Volume 9, Issue 1 (2021)
Health Educ Health Promot 2021, 9(1): 61-66 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Soheili B, Mirzaei A, Sayehmiri K, Montazeri A, Araban M, Ghazanfari Z. A Randomized Controlled Trial of a Theory-Based Health Education on Prevention of Elective Cesareans in Iran. Health Educ Health Promot 2021; 9 (1) :61-66
URL: http://hehp.modares.ac.ir/article-5-47306-en.html
URL: http://hehp.modares.ac.ir/article-5-47306-en.html
1- Department of Public Health, School of Health, Ilam University of Medical Sciences, Ilam, Iran
2- Department of Biostatistics, School of Health, Ilam University of Medical Sciences, Ilam, Iran
3- Mental Health Research Group, Health Metrics Research Centre, Iranian Institute for Health Sciences Research (ACECR), Tehran, Iran
4- Department of Health Education and Promotion, Public Health School, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
5- Department of Public Health, School of Health, Ilam University of Medical Sciences, Ilam, Iran ,ghazanfari-z@medilam.ac.ir
2- Department of Biostatistics, School of Health, Ilam University of Medical Sciences, Ilam, Iran
3- Mental Health Research Group, Health Metrics Research Centre, Iranian Institute for Health Sciences Research (ACECR), Tehran, Iran
4- Department of Health Education and Promotion, Public Health School, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
5- Department of Public Health, School of Health, Ilam University of Medical Sciences, Ilam, Iran ,
Keywords: Health Behavior [MeSH], Health Education [MeSH], Natural Childbirth [MeSH], Cesarean Section [MeSH]
Full-Text [PDF 482 kb]
(3968 Downloads)
| Abstract (HTML) (3142 Views)
Full-Text: (578 Views)
Introduction
Childbirth is a natural process. Monitoring and controlling natural delivery makes it possible to administer appropriate and timely treatment in cases of complications [1]. If natural childbirth is not viable, then cesarean section (CS) is suggested for the safety of mothers and babies. CS means surgical removal of the fetus from the abdomen and uterus walls [2]. However, in general, complications of elective cesarean section are more than normal delivery. Complications of CS delivery include bleeding, infection, maternal and infant mortality, postpartum depression, respiratory distress syndrome in infants, and higher economic cost for families [3-5].
The World Health Organization (WHO) has announced that 10-15% is an acceptable rate of CS for nulliparous women [6]. Despite this, the existing information shows that CS rates exceed this acceptable WHO standard in many countries [7]. In Iran, the rate is three times more than the global average [8].
Numerous factors may contribute to increased rates of CS. These include the socio-economic status of women, maternal age during the first pregnancy, doctor's concern regarding mother's conditions, legal matters, financial incentives, inadequate knowledge, negative attitudes of mothers towards vaginal childbirth, and mother's tendency to cesarean delivery [2, 9-13]. Thus, to evaluate how these factors could be influenced to reduce unnecessary cesarean delivery, some theory-based educational interventions are proposed [7]. One such intervention is educational programs using the Theory of Planned Behavior (TPB). For instance, studies conducted by Shahraki-Sanavi et al. [14], and Besharati et al. [15] demonstrated that such programs might be successful in changing women's attitudes normal delivery. However, more studies are needed to confirm these results.
While the WHO advocates no more than 10-15% rates for CS, a systematic review by studying 197514 pregnant women announced prevalence of CS in Iran equal to 48% that is much higher than its recommended levels [16, 17]. Some initiatives, including free-of-charge normal vaginal delivery (NVD), started on May 6, 2014, by the Iran Ministry of Health to limit CS and promote NVD. With the implementation in the ministry's approach, only a 6% increase in the percentage of NVD was achieved [18], and the rate of CS remains high. Therefore, interventions are needed to promote NVD to achieve WHO and ministry of health standard CS standards.
Considering the maternal and neonatal effects of CS [19, 20] and the WHO's recommendation on non-clinical interventions such as psychoeducation [21], the current study aims to evaluate the effect of theory-based health education on the prevention of elective cesarean sections among a sample of Iranian women referred to health care centers in Kermanshah.
Materials and Methods
This was a parallel randomized trial conducted on a sample of nulliparous pregnant women at the gestational age of 28-36 weeks, referred to health care centers in Kermanshah, a province in the west of Iran. The study flowchart is also presented in Diagram 1.
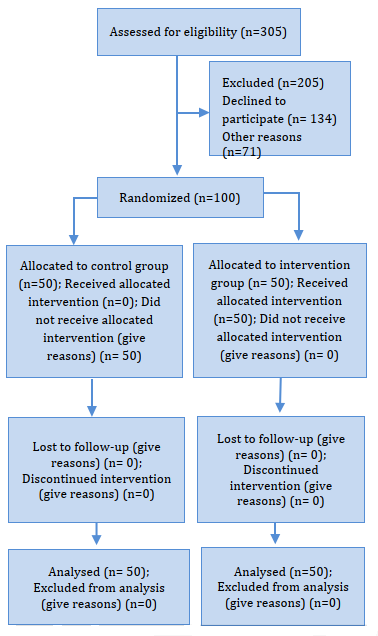
Figure 1) Flow diagram of the study participants
The study sample, which began in December 2015 and ended in October 2016, was taken from eight health care centers. The health centers were initially selected through the roll of a die. Four centers were allocated as the intervention group and four as the control group in a randomized manner. Health care centers, which formed the framework for selecting participants in intervention and control groups, were the same regarding economic, social, and cultural conditions.
Inclusion criteria were as follows: being nulliparous at the gestational age range of 28-36 weeks; and age between 18-35. Exclusion criteria included contraindication to NVD, premature childbirth, incomplete questionnaire, and absence from training sessions.
The intervention consisted of three training sessions in 2 weeks. The first session was held to provide a favorable attitude towards natural childbirth. The explanations about delivery methods, cesarean section indications, the advantages and disadvantages of each method were presented for pregnant women with the lecture method in one hour. Then they were asked to express their opinions, beliefs, and concerns about the issue in a group discussion session which lasted for one hour and a half.
The subject of the second session was to learn feasible methods for pain reduction to enhance mothers' perception of behavioral control. In this session, they helped learn breathing and relaxation techniques and master it through practical exercises. This session also lasted for one hour and thirteen minutes.
In order to influence perceived behavioral control, Training pain relief techniques such as deep breathing, relaxation, and the massage was done in two 90-minute sessions. The researcher taught these techniques, and then the group practiced them to learn them.
In order to affect subjective norms, pregnant women were asked to attend a meeting with a friend or family member. Participating in training sessions with friends or family members who have a major role in their decision-making was a technique to affect their subjective norms. A pamphlet was designed to help women were attending sessions alone. These people could support and reinforce them to select natural childbirth.
In each session, a time is specified to review the content and answer their questions. The control group received only standard care led by midwives at health care centers. Standard care included examinations of maternal weight, fundal height, FHR auscultation, education and screening for alarm signs in late pregnancy, and education about delivery and infant care were provided to women. Data on variables of TPB were gathered at baseline and 1-month follow-up. In order to find their delivery method, each mother also received a phone call after childbirth to record their delivery method.
The data collection instrument involved a two-section questionnaire including 50 items. The first section had 9 items related to demographic and obstetric questions. The second section included questions related to TPB's variables. This section included attitude with 8 questions (behavioral beliefs: 8Q, outcome evaluation: 8Q), subjective norms with 5 questions (normative beliefs: 5Q, motivations to comply: 5Q), perceived behavioral
control with 6 questions (control beliefs: 6Q, perceived power: 6Q), and behavioral intention with 3 Questions. The answers to the questions of this part were set on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree) . The possible range of scores was 8 to 200 for attitude, 5 to 125 for subjective norms, 6 to 150 for perceived behavioral control, and 3 to 15 for behavioral intention. The scoring was set as Ajzen's TPB questionnaire construction [22].
Content validity was evaluated based on experts' comments, and essential modifications were made. Reliability was also evaluated by Cronbach's alpha. The Cronbach coefficient was 0.82 for attitude, 0.77 for subjective norm, 0.70 for perceived behavioral control, and 0.84 for behavioral intention. Answering each questionnaire by the researcher required 10 to 15 minutes through an interview. This process was done two times, before and after the intervention.
A sample of 43 pregnant women was estimated per each group, according to the percent of elective C-section in intervention and control group as 6% and 28%, alpha and beta errors equal to 0.05 and 0.1 using the following statistical formula [23]:
To increase the power of the test to 86%, the sample size was increased to 50 in each group.
Data were analyzed by SPSS software. The normal distribution of data was controlled by the Kolmogorov-Smirnov test. To compare demographic data of the intervention and control groups before the intervention, the independent t-test and chi-square were applied. Paired t-test was used to compare the pre-test and post-test scores of attitude, subjective norms, perceived behavioral control, and behavioral intention in each group. Due to the difference between groups in terms of income, the analysis of covariance test was used to adjust income variable and pre-test data. Finally, a comparison of the type of delivery (including NVD, emergency cesarean section, and elective cesarean section) was done using the Chi-square test between groups.
Approval for this research was acquired through Ilam University of Medical Sciences Ethics Committee (EC Ref No: Ec/94/H/291). Objectives of the study were outlined at the beginning of the study. Written informed consent was obtained from participants, confidentiality of information was ensured, and participants were given authority to withdraw from the study if they were exposed to problems that might have hindered their participation.
Findings
In this work, 100 pregnant women have participated. Mean±SD for the women's age was 22.78±3.68 years. There was no significant difference between the two groups in terms of age, job and education status of women and their spouse, and planned pregnancy (p>0.05), but there was a significant difference between groups in terms of income (p<0.05; Table 1).
Table 2 shows the mean scores of outcome variables for the intervention and control groups at baseline and one-month follow-up. Results showed significant differences at follow-up for the mean scores of attitude, subjective norms, perceived behavioral control (p≤0.001), and behavioral intention (p≤0.01) between groups. Table 3 shows the type of delivery at the end of the study in both groups. Results showed a statistically significant difference between groups in terms of delivery type (p<0.05).
The risk difference 95% CI of elective C-section does not include the null value (RD=0), so the difference of elective C-section's prevalence between intervention and control groups is statistically significant. Also, the relative risk 95% CI of elective C-section in the intervention compared to control is between 0.42 and 0.002. Since the 95% CI does not include the null value (RR=1), the proportion of elective C-sections in the intervention group is statistically lower than the control group.
Table 1) Baseline characteristics of study participants in the intervention and control groups

Table 2) TPB variables’ mean in intervention and control groups at baseline and follow-up (Mean±SD)
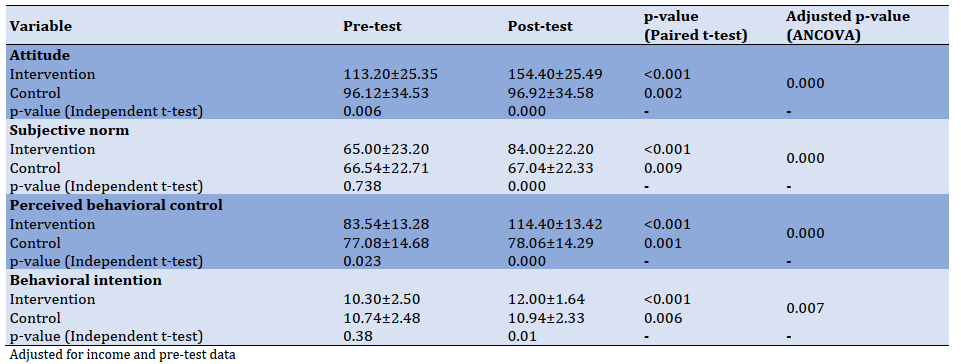
Table 3) Percentage of Natural childbirth, emergency C-section, elective C-section, relative risk and risk difference in intervention and control groups; X2=8.627, p-value=0.013, Phi Cramer's V=0.294

Discussion
It has been reported that CS rates higher than 10% were not associated with reductions in maternal and newborn mortality rates [24]. Thus the current study evaluated the effectiveness of education based on TPB on CS prevention. Results showed a significant difference for TPB's variables in the intervention group. We also had a slight increase in the mean of the TPB structures in the control group, but this increase was extremely low despite its significance. This slight increase in the control group could have been caused by the function of the health sector evolution plan (HSEP) of Iran to prevent elective cesarean section and a high correlation between pre & post-test data. On closer examination, the mean difference was calculated between two times for groups and then compared by the independent t-test. The results demonstrated a significant difference between the groups. In line with our studies of Shahraki-Sanavi et al. and Besharati et al. found that TPB-based interventions led to positive beliefs to NVD and choosing NVD more than CS [14, 15].
The study's findings showed that TPB-based intervention had a desirable impact on decreasing elective cesarean and consequently increasing NVD. The ratio of elective cesarean was also different between the groups, so that; elective CS was significantly lower in the intervention group than the control group (6% vs. 28%). A study in China showed a 35% decrease in elective CS among women who attended a prenatal education course [25]. Educational interventions for women in companion with their families have been proposed to increase NVD and decrease CS rates [26]. Our educational intervention included one friend or family member of the women to affect more some behavioral beliefs of women. Social desirability is the possible limitation that can affect the participants' responses—having the control group could somewhat control this problem.
Conclusion
This study could improve the outcome variables and NVD rates by providing education to women and their close friends or relatives during pregnancy.
Acknowledgments: We express our gratitude to the Deputy of Research at Ilam University of Medical Sciences and those who helped us conduct this study. We are grateful to the participants who participated in the study.
Ethical Permissions: The Ethics Committee of Ilam University of Medical Sciences confirmed the morality and ethics of the study Code: (EC Ref No: Ec/94/H/291).
Conflict of Interests: This article is a part of the result of an MSc thesis approved by the Ilam University of Medical Sciences.
Authors' Contributions: Authors' Contributions: Soheili B. (First author), Original researcher (30%); Mirzaei A. (Second author), Assistant researcher (10%); Sayehmiri K. (Third author), Statistical analyst (5%); Montazeri A. (Forth author), Methodologist (10%); Araban M. (Fifth author), Assistant researcher (10%); Ghazanfari Z. (Sixth author), Methodologist (35%).
Funding/Sources: No grant was received for this study.
Childbirth is a natural process. Monitoring and controlling natural delivery makes it possible to administer appropriate and timely treatment in cases of complications [1]. If natural childbirth is not viable, then cesarean section (CS) is suggested for the safety of mothers and babies. CS means surgical removal of the fetus from the abdomen and uterus walls [2]. However, in general, complications of elective cesarean section are more than normal delivery. Complications of CS delivery include bleeding, infection, maternal and infant mortality, postpartum depression, respiratory distress syndrome in infants, and higher economic cost for families [3-5].
The World Health Organization (WHO) has announced that 10-15% is an acceptable rate of CS for nulliparous women [6]. Despite this, the existing information shows that CS rates exceed this acceptable WHO standard in many countries [7]. In Iran, the rate is three times more than the global average [8].
Numerous factors may contribute to increased rates of CS. These include the socio-economic status of women, maternal age during the first pregnancy, doctor's concern regarding mother's conditions, legal matters, financial incentives, inadequate knowledge, negative attitudes of mothers towards vaginal childbirth, and mother's tendency to cesarean delivery [2, 9-13]. Thus, to evaluate how these factors could be influenced to reduce unnecessary cesarean delivery, some theory-based educational interventions are proposed [7]. One such intervention is educational programs using the Theory of Planned Behavior (TPB). For instance, studies conducted by Shahraki-Sanavi et al. [14], and Besharati et al. [15] demonstrated that such programs might be successful in changing women's attitudes normal delivery. However, more studies are needed to confirm these results.
While the WHO advocates no more than 10-15% rates for CS, a systematic review by studying 197514 pregnant women announced prevalence of CS in Iran equal to 48% that is much higher than its recommended levels [16, 17]. Some initiatives, including free-of-charge normal vaginal delivery (NVD), started on May 6, 2014, by the Iran Ministry of Health to limit CS and promote NVD. With the implementation in the ministry's approach, only a 6% increase in the percentage of NVD was achieved [18], and the rate of CS remains high. Therefore, interventions are needed to promote NVD to achieve WHO and ministry of health standard CS standards.
Considering the maternal and neonatal effects of CS [19, 20] and the WHO's recommendation on non-clinical interventions such as psychoeducation [21], the current study aims to evaluate the effect of theory-based health education on the prevention of elective cesarean sections among a sample of Iranian women referred to health care centers in Kermanshah.
Materials and Methods
This was a parallel randomized trial conducted on a sample of nulliparous pregnant women at the gestational age of 28-36 weeks, referred to health care centers in Kermanshah, a province in the west of Iran. The study flowchart is also presented in Diagram 1.
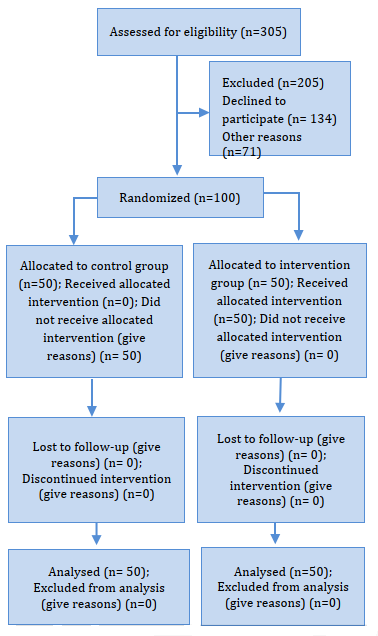
Figure 1) Flow diagram of the study participants
The study sample, which began in December 2015 and ended in October 2016, was taken from eight health care centers. The health centers were initially selected through the roll of a die. Four centers were allocated as the intervention group and four as the control group in a randomized manner. Health care centers, which formed the framework for selecting participants in intervention and control groups, were the same regarding economic, social, and cultural conditions.
Inclusion criteria were as follows: being nulliparous at the gestational age range of 28-36 weeks; and age between 18-35. Exclusion criteria included contraindication to NVD, premature childbirth, incomplete questionnaire, and absence from training sessions.
The intervention consisted of three training sessions in 2 weeks. The first session was held to provide a favorable attitude towards natural childbirth. The explanations about delivery methods, cesarean section indications, the advantages and disadvantages of each method were presented for pregnant women with the lecture method in one hour. Then they were asked to express their opinions, beliefs, and concerns about the issue in a group discussion session which lasted for one hour and a half.
The subject of the second session was to learn feasible methods for pain reduction to enhance mothers' perception of behavioral control. In this session, they helped learn breathing and relaxation techniques and master it through practical exercises. This session also lasted for one hour and thirteen minutes.
In order to influence perceived behavioral control, Training pain relief techniques such as deep breathing, relaxation, and the massage was done in two 90-minute sessions. The researcher taught these techniques, and then the group practiced them to learn them.
In order to affect subjective norms, pregnant women were asked to attend a meeting with a friend or family member. Participating in training sessions with friends or family members who have a major role in their decision-making was a technique to affect their subjective norms. A pamphlet was designed to help women were attending sessions alone. These people could support and reinforce them to select natural childbirth.
In each session, a time is specified to review the content and answer their questions. The control group received only standard care led by midwives at health care centers. Standard care included examinations of maternal weight, fundal height, FHR auscultation, education and screening for alarm signs in late pregnancy, and education about delivery and infant care were provided to women. Data on variables of TPB were gathered at baseline and 1-month follow-up. In order to find their delivery method, each mother also received a phone call after childbirth to record their delivery method.
The data collection instrument involved a two-section questionnaire including 50 items. The first section had 9 items related to demographic and obstetric questions. The second section included questions related to TPB's variables. This section included attitude with 8 questions (behavioral beliefs: 8Q, outcome evaluation: 8Q), subjective norms with 5 questions (normative beliefs: 5Q, motivations to comply: 5Q), perceived behavioral
control with 6 questions (control beliefs: 6Q, perceived power: 6Q), and behavioral intention with 3 Questions. The answers to the questions of this part were set on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree) . The possible range of scores was 8 to 200 for attitude, 5 to 125 for subjective norms, 6 to 150 for perceived behavioral control, and 3 to 15 for behavioral intention. The scoring was set as Ajzen's TPB questionnaire construction [22].
Content validity was evaluated based on experts' comments, and essential modifications were made. Reliability was also evaluated by Cronbach's alpha. The Cronbach coefficient was 0.82 for attitude, 0.77 for subjective norm, 0.70 for perceived behavioral control, and 0.84 for behavioral intention. Answering each questionnaire by the researcher required 10 to 15 minutes through an interview. This process was done two times, before and after the intervention.
A sample of 43 pregnant women was estimated per each group, according to the percent of elective C-section in intervention and control group as 6% and 28%, alpha and beta errors equal to 0.05 and 0.1 using the following statistical formula [23]:
To increase the power of the test to 86%, the sample size was increased to 50 in each group.
Data were analyzed by SPSS software. The normal distribution of data was controlled by the Kolmogorov-Smirnov test. To compare demographic data of the intervention and control groups before the intervention, the independent t-test and chi-square were applied. Paired t-test was used to compare the pre-test and post-test scores of attitude, subjective norms, perceived behavioral control, and behavioral intention in each group. Due to the difference between groups in terms of income, the analysis of covariance test was used to adjust income variable and pre-test data. Finally, a comparison of the type of delivery (including NVD, emergency cesarean section, and elective cesarean section) was done using the Chi-square test between groups.
Approval for this research was acquired through Ilam University of Medical Sciences Ethics Committee (EC Ref No: Ec/94/H/291). Objectives of the study were outlined at the beginning of the study. Written informed consent was obtained from participants, confidentiality of information was ensured, and participants were given authority to withdraw from the study if they were exposed to problems that might have hindered their participation.
Findings
In this work, 100 pregnant women have participated. Mean±SD for the women's age was 22.78±3.68 years. There was no significant difference between the two groups in terms of age, job and education status of women and their spouse, and planned pregnancy (p>0.05), but there was a significant difference between groups in terms of income (p<0.05; Table 1).
Table 2 shows the mean scores of outcome variables for the intervention and control groups at baseline and one-month follow-up. Results showed significant differences at follow-up for the mean scores of attitude, subjective norms, perceived behavioral control (p≤0.001), and behavioral intention (p≤0.01) between groups. Table 3 shows the type of delivery at the end of the study in both groups. Results showed a statistically significant difference between groups in terms of delivery type (p<0.05).
The risk difference 95% CI of elective C-section does not include the null value (RD=0), so the difference of elective C-section's prevalence between intervention and control groups is statistically significant. Also, the relative risk 95% CI of elective C-section in the intervention compared to control is between 0.42 and 0.002. Since the 95% CI does not include the null value (RR=1), the proportion of elective C-sections in the intervention group is statistically lower than the control group.
Table 1) Baseline characteristics of study participants in the intervention and control groups

Table 2) TPB variables’ mean in intervention and control groups at baseline and follow-up (Mean±SD)
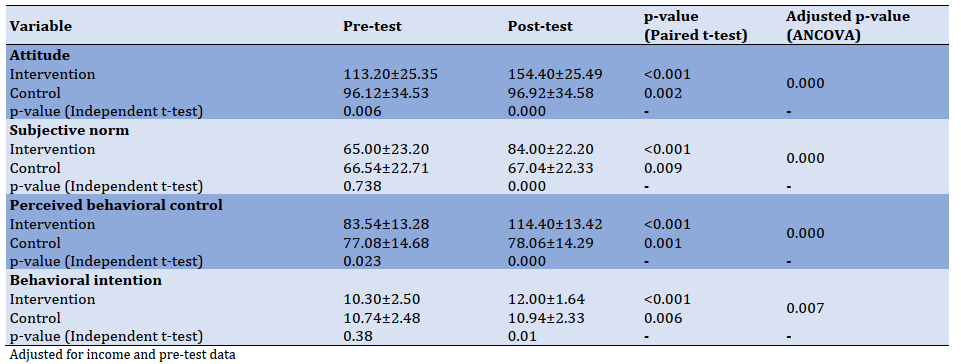
Table 3) Percentage of Natural childbirth, emergency C-section, elective C-section, relative risk and risk difference in intervention and control groups; X2=8.627, p-value=0.013, Phi Cramer's V=0.294

Discussion
It has been reported that CS rates higher than 10% were not associated with reductions in maternal and newborn mortality rates [24]. Thus the current study evaluated the effectiveness of education based on TPB on CS prevention. Results showed a significant difference for TPB's variables in the intervention group. We also had a slight increase in the mean of the TPB structures in the control group, but this increase was extremely low despite its significance. This slight increase in the control group could have been caused by the function of the health sector evolution plan (HSEP) of Iran to prevent elective cesarean section and a high correlation between pre & post-test data. On closer examination, the mean difference was calculated between two times for groups and then compared by the independent t-test. The results demonstrated a significant difference between the groups. In line with our studies of Shahraki-Sanavi et al. and Besharati et al. found that TPB-based interventions led to positive beliefs to NVD and choosing NVD more than CS [14, 15].
The study's findings showed that TPB-based intervention had a desirable impact on decreasing elective cesarean and consequently increasing NVD. The ratio of elective cesarean was also different between the groups, so that; elective CS was significantly lower in the intervention group than the control group (6% vs. 28%). A study in China showed a 35% decrease in elective CS among women who attended a prenatal education course [25]. Educational interventions for women in companion with their families have been proposed to increase NVD and decrease CS rates [26]. Our educational intervention included one friend or family member of the women to affect more some behavioral beliefs of women. Social desirability is the possible limitation that can affect the participants' responses—having the control group could somewhat control this problem.
Conclusion
This study could improve the outcome variables and NVD rates by providing education to women and their close friends or relatives during pregnancy.
Acknowledgments: We express our gratitude to the Deputy of Research at Ilam University of Medical Sciences and those who helped us conduct this study. We are grateful to the participants who participated in the study.
Ethical Permissions: The Ethics Committee of Ilam University of Medical Sciences confirmed the morality and ethics of the study Code: (EC Ref No: Ec/94/H/291).
Conflict of Interests: This article is a part of the result of an MSc thesis approved by the Ilam University of Medical Sciences.
Authors' Contributions: Authors' Contributions: Soheili B. (First author), Original researcher (30%); Mirzaei A. (Second author), Assistant researcher (10%); Sayehmiri K. (Third author), Statistical analyst (5%); Montazeri A. (Forth author), Methodologist (10%); Araban M. (Fifth author), Assistant researcher (10%); Ghazanfari Z. (Sixth author), Methodologist (35%).
Funding/Sources: No grant was received for this study.
Article Type: Original Research |
Subject:
Health Education and Health Behavior
Received: 2020/12/2 | Accepted: 2021/01/20 | Published: 2021/05/10
Received: 2020/12/2 | Accepted: 2021/01/20 | Published: 2021/05/10
References
1. Sharifirad G, Rezaeian M, Soltani R, Javaheri S, Amidi Mazaheri M. A survey on the effects of husbands' education of pregnant women on knowledge, attitude, and reducing elective cesarean section. J Educ Health Promot. 2013;2:50. [Link] [DOI:10.4103/2277-9531.119036] [PMID] [PMCID]
2. Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap LC, Wenstrom KD. Williams obstetrics. 22nd Edition. New York: McGraw Hill; 2005. [Link]
3. Feng XL, Wang Y, An L, Ronsmans C. Cesarean section in the people's Republic of China: Current perspectives. Int J Womens Health. 2014;6:59-74. [Link] [DOI:10.2147/IJWH.S41410] [PMID] [PMCID]
4. Mishanina E, Rogozinska E, Thatthi T, Uddin-Khan R, Khan KS, Meads C. Use of labour induction and risk of cesarean delivery: A systematic review and meta-analysis. CMAJ. 2014;186(9):665-73. [Link] [DOI:10.1503/cmaj.130925] [PMID] [PMCID]
5. Baghianimoghadam MH, Hashemifard T, Jafari S, Yadolahi P, Kamali moradzadah M, Hashemifard F. The effect of educational intervention on selection of delivery method based on health belief model. J Commun Health Res. 2014;3(2):115-23. [Persian] [Link]
6. Gibbons L, Belizán JM, Lauer JA, Betrán AP, Merialdi M, Althabe F. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: Overuse as a barrier to universal coverage [Report]. Geneva: World Health Organization; 2010. [Link]
7. Kulkarni A, Wright E, Kingdom J. Web-based education and attitude to delivery by caesarean section in nulliparous women. J Obstet Gynaecol Can. 2014;36(9):768-75. [Link] [DOI:10.1016/S1701-2163(15)30478-3]
8. Karami Matin B, Ataee M, Mirzaei_Alavijeh M, Mahboubi M, Aghaei A, Mohammadi P. Cognitive Factors related to cesarean intention among Iranian pregnant women. J Biol Todays World. 2014;3(11):251-55. [Link] [DOI:10.15412/J.JBTW.01031105]
9. Klein MC. Obstetrician's fear of childbirth: How did it happen?. Birth. 2005;32(3):207-9. [Link] [DOI:10.1111/j.0730-7659.2005.00371.x] [PMID]
10. Gamble J, Creedy DK, McCourt C, Weaver J, Beake S. A critique of the literature on women's request for cesarean section. Birth. 2007;34(4):331-40. [Link] [DOI:10.1111/j.1523-536X.2007.00193.x] [PMID]
11. Stoll K, Fairbrother N, Carty E, Jordan N, Miceli C, Vostrcil Y, et al. "It's all the rage these days": University students' attitudes toward vaginal and cesarean birth. Birth. 2009;36(2):133-40. [Link] [DOI:10.1111/j.1523-536X.2009.00310.x] [PMID]
12. Nilstun T, Habiba M, Lingman G, Saracci R, Da Frè M, Cuttini M. Cesarean delivery on maternal request: Can the ethical problem be solved by the principlist approach?. BMC Med Ethics. 2008;9:11. [Link] [DOI:10.1186/1472-6939-9-11] [PMID] [PMCID]
13. Yazdizadeh B, Nedjat S, Mohammad K, Rashidian A, Changizi N, Majdzadeh R. Cesarean section rate in Iran, multidimensional approaches for behavioral change of providers: A qualitative study. BMC Health Serv Res. 2011;11:159-73. [Link] [DOI:10.1186/1472-6963-11-159] [PMID] [PMCID]
14. Shahhraki Sanavi F, Ansari-Moghaddam A, Faraji Shovey M, Rakhshani F. Effective education to decrease elective caesarean section. J Park Med Assoc. 2014;64(5):500-5. [Link]
15. Besharati F, Hazavehei SMM, Moeini B, Moghimbeigi A. Effect of educational interventions based on theory of planned behavior (TPB) in selecting delivery mode among pregnant women referred to Rasht health centers. J Adv Med Biomed Res. 2011;19(77):94-106. [Link]
16. Rafiei M, Saei Ghare M, Akbari M, Kiani F, Sayehmiri F, Sayehmiri K, et al. Prevalence, causes, and complications of cesarean delivery in Iran: A systematic review and meta-analysis. Int J Reprod Biomed. 2018;16(4):221-34. [Link]
17. Rasoli M, Mirrezaie SM, Fooladi E, Zarouj Hosseini R, Fayaz M. Effects of reviewing childbirth scenarios on choice of delivery type: A randomized controlled trial. Turk J Obstet Gynecol. 2019;16(1):15-22. [Link] [DOI:10.4274/tjod.galenos.2019.92260] [PMID] [PMCID]
18. Ghanbari A, Moaddab F, Heyddarzade A, Jafaraghaee F, Barari F. Health system evolution plan; a new approach to health care delivery: the challenge ahead. HAKIM Res J. 2017;20(1):1-8. [Link]
19. Betran AP, Torloni MR, Zhang JJ, Gülmezoglu AM, WHO Working Group on Caesarean Section. WHO statement on caesarean section rates. BJOG. 2016;123(5):667-70. [Link] [DOI:10.1111/1471-0528.13526] [PMID] [PMCID]
20. Pilar Betran A, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015;12:57. [Link] [DOI:10.1186/s12978-015-0043-6] [PMID] [PMCID]
21. World Health Organization. WHO recommendations on non-clinical interventions to reduce unnecessary caesarean sections. Geneva: World Health Organization; 2018. [Link]
22. Ajzen I. Constructing a theory of planned behavior questionnaire. Unknown Publisher; 2019. [Link]
23. Sayehmiri K. Applied biostatistics and method of research. 5th Edition. Ilam: Ilam University of Medical Sciences; 2020. [Persian] [Link]
24. Ye J, Zhang J, Mikolajczyk R, Torloni MR, Gülmezoglu AM, Betran AP. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: A worldwide population-based ecological study with longitudinal data. BJOG. 2016;123(5):745-53. [Link] [DOI:10.1111/1471-0528.13592] [PMID] [PMCID]
25. Gao Y, Tang Y, Tong M, Du Y, Chen Q. Does attendance of a prenatal education course reduce rates of caesarean section on maternal request? A questionnaire study in a tertiary women hospital in Shanghai, China. BMJ Open. 2019;9(6):e029437. [Link] [DOI:10.1136/bmjopen-2019-029437] [PMID] [PMCID]
26. Pilar Betrán A, Temmerman M, Kingdon C, Mohiddin A, Opiyo N, Torloni MR, et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet. 2018;392(10155):1358-68. [Link] [DOI:10.1016/S0140-6736(18)31927-5]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |