ijerph17114065] [PMID] [PMCID]
19. Asghari A, Saed F, Dibajnia P. Psychometric properties of the Depression Anxiety Stress Scales-21 (DASS-21) in a non-clinical Iranian sample. Int J Psychol. 2008;2(2):82-102. [Persian] [Link]
20. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: Development and initial validation. Int J Ment Health Addict. 2020. [Link] [DOI:10.1007/s11469-020-00270-8]
21. Jasemzadeh M, Jaafarzadeh N, Khafaie MA, Malehi AS, Araban M. Predicator of pregnant women's self-care behavior against air pollution: An explanation based on the Extended Parallel Process Model (EPPM). Electron Physician. 2016;8(9):2871-7. [Link] [DOI:10.19082/2871] [PMID] [PMCID]
22. Wang C, Zhao H. The impact of COVID-19 on anxiety in Chinese University students. Front Psychol. 2020;11:1168. [Link] [DOI:10.3389/fpsyg.2020.01168] [PMID] [PMCID]
23. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. [Link] [DOI:10.3390/ijerph17051729] [PMID] [PMCID]
24. Ayittey FK, Ayittey MK, Chiwero NB, Kamasah JS, Dzuvor C. Economic impacts of Wuhan 2019‐nCoV on China and the world. J Med Virol. 2020;92(5):473-5. [Link] [DOI:10.1002/jmv.25706] [PMID] [PMCID]
25. Wang Y, Duan Z, Ma Z, Mao Y, Li X, Wilson A, et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl Psychiatry. 2020;10:263. [Link] [DOI:10.1038/s41398-020-00950-y] [PMID] [PMCID]
26. Huckins J, Hedlund EL, Rogers C, Nepal SK, Wu J, Obuchi M, et al. Mental health and behavior during the early phases of the COVID-19 pandemic: A longitudinal mobile smartphone and ecological momentary assessment study in college students. J Med Internet Res. 2020. [Link] [DOI:10.31234/osf.io/4enzm]
27. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4(6):421. [Link] [DOI:10.1016/S2352-4642(20)30109-7]
28. Radwan E, Radwan A, Radwan W. The role of social media in spreading panic among primary and secondary school students during the COVID-19 pandemic: An online questionnaire study from the Gaza Strip, Palestine. Heliyon. 2020;6(12):e05807. [Link] [DOI:10.1016/j.heliyon.2020.e05807] [PMID] [PMCID]
29. Jordan RE, Adab P, Cheng KK. Covid-19: Risk factors for severe disease and death. BMJ. 2020;368:m1198. [Link] [DOI:10.1136/bmj.m1198] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |